National OTC Medicines List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Treatment of Herpes Simplex Virus Epithelial Keratitis
THE TREATMENT OF HERPES SIMPLEX VIRUS EPITHELIAL KERATITIS BY Kirk R. Wilhelmus, MD, MPH ABSTRACT Purpose: Epithelial keratitis is the most common presentation of ocular infection by herpes simplex virus (HSV). Quantitative assessment of available therapy is needed to guide evidence-based ophthalmology. This study aimed to compare the efficacy of various treatments for dendritic or geographic HSV epithelial keratitis and to evaluate the role of various clinical characteristics on epithelial healing. Methods: Following a systematic review of the literature, information from clinical trials of HSV dendritic or geographic epithelial keratitis was extracted, and the methodological quality of each study was scored. Methods of epithelial cau- terization and curettage were grouped as relatively equivalent physicochemical therapy, and solution and ointment for- mulations of a given topical antiviral agent were combined. The proportion healed with 1 week of therapy, a scheduled follow-up day that approximated the average time of resolution with antiviral therapy, was selected as the primary out- come based on a masked evaluation of maximum treatment differences in published healing curves. The proportion healed at 14 days was recorded as supplemental information. Fixed-effects and random-effects meta-analysis models were used to obtain summary estimates by pooling results from comparative treatment trials. Hypotheses about which prognostic factors might affect epithelial healing during antiviral therapy were developed by multivariate analysis of the Herpetic Eye Disease Study dataset. Results: After excluding 48 duplicate reports, 14 nonrandomized studies, 15 studies with outdated or similar treatments, and 29 trials lacking sufficient data on healing or accessibility, 76 primary reports were identified. -
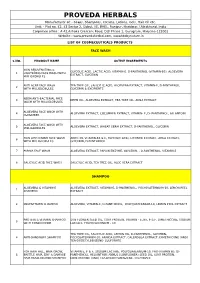
Cosmeceutical Products List
PROVEDA HERBALS Manufacturer of: - Soaps, Shampoos, Creams, Lotions, Gels, Hair Oil etc. Unit: - Plot no. 42, 43 Sector 2, Sidcul, IIE, BHEL, Ranipur, Haridwar, Uttrakhand, India Corporate office : A 42,Ashoka Crescent Road, DLF Phase 1, Gurugram, Haryana-122002 Website : www.provedaherbal.com, www.tbcbynature.in LIST OF COSMECEUTICALS PRODUCTS FACE WASH S.NO. PRODUCT NAME ACTIVE INGREDIENTS SKIN REJUVENATING & GLYCOLIC ACID, LACTIC ACID, VITAMIN-E, D-PANTHENOL (VITAMIN-B5), ALOEVERA 1 LIGHTENING FACE WASH WITH EXTRACT, GLYCERIN MILLIGLOBULES ANTI ACNE FACE WASH TEA TREE OIL, SALICYLIC ACID, ALOEVERA EXTRACT, VITAMIN-E, D-PANTHENOL, 2 WITH MILLIGLOBULES GLYCERIN & EXCIPIENTS NEEM ANTI-BACTERIAL FACE 3 NEEM OIL, ALOEVERA EXTRACT, TEA TREE OIL, AMLA EXTRACT WASH WITH MILLIGLOBULES ALOEVERA FACE WASH WITH 4 ALOEVERA EXTRACT, CUCUMBER EXTRACT, VITAMIN- E, D- PANTHENOL, ALLANTOIN CUCUMBER ALOEVERA FACE WASH WITH 5 ALOEVERA EXTRACT, WHEAT GERM EXTRACT, D-PANTHENOL, GLYCERIN MILLIGLOBULES SKIN LIGHTENING FACE WASH ARBUTIN, VITAMIN-B3 & E, GLYCOLIC ACID, LICORICE EXTRACT, AMLA EXTRACT, 6 WITH MILLIGLOBULES GLYCERIN, D-PANTHENOL 7 PAPAYA FACE WASH ALOEVERA EXTRACT, PAPAIN ENZYME, GLYCERIN, , D-PANTHENOL, VITAMIN-E 8 SALICYLIC ACID FACE WASH SALICYLIC ACID, TEA TREE OIL, ALOE VERA EXTRACT SHAMPOO ALOEVERA & VITAMIN-E ALOEVERA EXTRACT, VITAMIN-E, D-PANTHENOL, POLYQUATERNIUM-10, LEMON PEEL 1 SHAMPOO EXTRACT 2 MULTIVITAMIN SHAMPOO ALOEVERA, VITAMIN-E, D-PANTHENOL, POLYQUATERNIUM-10, LEMON PEEL EXTRACT PROTEIN & VITAMIN SHAMPOO SUN FLOWER SEED OIL, -

Inclusion and Exclusion Criteria for Each Key Question
