Skin Moisturizing Effects of Panthenol-Based Formulations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Cosmeceutical Products List
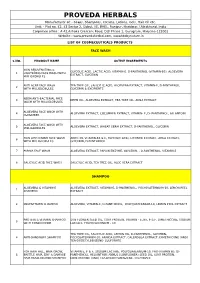
PROVEDA HERBALS Manufacturer of: - Soaps, Shampoos, Creams, Lotions, Gels, Hair Oil etc. Unit: - Plot no. 42, 43 Sector 2, Sidcul, IIE, BHEL, Ranipur, Haridwar, Uttrakhand, India Corporate office : A 42,Ashoka Crescent Road, DLF Phase 1, Gurugram, Haryana-122002 Website : www.provedaherbal.com, www.tbcbynature.in LIST OF COSMECEUTICALS PRODUCTS FACE WASH S.NO. PRODUCT NAME ACTIVE INGREDIENTS SKIN REJUVENATING & GLYCOLIC ACID, LACTIC ACID, VITAMIN-E, D-PANTHENOL (VITAMIN-B5), ALOEVERA 1 LIGHTENING FACE WASH WITH EXTRACT, GLYCERIN MILLIGLOBULES ANTI ACNE FACE WASH TEA TREE OIL, SALICYLIC ACID, ALOEVERA EXTRACT, VITAMIN-E, D-PANTHENOL, 2 WITH MILLIGLOBULES GLYCERIN & EXCIPIENTS NEEM ANTI-BACTERIAL FACE 3 NEEM OIL, ALOEVERA EXTRACT, TEA TREE OIL, AMLA EXTRACT WASH WITH MILLIGLOBULES ALOEVERA FACE WASH WITH 4 ALOEVERA EXTRACT, CUCUMBER EXTRACT, VITAMIN- E, D- PANTHENOL, ALLANTOIN CUCUMBER ALOEVERA FACE WASH WITH 5 ALOEVERA EXTRACT, WHEAT GERM EXTRACT, D-PANTHENOL, GLYCERIN MILLIGLOBULES SKIN LIGHTENING FACE WASH ARBUTIN, VITAMIN-B3 & E, GLYCOLIC ACID, LICORICE EXTRACT, AMLA EXTRACT, 6 WITH MILLIGLOBULES GLYCERIN, D-PANTHENOL 7 PAPAYA FACE WASH ALOEVERA EXTRACT, PAPAIN ENZYME, GLYCERIN, , D-PANTHENOL, VITAMIN-E 8 SALICYLIC ACID FACE WASH SALICYLIC ACID, TEA TREE OIL, ALOE VERA EXTRACT SHAMPOO ALOEVERA & VITAMIN-E ALOEVERA EXTRACT, VITAMIN-E, D-PANTHENOL, POLYQUATERNIUM-10, LEMON PEEL 1 SHAMPOO EXTRACT 2 MULTIVITAMIN SHAMPOO ALOEVERA, VITAMIN-E, D-PANTHENOL, POLYQUATERNIUM-10, LEMON PEEL EXTRACT PROTEIN & VITAMIN SHAMPOO SUN FLOWER SEED OIL, -

National OTC Medicines List
National OTC Medicines List ‐ DraŌ 01 DRAFT National OTC Medicines List Draft 01 Ministry of Public Health of Lebanon This list was prepared under the guidance of His Excellency Minister Waêl Abou Faour andDRAFT the supervision of the Director General Dr. Walid Ammar. Editors Rita KARAM, Pharm D. PhD. Myriam WATFA, Pharm D Ghassan HAMADEH, MD.CPE FOREWORD According to the French National Agency for Medicines and Health Products Safety (ANSM), Over-the-counter (OTC) drugs are medicines that are accessible to patients in pharmacies, based on criteria set to safeguard patients’ safety. Due to their therapeutic class, these medicines could be dispensed without physician’s intervention for diagnostic, treatment initiation or maintenance purposes. Moreover, their dosage, treatment period and Package Insert Leaflet should be suitable for OTC classification. The packaging size should be in accordance with the dosage and treatment period. According to ArticleDRAFT 43 of the Law No.367 issued in 1994 related to the pharmacy practice, and the amendment of Articles 46 and 47 by Law No.91 issued in 2010, pharmacists do not have the right to dispense any medicine that is not requested by a unified prescription, unless the medicine is mentioned in a list which is established by pharmacists and physicians’ syndicates. In this regard, the Ministry of Public Health (MoPH) developed the National OTC Medicines List, and presentedit in a scientific, objective, reliable, and accessible listing. The OTC List was developed by a team of pharmacists and physicians from the Ministry of Public Health (MoPH). In order to ensure a safe and effective self- medicationat the pharmacy level, several pharmaceutical categories (e.g. -

