Resistance to Second Generation Antiandrogens in Prostate Cancer: Pathways and Mechanisms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The 2021 List of Pharmacological Classes of Doping Agents and Doping Methods
BGBl. III - Ausgegeben am 8. Jänner 2021 - Nr. 1 1 von 23 The 2021 list of pharmacological classes of doping agents and doping methods www.ris.bka.gv.at BGBl. III - Ausgegeben am 8. Jänner 2021 - Nr. 1 2 von 23 www.ris.bka.gv.at BGBl. III - Ausgegeben am 8. Jänner 2021 - Nr. 1 3 von 23 THE 2021 PROHIBITED LIST WORLD ANTI-DOPING CODE DATE OF ENTRY INTO FORCE 1 January 2021 Introduction The Prohibited List is a mandatory International Standard as part of the World Anti-Doping Program. The List is updated annually following an extensive consultation process facilitated by WADA. The effective date of the List is 1 January 2021. The official text of the Prohibited List shall be maintained by WADA and shall be published in English and French. In the event of any conflict between the English and French versions, the English version shall prevail. Below are some terms used in this List of Prohibited Substances and Prohibited Methods. Prohibited In-Competition Subject to a different period having been approved by WADA for a given sport, the In- Competition period shall in principle be the period commencing just before midnight (at 11:59 p.m.) on the day before a Competition in which the Athlete is scheduled to participate until the end of the Competition and the Sample collection process. Prohibited at all times This means that the substance or method is prohibited In- and Out-of-Competition as defined in the Code. Specified and non-Specified As per Article 4.2.2 of the World Anti-Doping Code, “for purposes of the application of Article 10, all Prohibited Substances shall be Specified Substances except as identified on the Prohibited List. -

Prnu-BICALUTAMIDE
PRODUCT MONOGRAPH PrNU-BICALUTAMIDE Bicalutamide Tablets, 50 mg Non-Steroidal Antiandrogen NU-PHARM INC. DATE OF PREPARATION: 50 Mural Street, Units 1 & 2 October 16, 2009 Richmond Hill, Ontario L4B 1E4 Control#: 133521 Page 1 of 27 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION....................................................... 3 SUMMARY PRODUCT INFORMATION ............................................................................. 3 INDICATIONS AND CLINICAL USE ................................................................................... 3 CONTRAINDICATIONS ........................................................................................................ 3 WARNINGS AND PRECAUTIONS....................................................................................... 4 ADVERSE REACTIONS......................................................................................................... 5 DRUG INTERACTIONS ......................................................................................................... 9 DOSAGE AND ADMINISTRATION ................................................................................... 10 OVERDOSAGE...................................................................................................................... 10 ACTION AND CLINICAL PHARMACOLOGY.................................................................. 10 STORAGE AND STABILITY............................................................................................... 11 DOSAGE FORMS, COMPOSITION AND PACKAGING -

Campro Catalog Stable Isotope
Introduction & Welcome Dear Valued Customer, We are pleased to present to you our Stable Isotopes Catalog which contains more than three thousand (3000) high quality labeled compounds. You will find new additions that are beneficial for your research. Campro Scientific is proud to work together with Isotec, Inc. for the distribution and marketing of their stable isotopes. We have been working with Isotec for more than twenty years and know that their products meet the highest standard. Campro Scientific was founded in 1981 and we provide services to some of the most prestigious universities, research institutes and laboratories throughout Europe. We are a research-oriented company specialized in supporting the requirements of the scientific community. We are the exclusive distributor of some of the world’s leading producers of research chemicals, radioisotopes, stable isotopes and environmental standards. We understand the requirements of our customers, and work every day to fulfill them. In working with us you are guaranteed to receive: - Excellent customer service - High quality products - Dependable service - Efficient distribution The highly educated staff at Campro’s headquarters and sales office is ready to assist you with your questions and product requirements. Feel free to call us at any time. Sincerely, Dr. Ahmad Rajabi General Manager 180/280 = unlabeled 185/285 = 15N labeled 181/281 = double labeled (13C+15N, 13C+D, 15N+18O etc.) 186/286 = 12C labeled 182/282 = d labeled 187/287 = 17O labeled 183/283 = 13C labeleld 188/288 = 18O labeled 184/284 = 16O labeled, 14N labeled 189/289 = Noble Gases Table of Contents Ordering Information.................................................................................................. page 4 - 5 Packaging Information .............................................................................................. -