Supplemental Table 1: Inclusion and exclusion criteria for each key question Chronic HBV infection in adults ≥ 18 year old (detectable HBsAg in serum for >6 months) Definition of disease Q1 Q2 Q3 Q4 Q5 Q6 Q7 HBV HBV infection with infection and persistent compensated Immunoactive Immunotolerant Seroconverted HBeAg HBV mono-infected viral load cirrhosis with Population chronic HBV chronic HBV from HBeAg to negative population under low level infection infection anti-HBe entecavir or viremia tenofovir (<2000 treatment IU/ml) Adding 2nd Stopped antiviral therapy antiviral drug Interventions and Entecavir compared Antiviral Antiviral therapy compared to continued compared to comparisons to tenofovir therapy therapy continued monotherapy Q1-2: Clinical outcomes: Cirrhosis, decompensated liver disease, HCC and death Intermediate outcomes (if evidence on clinical outcomes is limited or unavailable): HBsAg loss, HBeAg seroconversion and Outcomes HBeAg loss Q3-4: Cirrhosis, decompensated liver disease, HCC, relapse (viral and clinical) and HBsAg loss Q5: Renal function, hypophosphatemia and bone density Q6: Resistance, flare/decompensation and HBeAg loss Q7: Clinical outcomes: Cirrhosis, decompensated liver disease, HCC and death Study design RCT and controlled observational studies Acute HBV infection, children and pregnant women, HIV (+), HCV (+) or HDV (+) persons or other special populations Exclusions such as hemodialysis, transplant, and treatment failure populations. Co treatment with steroids and uncontrolled studies. Supplemental Table 2: Detailed Search Strategy: Ovid Database(s): Embase 1988 to 2014 Week 37, Ovid MEDLINE(R) In-Process & Other Non- Indexed Citations and Ovid MEDLINE(R) 1946 to Present, EBM Reviews - Cochrane Central Register of Controlled Trials August 2014, EBM Reviews - Cochrane Database of Systematic Reviews 2005 to July 2014 Search Strategy: # Searches Results 1 exp Hepatitis B/dt 26410 ("hepatitis B" or "serum hepatitis" or "hippie hepatitis" or "injection hepatitis" or 2 178548 "hepatitis type B").mp. -

Tonsillopharyngitis - Acute (1 of 10)
Tonsillopharyngitis - Acute (1 of 10) 1 Patient presents w/ sore throat 2 EVALUATION Yes EXPERT Are there signs of REFERRAL complication? No 3 4 EVALUATION Is Group A Beta-hemolytic Yes DIAGNOSIS Streptococcus (GABHS) • Rapid antigen detection test infection suspected? (RADT) • roat culture No TREATMENT EVALUATION No A Supportive management Is GABHS confi rmed? B Pharmacological therapy (Non-GABHS) Yes 5 TREATMENT A EVALUATE RESPONSEMIMS Supportive management TO THERAPY C Pharmacological therapy • Antibiotics Poor/No Good D Surgery, if recurrent or complicated response response REASSESS PATIENT COMPLETE THERAPY & REVIEW THE DIAGNOSIS© Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B269 © MIMS Pediatrics 2020 Tonsillopharyngitis - Acute (2 of 10) 1 ACUTE TONSILLOPHARYNGITIS • Infl ammation of the tonsils & pharynx • Etiologies include bacterial (group A β-hemolytic streptococcus, Haemophilus infl uenzae, Fusobacterium sp, etc) & viral (infl uenza, adenovirus, coronavirus, rhinovirus, etc) pathogens • Sore throat is the most common presenting symptom in older children TONSILLOPHARYNGITIS 2 EVALUATION FOR COMPLICATIONS • Patients w/ sore throat may have deep neck infections including epiglottitis, peritonsillar or retropharyngeal abscess • Examine for signs of upper airway obstruction Signs & Symptoms of Sore roat w/ Complications • Trismus • Inability to swallow liquids • Increased salivation or drooling • Peritonsillar edema • Deviation of uvula -

Antimicrobial Activity of Cationic