Safety Assessment of Panthenol, Pantothenic Acid, and Derivatives As Used in Cosmetics
Safety Assessment of Panthenol, Pantothenic Acid, and Derivatives as Used in Cosmetics Status: Scientific Literature Review for Public Comment Release Date: February 2, 2017 Panel Meeting Date: April 10-11, 2017 All interested persons are provided 60 days from the above date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Director, Dr. Lillian J. Gill. The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D., Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Director is Lillian J. Gill, D.P.A. This safety assessment was prepared by Laura N. Scott, Scientific Writer/Analyst. © Cosmetic Ingredient Review 1620 L Street, NW, Suite 1200 ♢ Washington, DC 20036-4702 ♢ ph 202.331.0651 ♢ fax 202.331.0088 ♢ [email protected] INTRODUCTION This assessment reviews the safety of Panthenol, Pantothenic Acid and 5 of their derivatives as used in cosmetic formulations. -

Dietary Supplements Compendium Volume 1
2015 Dietary Supplements Compendium DSC Volume 1 General Notices and Requirements USP–NF General Chapters USP–NF Dietary Supplement Monographs USP–NF Excipient Monographs FCC General Provisions FCC Monographs FCC Identity Standards FCC Appendices Reagents, Indicators, and Solutions Reference Tables DSC217M_DSCVol1_Title_2015-01_V3.indd 1 2/2/15 12:18 PM 2 Notice and Warning Concerning U.S. Patent or Trademark Rights The inclusion in the USP Dietary Supplements Compendium of a monograph on any dietary supplement in respect to which patent or trademark rights may exist shall not be deemed, and is not intended as, a grant of, or authority to exercise, any right or privilege protected by such patent or trademark. All such rights and privileges are vested in the patent or trademark owner, and no other person may exercise the same without express permission, authority, or license secured from such patent or trademark owner. Concerning Use of the USP Dietary Supplements Compendium Attention is called to the fact that USP Dietary Supplements Compendium text is fully copyrighted. Authors and others wishing to use portions of the text should request permission to do so from the Legal Department of the United States Pharmacopeial Convention. Copyright © 2015 The United States Pharmacopeial Convention ISBN: 978-1-936424-41-2 12601 Twinbrook Parkway, Rockville, MD 20852 All rights reserved. DSC Contents iii Contents USP Dietary Supplements Compendium Volume 1 Volume 2 Members . v. Preface . v Mission and Preface . 1 Dietary Supplements Admission Evaluations . 1. General Notices and Requirements . 9 USP Dietary Supplement Verification Program . .205 USP–NF General Chapters . 25 Dietary Supplements Regulatory USP–NF Dietary Supplement Monographs . -

PRODUCT GUIDE P4
