MICROMEDEX® Healthcare Series Document
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -
A Systematic Review of Combination and High-Dose Atypical
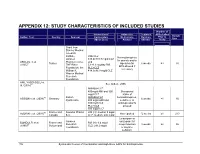
APPENDIX 12: STUDY CHARACTERISTICS OF INCLUDED STUDIES Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study Grant from Stanley Medical research Institute, RIS+CLZ Benzodiazepines Janssen 515.6±138.7 mg/d CLZ for anxiety and/or AKDEDE et al. Pharmaceutica, and 42 Turkey biperiden for 6 weeks ≥3 30 (2005) THE Ritter 5.1±1.3 mg/day RIS EPS allowed if Foundation, the PLC+CLZ necessary William K. 414.3±96.9 mg/d CLZ Warren Medical Research Foundation ANIL YAGCIOGLU et 45 See Akdede 2006 al. (2005) AMI400+CLZ 400mg/d AMI and 300 Occasional mg/d CLZ intake of 49 Sanofi- AMI600+CLZ benzodiazepines, ASSION et al. (2008) Germany 6 weeks ≥1 16 Synthelabo 600 mg/d AMI and sedatives, or 300mg/d CLZ antidepressants PLC+CLZ allowed 300 mg/d CLZ 60 France and Novartis Phama RIS (H): median 9 mg/d AZORIN et al. (2001) Not reported 12 weeks ≥1 273 Canada S.A. CLZ: median: 600 mg/d Lorazepam or Janssen oxazepam for BONDOLFI et al. France and RIS (H): 6.4 mg/d 66 Research sleep induction 8 weeks ≥2 86 (1998) Switzerland CLZ: 291.2 mg/d Foundation or daytime sedation; 156 Systematic Review of Combination and High-Dose AAPs for Schizophrenia Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study biperiden and procyclidine for EPS Supported by grants from Brain Research center, funded by the ARI+CLZ Antidepressants, Ministry of 15.5±7.1 mg/d ARI and 38 anticholinergics CHANG et al. -

Partial Agreement in the Social and Public Health Field
COUNCIL OF EUROPE COMMITTEE OF MINISTERS (PARTIAL AGREEMENT IN THE SOCIAL AND PUBLIC HEALTH FIELD) RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies, and superseding Resolution AP (82) 2) AND APPENDIX I Alphabetical list of medicines adopted by the Public Health Committee (Partial Agreement) updated to 1 July 1988 APPENDIX II Pharmaco-therapeutic classification of medicines appearing in the alphabetical list in Appendix I updated to 1 July 1988 RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (superseding Resolution AP (82) 2) (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies) The Representatives on the Committee of Ministers of Belgium, France, the Federal Republic of Germany, Italy, Luxembourg, the Netherlands and the United Kingdom of Great Britain and Northern Ireland, these states being parties to the Partial Agreement in the social and public health field, and the Representatives of Austria, Denmark, Ireland, Spain and Switzerland, states which have participated in the public health activities carried out within the above-mentioned Partial Agreement since 1 October 1974, 2 April 1968, 23 September 1969, 21 April 1988 and 5 May 1964, respectively, Considering that the aim of the Council of Europe is to achieve greater unity between its members and that this -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX -

Tympanic Measurement of Body Temperature in Stroke Patients
J Neurol Neurosurg Psychiatry 2005;76:1039–1042 1039 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.058149 on 16 June 2005. Downloaded from PostScript.............................................................................................. patient underwent surgery. Because of dystonia after pallidal stimulation or palli- LETTERS thoracic kyphosis, he could not be placed dotomy. in a head coil or neck quad. We therefore In our opinion, compared with pallido- obtained a pre-operative CT scan for ‘‘indivi- tomies in Parkinson’s disease, the target for Long term results of unilateral dual targeting’’. The coordinates of a target in TD and dystonia could be anatomically posteroventral pallidotomy for the posteroventral globus pallidus (GP) were slightly different—that is, more lateral in established (2 mm in front of the mid the posteroventral GP perhaps because of antipsychotic drug induced anterior–posterior commissure (AC-PC), different activity of the GpE. More study into tardive dyskinesia 5 mm below the AC-PC and 21 mm lateral this pathology is needed. Tardive dyskinesia (TD) is a well known side of the AC-PC (head width 16 cm, third effect of neuroleptic drug treatment, and may ventricle width 6 mm, AC-PC 25 mm long)). M W P M Lenders, H P J Buschman coexist with tardive dystonia.1 It can be Five lesions were made at 8, 6, 4, and 2 mm, Department of Neurosurgery, Medical Spectrum Twente, Enschede, The Netherlands treated with several drugs, although they and on target at 82˚for 60 s. As this did not result in a satisfying improvement of dyski- rarely lead to a complete removal of symp- M D I Vergouwen toms. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