A Phase 1 Multiple-Dose Study of Orteronel in Japanese Patients with Castration-Resistant Prostate Cancer
Cancer Chemother Pharmacol (2015) 75:373–380 DOI 10.1007/s00280-014-2654-y ORIGINAL ARTICLE A phase 1 multiple-dose study of orteronel in Japanese patients with castration-resistant prostate cancer Kazuhiro Suzuki · Seiichiro Ozono · Akito Yamaguchi · Hidekazu Koike · Hiroshi Matsui · Masao Nagata · Takatoshi Takubo · Kana Miyashita · Takafumi Matsushima · Hideyuki Akaza Received: 6 November 2014 / Accepted: 14 December 2014 / Published online: 24 December 2014 © The Author(s) 2014. This article is published with open access at Springerlink.com Abstract Cycle 1 in this study. Adverse events (AEs) were reported Purpose Orteronel (TAK-700) is a non-steroidal, selec- in all 15 patients. Most common AEs (>30 %) were hyper- tive, reversible inhibitor of 17,20-lyase. We evaluated the lipasemia (47 %), hyperamylasemia (40 %), and consti- safety, tolerability, pharmacokinetics, pharmacodynamics, pation (33 %). Acute pancreatitis (Grades 2 and 3) and and antitumor effect of orteronel with or without predniso- pancreatitis (Grade 1) were complicated in three patients lone in Japanese patients with castration-resistant prostate during the study. Dose-dependent increase in plasma orte- cancer (CRPC). ronel concentrations was indicated over the 200–400 mg Methods We conducted a phase 1 study in men with pro- BID dose range. Prednisolone coadministered did not alter gressive and chemotherapy-naïve CRPC. Patients received PK of orteronel. Serum testosterone was rapidly suppressed orteronel orally at doses of 200–400 mg twice daily (BID) below the lower limit of quantification across all doses. Of with or without oral prednisolone (5 mg BID). Dose-limit- 15 subjects, 13 achieved at least a 50 % reduction from ing toxicity (DLT) was assessed during Cycle 1 (28 days). -

Drug Testing Program
DRUG TESTING PROGRAM Copyright © 2021 CrossFit, LLC. All Rights Reserved. CrossFit is a registered trademark ® of CrossFit, LLC. 2021 DRUG TESTING PROGRAM 2021 DRUG TESTING CONTENTS 1. DRUG-FREE COMPETITION 2. ATHLETE CONSENT 3. DRUG TESTING 4. IN-COMPETITION/OUT-OF-COMPETITION DRUG TESTING 5. REGISTERED ATHLETE TESTING POOL (OUT-OF-COMPETITION DRUG TESTING) 6. REMOVAL FROM TESTING POOL/RETIREMENT 6A. REMOVAL FROM TESTING POOL/WATCH LIST 7. TESTING POOL REQUIREMENTS FOLLOWING A SANCTION 8. DRUG TEST NOTIFICATION AND ADMINISTRATION 9. SPECIMEN ANALYSIS 10. REPORTING RESULTS 11. DRUG TESTING POLICY VIOLATIONS 12. ENFORCEMENT/SANCTIONS 13. APPEALS PROCESS 14. LEADERBOARD DISPLAY 15. EDUCATION 16. DIETARY SUPPLEMENTS 17. TRANSGENDER POLICY 18. THERAPEUTIC USE EXEMPTION APPENDIX A: 2020-2021 CROSSFIT BANNED SUBSTANCE CLASSES APPENDIX B: CROSSFIT URINE TESTING PROCEDURES - (IN-COMPETITION) APPENDIX C: TUE APPLICATION REQUIREMENTS Drug Testing Policy V4 Copyright © 2021 CrossFit, LLC. All Rights Reserved. CrossFit is a registered trademark ® of CrossFit, LLC. [ 2 ] 2021 DRUG TESTING PROGRAM 2021 DRUG TESTING 1. DRUG-FREE COMPETITION As the world’s definitive test of fitness, CrossFit Games competitions stand not only as testaments to the athletes who compete but to the training methodologies they use. In this arena, a true and honest comparison of training practices and athletic capacity is impossible without a level playing field. Therefore, the use of banned performance-enhancing substances is prohibited. Even the legal use of banned substances, such as physician-prescribed hormone replacement therapy or some over-the-counter performance-enhancing supplements, has the potential to compromise the integrity of the competition and must be disallowed. With the health, safety, and welfare of the athletes, and the integrity of our sport as top priorities, CrossFit, LLC has adopted the following Drug Testing Policy to ensure the validity of the results achieved in competition. -