O HE U T T E R G D O O Back to basics Simplicity Effective PRODUCT GUIDE p4. Philosophy.................................The Outer Good p5. Cleanse .........................................Silk / Bubble p6. Balance ..........................................Restore / Revive p7. Smooth ..........................................Exfoliant p8. Treat..................................................Bright / Clear / Calm / Lift / Plump p10. Nourish .........................................Vitamin Energiser / Intense Collagen Repair / Daily Benefit Contents p12. Transform ...................................Eyes p13. Pamper / Condition .......Super Boost / Velvet p14. Body .................................................Body Milk / Face and Body Oil p15. Active Ingredients THE OUTER GOOD - PRODUCT GUIDE 3 Cleansing is the foundation for healthy skin, the most important step, so often overlooked, rushed and seen as a chore. Consider everything you put on your face each day, the onslaught of pollutants and daily impurities, skin needs to breathe. We need to help our skin help itself by removing congestion, enabling the safe passage of targeted active ingredients. AM: Cleanse to remove products from the evening before, sweat and slough off the night’s repair. PM: Double cleansing in the evening is key. The first cleanse helps dissolve and loosen makeup, SPF, dirt and impurities. Cleanse 2 washes any last traces away. Philosophy Silk Bubble Your skin is precious. It is our largest, living, breathing At The Outer Good, our philosophy is simple, treat -

LYSOVIT® (B-Complex+Lysine)
Lysovit/LPD/PK-02 LYSOVIT® (B-Complex+Lysine) 1. NAME OF THE MEDICINAL PRODUCT LYSOVIT® 2. QUALITATIVE AND QUANTITATIVE COMPOSITION LYSOVIT® Syrup 120 ml Description Each 5 ml contains: Thiamine HCl 4.16 mg Riboflavin USP 1.66 mg Pyridoxine HCl 1 mg Niacinamide USP 18 mg D-Panthenol USP 2.5 mg Cyanocobalamin USP 8.33 mcg Ascorbic Acid USP 75 mg Inositol USP 5 mg Lysine Monohydrochloride USP 33.33 mg 3. PHARMACEUTICAL FORM Syrup 4. CLINICAL PARTICULARS 4.1. THERAPEUTIC INDICATIONS 1. For maintenance of health and to meet the extra energy needs of growing children. 2. Increases appetite and helps in recovery from illnesses. 4.2. POSOLOGY AND METHOD OF ADMINISTRATION Children: 1 teaspoonful daily or as prescribed by the physician Adults: One to two teaspoonsful daily. Shake well before use. Thiamine Benefits: Thiamine is recommended for digestive problems including poor appetite, ulcerative colitis, and ongoing diarrhea. People take thiamine for conditions related to low levels of thiamine (thiamine deficiency syndromes), including beriberi and inflammation of the nerves (neuritis) associated with pellagra or pregnancy.4 1 Lysovit/LPD/PK-02 Thiamine - Daily Recommended Dietary Allowance (RDA): In adults, 1-2 mg of thiamine per day is commonly used. Infants 0-6 months, 0.2 mg Infants 7-12 months, 0.3 mg Children 1-3 years, 0.5 mg Children 4-8 years, 0.6 mg Boys 9-13 years, 0.9 mg Men 14 years and older, 1.2 mg4 Girls 9-13 years, 0.9 mg Women 14-18 years, 1 mg Women over 18 years, 1.1 mg Pregnant women, 1.4 mg Breast-feeding women, 1.5 mg Riboflavin Benefits: Riboflavin had a direct impact on maintenance of good brain function. -

Capillary Treatments 24 Capillary Treatments
capillary treatments 24 capillary treatments PRODUCT INCI NAME USAGE TOCOPHERYL ACETATE, RETINYL PALMITATE, A+B5+B8+E+F VITAMIN ETHYL LINOLEATE, ETHYL Intended for hair care. COMPLEX LINOLENATE, PANTHENOL, INOSITOL, ETHYL OLEATE CHOLECALCIFEROL, TOCOPHERYL ACETATE, ETHYL LINOLEATE, A+D+E+F VITAMIN COMPLEX Treatments intended for hair care and restoring. RETINYL PALMITATE, ETHYL LINOLENATE, ETHYL OLEATE SODIUM SULFITE, HYDROLYZED COLLAGEN, ALISARINE BASIC Straightener hair complex, fine or porous hair. UREA, HYDROLYZED KERATIN SODIUM SULFITE, THIOGLYCOLIC ACID, AMMONIUM