PHARMACEUTICAL APPENDIX to the HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2008) (Rev
Harmonized Tariff Schedule of the United States (2008) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2008) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM GADOCOLETICUM 280776-87-6 ABAFUNGIN 129639-79-8 ACIDUM LIDADRONICUM 63132-38-7 ABAMECTIN 65195-55-3 ACIDUM SALCAPROZICUM 183990-46-7 ABANOQUIL 90402-40-7 ACIDUM SALCLOBUZICUM 387825-03-8 ABAPERIDONUM 183849-43-6 ACIFRAN 72420-38-3 ABARELIX 183552-38-7 ACIPIMOX 51037-30-0 ABATACEPTUM 332348-12-6 ACITAZANOLAST 114607-46-4 ABCIXIMAB 143653-53-6 ACITEMATE 101197-99-3 ABECARNIL 111841-85-1 ACITRETIN 55079-83-9 ABETIMUSUM 167362-48-3 ACIVICIN 42228-92-2 ABIRATERONE 154229-19-3 ACLANTATE 39633-62-0 ABITESARTAN 137882-98-5 ACLARUBICIN 57576-44-0 ABLUKAST 96566-25-5 ACLATONIUM NAPADISILATE 55077-30-0 ABRINEURINUM 178535-93-8 ACODAZOLE 79152-85-5 ABUNIDAZOLE 91017-58-2 ACOLBIFENUM 182167-02-8 ACADESINE 2627-69-2 ACONIAZIDE 13410-86-1 ACAMPROSATE -

Emulated Clinical Trials from Longitudinal Real-World
Supplemental Material for “Emulated Clinical Trials from Longitudinal Real-World Data Efficiently Identify Candidates for Neurological Disease Modification: Examples from Parkinson's Disease” Table S1. ICD codes for PD cohort definition Type System Code Name icd9 3320 Paralysis agitans Inclusion icd10 G20 Parkinson's disease icd9 3316 Corticobasal degeneration icd9 3321 Secondary parkinsonism icd9 3330 Other degenerative diseases of the basal ganglia Exclusion icd10 G21 Secondary parkinsonism Progressive supranuclear ophthalmoplegia [Steele- icd10 G231 Richardson-Olszewski] icd10 G3185 Corticobasal degeneration Table S2. PD-indicated drugs and their corresponding ATC class names. The list below has been compiled by a domain expert based on the following sources: National Drug File – Reference Terminology (NDF-RT), Anatomical Therapeutic Chemical Classification System (ATC), and DrugBank (45). Drug ATC class code(s) ATC class name(s) Amantadine N04BB Adamantane derivatives Drugs used in erectile dysfunction; dopamine Apomorphine G04BE; N04BC agonists Belladonna alkaloids, tertiary amines; Atropine A03BA; S01FA anticholinergics Benztropine N04AC Ethers of tropine or tropine derivatives Biperiden N04AA Tertiary amines Bornaprine N04AA Tertiary amines Bromocriptine G02CB; N04BC Prolactine inhibitors; dopamine agonists Budipine N04BX Other dopaminergic agents Cabergoline G02CB; N04BC Prolactine inhibitors; dopamine agonists Carbidopa N/A N/A Dexetimide N04AA Tertiary amines Dihydroergocryptine N04BC Dopamine agonists Entacapone N04BX Other -

Anticholinergics for Neuroleptic-Induced Acute Akathisia
Anticholinergics for neuroleptic-induced acute akathisia Item Type Article Authors Rathbone, John Citation Rathbone, J. & Soares-Weiser, K. (2006). Anticholinergics for neuroleptic-induced acute akathisia. Cochrane Database of Systematic Reviews, (4), pp.1-14. Download date 24/09/2021 12:11:45 Link to Item http://hdl.handle.net/20.500.12904/9902 Cochrane Database of Systematic Reviews Anticholinergics for neuroleptic-induced acute akathisia (Review) Rathbone J, Soares-Weiser K Rathbone J, Soares-Weiser K. Anticholinergics for neuroleptic-induced acute akathisia. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD003727. DOI: 10.1002/14651858.CD003727.pub3. www.cochranelibrary.com Anticholinergics for neuroleptic-induced acute akathisia (Review) Copyright © 2012 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 3 METHODS ...................................... 3 RESULTS....................................... 5 DISCUSSION ..................................... 6 AUTHORS’CONCLUSIONS . 6 ACKNOWLEDGEMENTS . 7 REFERENCES ..................................... 7 CHARACTERISTICSOFSTUDIES . 8 DATAANDANALYSES. 10 ADDITIONALTABLES. 10 WHAT’SNEW..................................... 10 HISTORY....................................... 10 CONTRIBUTIONSOFAUTHORS . 11 DECLARATIONSOFINTEREST -