(19) United States (12) Patent Application Publication (Io) Pub
llIIlIlllIlIlIllIlIllIllIllIIlIlllIlIIllllIIlllIIlIlllIIlIlllllIIIlllIlIllIIIIIIIIIIIIIIII US 20160015712AI (19) United States (12) Patent Application Publication (Io) Pub. No. : US 2016/0015712 A1 DORSCH et al. (43) Pub. Date: Jan. 21, 2016 (54) TRIAZOLO [4,5-D]PYRIMIDINE Publication Classification DERIVATIVES (51) Int. Cl. (71) Applicant: MERCK PATENT GMBH, Darmstadt 261K31/519 (2006.01) (DE) 261K31/53 77 (2006.01) C07D 519/00 (2006.01) (72) Inventors: Dieter DORSCH, Ober-Ramstadt (DE); C07D 487/04 (2006.01) Guenter HOELZEMANN, (52) U.S. Cl. Seeheim- Jugenheim (DE); Michel CPC ............ 261K31/519 (2013.01); C07D 487/04 CALDERINI, Darmstadt (DE); Ansgar (2013.01);261K31/5377 (2013.01); C07D WEGENER, Heusenstamm (DE); 519/00 (2013.01) Oliver POESCHKE, Wiesbaden (DE) (57) ABSTRACT (73) Assignee: MERCK PATENT GMBH, Darmstadt (DE) Compounds of the formula I (21) Appl. No. : 14/772, 865 (22) PCT Filed: Feb. 10, 2014 H (86) PCT No. : PCT/EP2014/000361 II ) 371 (c)(I), NX N (2) Date: Sep. 4, 2015 (30) Foreign Application Priority Data in which R' and R have the meanings indicated in Claim 1, are inhibitors of GCN2, and can be employed, inter alia, for Mar. 5, 2013 (EP) ... 13001110.9 the treatment of cancer. US 2016/0015712 A1 Jan. 21, 2016 TRIAZOLO [4,5-D]PYRIMIDINE [0006] Several mechanistic studies discovered that DERIVATIVES immune escape has an important interface with metabolic alterations within the tumor microenvironment. Here impor- BACKGROUND OF THE INVENTION tant roles in mediating immune tolerance to antigens have been associated to the catabolism ofthe essential amino acids [0001] The invention had the object of finding novel com- tryptophan and arginine, carried out by the enzymes pounds having valuable properties, in particular those which indoleamine 2,3-dioxygenase (IDO) and arginase I (ARG), can be used for the medicaments. -

Galeterone for the Treatment of Castration- Resistant Prostate Cancer Bruce Montgomery1, Mario A
Published OnlineFirst November 2, 2015; DOI: 10.1158/1078-0432.CCR-15-1432 Cancer Therapy: Clinical Clinical Cancer Research Androgen Receptor Modulation Optimized for Response (ARMOR) Phase I and II Studies: Galeterone for the Treatment of Castration- Resistant Prostate Cancer Bruce Montgomery1, Mario A. Eisenberger2, Matthew B. Rettig3, Franklin Chu4, Roberto Pili5, Joseph J. Stephenson6, Nicholas J. Vogelzang7, Alan J. Koletsky8, Luke T. Nordquist9, William J. Edenfield10, Khalid Mamlouk11, Karen J. Ferrante11, and Mary-Ellen Taplin12 Abstract Purpose: Galeterone is a selective, multitargeted agent that Results: In ARMOR1, across all doses, 49.0% (24/49) achieved a inhibits CYP17, antagonizes the androgen receptor (AR), and 30% decline in prostate-specific antigen (PSA; PSA30) and reduces AR expression in prostate cancer cells by causing an 22.4% (11/49) demonstrated a 50% PSA decline (PSA50). In increase in AR protein degradation. These open-label phase I ARMOR2 part 1, across all doses, PSA30 was 64.0% (16/25) and and II studies [Androgen Receptor Modulation Optimized PSA50 was 48.0% (12/25). In the 2,550-mg dose cohort, PSA30 for Response-1 (ARMOR1) and ARMOR2 part 1] evaluated was 72.7% (8/11) and PSA50 was 54.5% (6/11). Galeterone was the efficacy and safety of galeterone in patients with treat- well tolerated; the most common adverse events were fatigue, ment-naive nonmetastatic or metastatic castration-resistant increased liver enzymes, gastrointestinal events, and pruritus. Most prostate cancer (CRPC) and established a dose for further were mild or moderate in severity and required no action and there study. were no apparent mineralocorticoid excess (AME) events. -