HYDROXIDE, ALISARINE MAX Straightener hair complex, difficult or very strong hair. UREA, HYDROLYZED KERATIN, HYDROLYZED COLLAGEN SODIUM SULFITE, UREA, HYDROLYZED KERATIN, HYDROLYZED COLLAGEN, ALISARINE PLUS Straightener hair complex, normal or strong hair. IMIDAZOLIDINYL UREA, DIAZOLIDINYL UREA, FORMALDEHYDE UNDECYLENAMIDE DEA, FAEX EXTRACT, PIROCTONE OLAMINE, NIACINAMIDE, ANTI-DANDRUFF COMPLEX PANTHENOL, RIBOFLAVIN, Anti-dandruff. THIAMINE HCL, PYRIDOXINE HCL, BIOTIN, INOSITOL, CYANOCOBALAMIN FAEX EXTRACT, TOCOPHERYL ACETATE, RETINYL PALMITATE, TIOXOLONE, NIACINAMIDE, ANTI-GREASE COMPLEX PANTHENOL, RIBOFLAVIN, Anti-grease. PYRIDOXINE HCL, INOSITOL, BIOTIN, THIAMINE HCL, CYANOCOBALAMIN POLYSORBATE 80, ANTI-PRURITIC AND SORBITAN OLEATE, OLEA Dermo-protecting, softening and calming. It protects the scalp against irritations ANTIIRRITANT CAPILLARY EUROPAEA LEAF EXTRACT, and itches. COMPLEX MENTHA PIPERITA EXTRACT 25 capillary treatments PRODUCT INCI NAME USAGE HYDROLYZED SERUM -

Active Pharmaceutical Ingredients (Apis)
YOUR ENDTOEND PARTNER YOUR ENDTOEND PARTNER PRODUCTS CUSTOMIZED SOLUTIONS EXPERT SERVICES PRODUCTS CUSTOMIZED SOLUTIONS EXPERT SERVICES YOUR ENDTOEND PARTNER YOUR ENDTOEND PARTNER PRODUCTS CUSTOMIZED SOLUTIONS EXPERT SERVICES PRODUCTS CUSTOMIZED SOLUTIONS EXPERT SERVICES YOUR ENDTOEND PARTNER YOUR ENDTOEND PARTNER PRODUCTS CUSTOMIZED SOLUTIONS EXPERT SERVICES PRODUCTS CUSTOMIZED SOLUTIONS EXPERT SERVICES PRODUCTS WITH PURPOSE Active Pharmaceutical YOUR ENDTOEND PARTNER YOUR ENDTOEND PARTNER IngredientsPRODUCTS CUSTOMIZED SOLUTIONS (APIs)EXPERT SERVICES PRODUCTS CUSTOMIZED SOLUTIONS EXPERT SERVICES Product code Product Product code Product Product code Product 50 1627 9 Vitamin B12 0.1% WS Ph5 Vitamin A Vitamin B2 04 2915 5 Vitamin B12 Crystalline 04 2187 1 Dry Vitamin A Palmitate, Type 250 CWS/F 50 1626 1 Riboflavin 5’-Phosphate Ph (tocopherol) 50 1630 0 Vitamin B12 Crystalline Ph4 04 7040 6 Riboflavin Universal 04 2401 3 Vitamin A Palmitate 1.7 MIU/g (BHA/BHT) Vitamin C 04 2400 5 Vitamin A Palmitate 1.7 MIU/g2 Vitamin B3 04 0809 3 Ascorbic Acid Fine Granular 50 1626 2 Retinyl Palmitate 1.7 MIU/g Ph1, 3 04 8784 8 Niacinamide 04 2246 0 Ascorbic Acid Fine Powder2 50 1227 9 Dry Vitamin A Acetate 500 B 50 1629 1 Niacinamide Ph3, 4 50 1645 0 Ascorbic Acid Fine Powder Ph1, 3 Vitamin E Vitamin B5 50 1625 5 Ascorbic Acid Ph 50 0112 9 Dry Vitamin E 50% CWS/S 04 1267 8 Calcium D-Pantothenate 04 1944 3 Calcium Ascorbate 04 2008 5 dl-alpha-Tocopheryl Acetate2 04 1385 2 D-Panthenol2 50 1625 6 Sodium Ascorbate Ph 50 1626 0 dl-a-Tocopheryl Acetate Ph1, -
Hazard Classification: Non Hazardous As Defined by 29CFR Part 1910.1200 (Special Chemical Identification: Common Name)
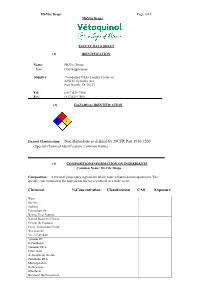
Hi-Vite Drops Page 1of 5 Hi-Vite Drops SAFETY DATA SHEET (1) IDENTIFICATION Name: Hi-Vite Drops Use: Oral Supplement Supplier: Vetoquinol USA (Tomlyn Products) 4250 N. Sylvania Ave Fort Worth, TX 76137 Tel: ( 817)529-7500 Fax: (817)529-7506 (2) HAZARD(S) IDENTIFICATION Hazard Classification: Non Hazardous as defined by 29CFR Part 1910.1200 (Special Chemical Identification: Common Name) (3) COMPOSITION/INFORMATION ON INGREDIENTS Common Name: Hi-Vite Drops Composition: A blend of proprietary ingredients which make a flavored oral supplement. The specific concentration of the ingredients has been withheld as a trade