ANTIMICROBIAL ACTIVITY OF CATIONIC ANTISEPTICS IN LAYER-BY-LAYER THIN FILM ASSEMBLIES A Thesis by CHARLENE MYRIAH DVORACEK Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE May 2009 Major Subject: Mechanical Engineering ANTIMICROBIAL ACTIVITY OF CATIONIC ANTISEPTICS IN LAYER-BY-LAYER THIN FILM ASSEMBLIES A Thesis by CHARLENE MYRIAH DVORACEK Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Approved by: Chair of Committee, Jaime Grunlan Committee Members, Michael Benedik Xinghang Zhang Head of Department, Dennis O'Neal May 2009 Major Subject: Mechanical Engineering iii ABSTRACT Antimicrobial Activity of Cationic Antiseptics in Layer-by-Layer Thin Film Assemblies. (May 2009) Charlene Myriah Dvoracek, B.S., Rose-Hulman Institute of Technology Chair of Advisory Committee: Dr. Jaime Grunlan Layer-by-layer (LbL) assembly has proven to be a powerful technique for assembling thin films with a variety of properties including electrochromic, molecular sensing, oxygen barrier, and antimicrobial. LbL involves the deposition of alternating cationic and anionic ingredients from solution, utilizing the electrostatic charges to develop multilayer films. The present work incorporates cationic antimicrobial agents into the positively-charged layers of LbL assemblies. When these thin films are exposed to a humid environment, the antimicrobial molecules readily diffuse out and prevent bacterial growth. The influence of exposure time, testing temperature, secondary ingredients and number of bilayers on antimicrobial efficacy is evaluated here. Additionally, film growth and microstructure are analyzed to better understand the behavior of these films. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009. -

Being Aware of Chlorhexidine Allergy
Being aware of chlorhexidine allergy If you have an immediate allergic reaction to chlorhexidine you may experience symptoms such as: x itching x skin rash (hives) x swelling x anaphylaxis. People who develop anaphylaxis to chlorhexidine may have experienced mild reactions, such as skin rash, to chlorhexidine before. Irritant contact dermatitis or allergic contact dermatitis Chlorhexidine can also cause irritant dermatitis. This is not a true allergic reaction. It is caused by chlorhexidine directly irritating skin and results in rough, dry and scaly Chlorhexidine is an antiseptic. Allergic reactions to skin, sometimes with weeping sores. chlorhexidine are rare but are becoming more common. Chlorhexidine is used in many products both in Chlorhexidine can also cause allergic contact hospitals and in the community. dermatitis. Symptoms look like irritant dermatitis, but the cause of the symptoms is delayed by 12-48 hours Why have I been given this factsheet? after contact with chlorhexidine. You have been given this brochure because you have had a reaction to a medication, a medical dressing Both irritant dermatitis and allergic contact dermatitis or antiseptic. This may or may not be caused by a caused by chlorhexidine are annoying but not chlorhexidine allergy. dangerous. It is important that you are aware of the possibility of an It is recommended that you avoid chlorhexidine if you allergy. experience these responses as some people have gone on to develop immediate allergic reaction to chlorhexidine. Allergic reactions to chlorhexidine Severe allergic reactions to chlorhexidine are rare, but How do I know which products contain they can be serious. Immediate allergic reactions can chlorhexidine? cause anaphlaxis (a very severe allergic reaction which can be life-threatening). -

Fluoroquinolones in Children: a Review of Current Literature and Directions for Future Research