Comprehensive List of Cross-Reactive and Non Cross-Reactive Compounds
Comprehensive List of Cross-Reactive and Non Cross-Reactive Compounds Rev.A 10-8-2002 TOX Specificity-Chemical Name Biosite Inc. Page 1 Highest Conc. Tested Conc. Giving Positive TRADE NAME CHEMICAL NAME DRUG CLASS (ng/ml) (ng/ml) Sectral Acebutolol Antihypertensive 100,000 Ethanal Acetaldehyde Solvent 10,000,000 Tylenol/Paracetamol/APAP Acetaminophen Analgesic 1,000,000 Acetanilide Acetanilide Analgesic 100,000 Diamox Acetazolamide Diuretic 100,000 Dymelor Acetohexamide Antidiabetic 1,000,000 Acetone Acetone Solvent 10,000,000 Notensil Acetopromazine Tranquilizer 100,000 Mucomyst Acetyl-l-cysteine, N- Mucolytic 100,000 LAAM Acetylmethadol, l-a- Narcotic analgesic 100,000 Aspirin Acetylsalicylic acid Analgesic 1,000,000 Aspirin metabolite Acetylsalicylic acid metab.(Salicylic acid) Aspirin metabolite 1,000,000 Aspirin metabolite Acetylsalicylic acid metab.(Salicyluric acid) Aspirin metabolite 100,000 Acyclovir Acyloguanosine Antiviral 100,000 Dowacide Q Adamantane, (1-(3-Chloroallyl)-3,5,7-triaza-1-azonia)- Antibacterial 100,000 Gumbaral Adenosylmethionine, S- Anti-inflammatory 100,000 Deracyn Adinazolam Benzodiazepine 100,000 BZO 1,000 Deracyn metabolite Adinazolam, Desmethyl Benzodiazepine metabolite 100,000 BZO 250 HSA Albumin, Human Protein 5,000,000 Proventil/Ventolin Albuterol Bronchodilator 200,000 Octalene Aldrin Insecticide 100,000 Fosamax Alendronate Bone reabsorption inhibitor 200,000 Diadol Allobarbital Barbiturate 100,000 BAR 150 Zyloprim Allopurinol Antiurolithic 100,000 Nisentil Alphaprodine Narcotic analgesic 100,000 Xanax -

WO 2014/006004 Al 9 January 2014 (09.01.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/006004 Al 9 January 2014 (09.01.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 9/20 (2006.01) A61K 31/485 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/EP2013/06385 1 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KN, KP, KR, 1 July 20 13 (01 .07.2013) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: PA 2012 70405 6 July 2012 (06.07.2012) DK (84) Designated States (unless otherwise indicated, for every 61/668,741 6 July 2012 (06.07.2012) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (71) Applicant: EGALET LTD. -

Extrapyramidal Symptoms Often Arise During Psychiatric Therapy with Neuroleptics
DIFFERENTIAL ANTAGONISM OF ANTIAVOIDANCE, CATALEPTIC AND PTOTIC EFFECTS OF NEUROLEPTICS BY BIPERIDEN Makoto OKA, Kiyoko YAMADA, Chiaki KAMEI, Kouichi YOSHIDA and Masanao SHIMIZU Department of Pharmacology, Research Laboratories, Dainippon Pharmaceutical Co., Ltd., Suita-shi, Osaka 564, Japan Accepted January 11, 1979 Abstract-The interaction between neuroleptics and an anticholinergic, biperiden, in the antiavoidance, catalepsy and ptosis tests was investigated in mice for the purpose of predicting the extrapyramidal side-effects of neuroleptics. The cataleptic effect of most neuroleptics used was antagonized to some extent by biperiden, while the ptotic effect was hardly influenced. The antiavoidance effect of neuroleptics was differen tially antagonized by biperiden. The antiavoidance effect of haloperidol, trifluperidol and perphenazine was markedly antagonized and that of chlorpromazine moderately. However, the effect of thioridazine, chlorprothixene, levomepromazine and clozapine was little antagonized. In neuropharmacological tests, haloperidol, trifluperidol and perphenazine exhibited a selective antidopaminergic activity, while chlorprothixene, levomepromazine and clozapine showed antidopaminergic, antiadrenergic and also anticholinergic activities when similar doses were given. These results indicate that biperiden antagonism may be marked in the tests related to the extrapyramidal symp toms and in drugs liable to induce extrapyramidal side-effects, however, there would be little or no antagonism in drugs possessing the anticholinergic