secret. Chemical %Concentration Classification CAS Exposure Water Sucrose Sorbital Polysorbate 80 Bovine Liver Peptone Natural Roast beef Flavor Gelatin By Products Ferric Ammonium Citrate Niacinamide Vit. A Palmitate Vitamin D3 D-Panthenol Thiamine HCL Citirc Acid A-Tocopheryl Acetate Pyridoxine HCL Methylparaben Na Benzoate Riboflavin Butylated Hydroxyanisol Menadione Cyanocobolamine Hi-Vite Drops Page 2of 5 (4) FIRST AID MEASURES Exposure Route Symptom Treatment INHALATION N/A N/A SKIN CONTACT N?A N/A EYE CONTACT May irritate eyes if exposure occurs Rinse with cool fresh water for 10 minutes. If irritation persists seek medical attention If ingestion Occurs please call a physician INGESTION Ingestion may cause an allergic reaction in and or certain individuals. poison control (5) FIRE-FIGHTING MEASURES Suitable Extinguisher: FOAM, DRY POWDER, WATER, CO2 Special Precautions: None Special Protective Equipment: None (6) ACCIDENTAL RELEASE PROCEDURES Personal Precautions: None. Environmental precautions: do not freeze or expose to heat Methods for Cleaning up: None Hi-Vite Drops Page 3 of 5 (7) HANDLING AND STORING Precautions during handling: keep from freezing. -

Comparative Efficacy of Grotto Cream with Fucidin Cream on Normal and Diabetic Wound Models in Rats
80IndianBanna, J Physiol Zorba, Pharmacol Hossny and 2018; Kamel 62(1) : 80–86 Indian J Physiol Pharmacol 2018; 62(1) Original Article Comparative Efficacy of Grotto Cream with Fucidin Cream on Normal and Diabetic Wound Models in Rats H. A. El Banna1*, H. El Zorba1, A. Hossny2 and W. Kamel3 1 Department of Pharmacology, Faculty of Veterinary Medicine Cairo University, Giza 12211, Egypt 2 Studant, Hospital of Cairo University 3 Animal Health Research Institute, Dokki, Egypt Abstract Wound healing is a process of well-recognized orchestrated and predictable events, in which there are four distinct inter-related phases: haemostasis, inflammation, proliferation and remodeling. The present study was carried out to evaluate comparative efficacy of Grotto cream (combination composed of, bees wax, D- panthenol, Lavender oil, glycerin, Vitamin E, allantoin and dimethicone) with fucidin cream in normal and diabetic rats. Circular wound was excised on the dorsal side of each rat either control healthy or diabetics rats. Grotto cream or fucidin cream were topically applied to the wounds on alternating days for 21 days in normal rats and 30 days in diabetic ones. Streptozotocin (50 mg/kg b.wt) single intra-peritoneal injection was used to induced diabetic rat model. Wound contraction and epithelialization period were measured following excision wound model and were used to evaluate wound healing effect of either Grotto or fucidin cream. The obtained results indicated that topical application of Grotto creams accelerated wound healing when compared to control non treated rats. The rate of wound contraction was significantly increased on days 3–21 for normal rats and days 3 to 30 for diabetic rats in Grotto and fucidin creams treated animals respectively. -

Gentle Hydra-Cleanse with Hyaluronic Acid