Disposition of T Oxic Drugs and Chemicals
Disposition of Toxic Drugs and Chemicals in Man, Eleventh Edition Eleventh Edition in Man and Chemicals Drugs Toxic Disposition of The purpose of this work is to present in a single convenient source the current essential information on the disposition of the chemi- cals and drugs most frequently encountered in episodes of human poisoning. The data included relate to the body fluid concentrations of substances in normal or therapeutic situations, concentrations in fluids and tissues in instances of toxicity and the known metabolic fate of these substances in man. Brief mention is made of specific analytical procedures that are applicable to the determination of each substance and its active metabolites in biological specimens. It is expected that such information will be of particular interest and use to toxicologists, pharmacologists, clinical chemists and clinicians who have need either to conduct an analytical search for these materials in specimens of human origin or to interpret 30 Amberwood Parkway analytical data resulting from such a search. Ashland, OH 44805 by Randall C. Baselt, Ph.D. Former Director, Chemical Toxicology Institute Bookmasters Foster City, California HARD BOUND, 7” x 10”, 2500 pp., 2017 ISBN 978-0-692-77499-1 USA Reviewer Comments on the Tenth Edition “...equally useful for clinical scientists and poison information centers and others engaged in practice and research involving drugs.” Y. Caplan, J. Anal. Tox. “...continues to be an invaluable and essential resource for the forensic toxicologist and pathologist.” D. Fuller, SOFT ToxTalk “...has become an essential reference book in many laboratories that deal with clinical or forensic cases of poisoning.” M. -

WO 2018/111890 Al 21 June 2018 (21.06.2018) W !P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/111890 Al 21 June 2018 (21.06.2018) W !P O PCT (51) International Patent Classification: EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, C07K 16/28 (2006.01) A61K 31/4166 (2006.01) MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, 59/595 (2006.01) TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, KM, ML, MR, NE, SN, TD, TG). (21) International Application Number: PCT/US20 17/065841 Declarations under Rule 4.17: (22) International Filing Date: — as to applicant's entitlement to apply for and be granted a 12 December 2017 (12.12.2017) patent (Rule 4.1 7(H)) — as to the applicant's entitlement to claim the priority of the (25) Filing Language: English earlier application (Rule 4.17(Hi)) (26) Publication Langi English — of inventorship (Rule 4.1 7(iv)) (30) Priority Data: Published: 62/433,158 12 December 2016 (12.12.2016) US — with international search report (Art. 21(3)) — with sequence listing part of description (Rule 5.2(a)) (71) Applicant (for all designated States except AL, AT, BE, BG, CH, CN, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IN, IS, IT, LT, LU, LV, MC, MK, MT, NL, NO, PL, P T RO, RS, SE, SI, SK, SM, TR): GENENTECH, INC. [US/US]; 1 DNA Way, South San Francisco, CA 94080-4990 (US). -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -
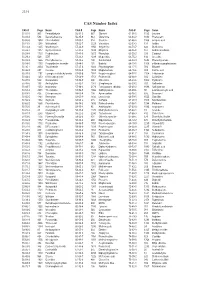
CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

LIGANDROL Comprometimento Ósseo
Apresenta ação anabólica com poucos efeitos androgênicos e virilizantes Auxilia no tratamento de condições onde há perda de massa muscular e LIGANDROL comprometimento ósseo Promove a hipertrofia e aumenta a força muscular O QUE É? RA especialmente pelos ligantes exógenos, como os esteróides anabolizantes androgênicos (EAA), pode estar envolvida com o O ligandrol, também conhecido como anabolicum ou LGD- desenvolvimento de patologias na próstata, coração e fígado. Isto 4033, é caracterizado como um modulador seletivo do receptor porque, o receptor RA está expresso em diferentes tecidos, o que de androgênio (SARM) de estrutura não esteroidal que atua de de certa forma limita o uso terapêutico dos EAA em condições forma seletiva sobre os tecidos que expressam os receptores mais específicas como sarcopenia, caquexia associada à doenças androgênicos (RA). Por sua especificidade e alta afinidade ao como câncer, osteoporose e hipogonadismo. RA, tem sido demonstrado que o ligandrol apresenta atividade anabólica no músculo e anti – reabsortiva e anabólica no tecido Com o intuito de contornar possíveis limitações que resultam da ósseo, ao passo que apresenta efeitos androgênicos mínimos ativação global dos RA, os moduladores seletivos de receptores sobre próstata, couro cabeludo e pele. 1 androgênicos, também conhecidos como SARMs, do inglês Selective Androgen Receptor Modulators, tem sido objeto de Os SARMs como o ligandrol e ostarine, têm sido avaliados como estudo uma vez que parecem ativar os RA de maneira específica uma alternativa eficaz e segura para o tratamento de perda e seletiva em determinados tecidos, reduzindo também a de massa muscular associada ao envelhecimento e a outras ocorrência de efeitos colaterais indesejados.