Academic Year 2015 - 2016 Fluoroquinolones in children: a review of current literature and directions for future research Laurens GOEMÉ Promotor: Prof. Dr. Johan Vande Walle Co-promotor: Dr. Kevin Meesters, Dr. Pauline De Bruyne Dissertation presented in the 2nd Master year in the programme of Master of Medicine in Medicine 1 Deze pagina is niet beschikbaar omdat ze persoonsgegevens bevat. Universiteitsbibliotheek Gent, 2021. This page is not available because it contains personal information. Ghent Universit , Librar , 2021. Table of contents Title page Permission for loan Introduction Page 4-6 Methodology Page 6-7 Results Page 7-20 1. Evaluation of found articles Page 7-12 2. Fluoroquinolone characteristics in children Page 12-20 Discussion Page 20-23 Conclusion Page 23-24 Future perspectives Page 24-25 References Page 26-27 3 1. Introduction Fluoroquinolones (FQ) are a class of antibiotics, derived from modification of quinolones, that are highly active against both Gram-positive and Gram-negative bacteria. In 1964,naladixic acid was approved by the US Food and Drug Administration (FDA) as first quinolone (1). Chemical modifications of naladixic acid resulted in the first generation of FQ. The antimicrobial spectrum of FQ is broader when compared to quinolones and the tissue penetration of FQ is significantly deeper (1). The main FQ agents are summed up in table 1. FQ owe its antimicrobial effect to inhibition of the enzymes bacterial gyrase and topoisomerase IV which have essential and distinct roles in DNA replication. The antimicrobial spectrum of FQ include Enterobacteriacae, Haemophilus spp., Moraxella catarrhalis, Neiserria spp. and Pseudomonas aeruginosa (1). And FQ usually have a weak activity against methicillin-resistant Staphylococcus aureus (MRSA). -

A Comparative Evaluation of Terbinafine and Eberconazole in the Management of Tinea Versicolor
International Journal of Dermatology, Venereology and Leprosy Sciences. 2019; 2(2): 13-15 E-ISSN: 2664-942X P-ISSN: 2664-9411 www.dermatologypaper.com/ A comparative evaluation of Terbinafine and Derma 2019; 2(2): 13-15 Received: 13-05-2019 Eberconazole in the management of Tinea versicolor Accepted: 15-06-2019 Dr. Kalyani Mishra Dr. Kalyani Mishra Department of Dermatology, IPGMER and SSKM Hospital, DOI: https://doi.org/10.33545/26649411.2019.v2.i2a.26 Kolkata, West Bengal, India Abstract Introduction: Tinea versicolor is one of the most common infectious skin diseases that is seen in abundance during summer. The present study compared Terbinafine and Eberconazole in the management of Tinea versicolor. Materials & Methods: The present study was conducted on 235 cases (Group I) of Tinea versicolor of both genders. Patients were randomly divided into two study groups, i.e. Group I patients were given eberconazole 1% cream once daily for 2 weeks and Group II were given terbinafine 1% cream once daily for 2 weeks. Safety assessment was recorded. Results: Out of 240 patients, males were 125 and females were 115. In group I, 96 patients had complete healing while 72 patients in group II had complete healing, 24 in group I and 43 in group II had mild residual disease, 5 in group II had considerable residual. The difference was significant (P< 0.05). Conclusion: Authors found that eberconazole 1% cream was as effective as compared to terbinafine 1% in patients with Pityriasis versicolor. Keywords: Eberconazole, Terbinafine, Pityriasis versicolor Introduction Tinea versicolor (TV) or pityriasis versicolor, also known as Peter Elam’s disease, is one of [1] the most common infectious skin diseases that is seen in abundance during summer . -