GENTLE HYDRA-CLEANSE WITH HYALURONIC ACID No Parabens, Sulfates or Phthalates. Cruelty-Free, Vegan Friendly & Gluten-Free SKIN TYPE: ALL / SENSITIVE / ROSACEA / POST-OP pH: 5.89 PRODUCT DESCRIPTION: This sulfate-free, daily micro-foaming cleanser thoroughly cleanses the skin to gently remove surface impurities and soothe redness without stripping the skin of essential oils. Gentle enough for the most sensitive and post-procedure skin, this formula combines the nutritive benefits of soothing Cucumber Extract, healing Calendula Extract and deeply hydrating Hyaluronic Acid to rebalance and calm the skin, leaving it remarkably moist and supple. Added Vitamin B5 promotes the formation of new, healthy skin cells to aid in skin repair while also providing anti- inflammatory benefits. Excellent for all skin types. CLIENT USE: Moisten skin with lukewarm water. Lather cleanser in hands and massage into skin. Rinse thoroughly. PROFESSIONAL USE: Moisten skin with sponges and apply a small amount of cleanser to skin. Massage in gentle, circular motions, gradually adding more water. Remove thoroughly with warm, moist sponges. PRODUCT INGREDIENTS: Water/Aqua/Eau, Sodium Cocoyl Isethionate, Cocamidopropyl Hydroxysultaine, Cocamidopropyl Betaine, Sodium Methyl Cocoyl Taurate, PEG-7 Glyceryl Cocoate, Acrylates Copolymer, Glycol Distearate, Disodium EDTA, Sodium Hyaluronate, Tocopheryl Acetate, Panthenol, Cucumis Sativus (Cucumber) Fruit Extract, Calendula Officinalis (Calendula) Flower Extract, Simmondsia Chinensis (Jojoba) Seed Oil, Sodium Lauroyl Sarcosinate, Guar Hydroxypropyltrimonium Chloride, Citric Acid, Methylisothiazolinone, Dimethicone, Phenoxyethanol. HIGHLIGHT INGREDIENTS: Sodium Hyaluronate (Hyaluronic Acid): Special combination of high- and low-weight hyaluronic acids that expand once in the skin to provide excellent, long-lasting hydration. A glycosaminoglycan capable of binding 1,800 times it’s weight in water, when applied to the skin it forms a water-binding barrier allowing for increased moisture retention in the skin’s intracellular matrix. -

No Poo Beard Cleanser
No Poo Beard Cleanser This No Poo Beard Cleanser is designed for men taking care about their beard on a daily basis. Biovitrient 124 is a rich blend of plant extracts reaching the hair follicles in the skin via blood stream and offers a healthy looking beard. Biovitrient 125 also contains a rich blend of plant extracts as well as Provitamin B5, Biotin and Niacin, which enhance hair growth. The blend also provides moisturizing, emollients, filmogenic protection. Sil-O-San 8611 C supports foaming, it produces a dense foam, and provides good distribution and spreading. KEM E represents genle on the skin and is an effective alternative in cosmetic preservation approved in natural and organic cosmetic. No. Trade name INCI name Dosage % wt. Supplier 1 Water AQUA 33.45 Tinci or Schill 2 Sodium Lauroyl Sarcosinate SODIUM LAUROYL SARCOSINATE 40 and Seilacher 3 TC CAB 35 COCAMIDOPROPYL BETAINE 10 Tinci 4 Leraglu CG L5025 COCO GLUCOSIDE 5 STOCKMEIER 5 Jolee 7908 GLYCERYL LAURATE 2 Oleon 6 Polyquaternium-7 POLYQUATERNIUM7 2 Tinci 7 Sil-O-San 8631C PEG-12 DIMETHICONE 1 Schill and Seilacher GLYCERIN, AQUA, ALOE BARBADENSIS GEL EXTRACT, BETULA ALBA LEAF EXTRACT, CHAMOMILLA RECUTITA EXTRACT, EQUISETUM ARVENSE EXTRACT, URTICA DIOICA EXTRACT, HUMULUS LUPULUS EXTRACT, ARCTIUM LAPPA EXTRACT, 8 Biovitrient 124 1 Bionorm SALVIA OFFICINALIS LEAF EXTRACT, CAMELLIA SINENSIS EXTRACT, LAWSONIA INERMIS EXTRACT, PANICUM MILIACEUM EXTRACT, PANTHENOL, NIACIN, BIOTIN, SODIUM BENZOATE, POTASSIUM SORBATE, CITRIC ACID, GLYCERIN, AQUA, HUMULUS LUPULUS EXTRACT, ROSMARINUS