Review Article Sporotrichosis: an Overview and Therapeutic Options
Hindawi Publishing Corporation Dermatology Research and Practice Volume 2014, Article ID 272376, 13 pages http://dx.doi.org/10.1155/2014/272376 Review Article Sporotrichosis: An Overview and Therapeutic Options Vikram K. Mahajan Department of Dermatology, Venereology & Leprosy, Dr. R. P. Govt. Medical College, Kangra, Tanda, Himachal Pradesh 176001, India Correspondence should be addressed to Vikram K. Mahajan; [email protected] Received 30 July 2014; Accepted 12 December 2014; Published 29 December 2014 Academic Editor: Craig G. Burkhart Copyright © 2014 Vikram K. Mahajan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Sporotrichosis is a chronic granulomatous mycotic infection caused by Sporothrix schenckii, a common saprophyte of soil, decaying wood, hay, and sphagnum moss, that is endemic in tropical/subtropical areas. The recent phylogenetic studies have delineated the geographic distribution of multiple distinct Sporothrix species causing sporotrichosis. It characteristically involves the skin and subcutaneous tissue following traumatic inoculation of the pathogen. After a variable incubation period, progressively enlarging papulo-nodule at the inoculation site develops that may ulcerate (fixed cutaneous sporotrichosis) or multiple nodules appear proximally along lymphatics (lymphocutaneous sporotrichosis). Osteoarticular sporotrichosis or primary pulmonary sporotrichosis are rare and occur from direct inoculation or inhalation of conidia, respectively. Disseminated cutaneous sporotrichosis or involvement of multiple visceral organs, particularly the central nervous system, occurs most commonly in persons with immunosuppression. Saturated solution of potassium iodide remains a first line treatment choice for uncomplicated cutaneous sporotrichosis in resource poor countries but itraconazole is currently used/recommended for the treatment of all forms of sporotrichosis. -

Herpes Simplex Virus
HSV Herpes simplex virus HSV (Herpes simplex virus) can be spread when an infected person is producing and shedding the virus. Herpes simplex can be spread through contact with saliva, such as sharing drinks. Symptoms of herpes simplex virus infection include watery blisters in the skin or mucous membranes of the mouth, lips or genitals. Lesions heal with ascab characteristic of herpetic disease. As neurotropic and neuroinvasive viruses, HSV-1 and -2 persist in the body by becoming latent and hiding from the immune system in the cell bodies of neurons. After the initial or primary infection, some infected people experience sporadic episodes of viral reactivation or outbreaks. www.MedChemExpress.com 1 HSV Inhibitors (Z)-Capsaicin 1-Docosanol (Zucapsaicin; Civamide; cis-Capsaicin) Cat. No.: HY-B1583 (Behenyl alcohol) Cat. No.: HY-B0222 (Z)-Capsaicin is the cis isomer of capsaicin, acts 1-Docosanol is a saturated fatty alcohol used as an orally active TRPV1 agonist, and is used in traditionally as an emollient, emulsifier, and the research of neuropathic pain. thickener in cosmetics, and nutritional supplement; inhibitor of lipid-enveloped viruses including herpes simplex. Purity: 99.96% Purity: ≥98.0% Clinical Data: Launched Clinical Data: Launched Size: 10 mM × 1 mL, 10 mg, 50 mg Size: 500 mg 2-Deoxy-D-glucose 20(R)-Ginsenoside Rh2 (2-DG; 2-Deoxy-D-arabino-hexose; D-Arabino-2-deoxyhexose) Cat. No.: HY-13966 Cat. No.: HY-N1401 2-Deoxy-D-glucose is a glucose analog that acts as 20(R)-Ginsenoside Rh2, a matrix a competitive inhibitor of glucose metabolism, metalloproteinase (MMP) inhibitor, acts as a inhibiting glycolysis via its actions on hexokinase.