Emulated Clinical Trials from Longitudinal Real-World
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Biased Allosteric Regulation of the Prostaglandin F2α Receptor: From
Biased Allosteric Regulation of the Prostaglandin F2 Receptor: From Small Molecules to Large Receptor Complexes By Eugénie Goupil Department of Pharmacology and Therapeutics McGill University, Montréal, Canada November, 2012 A thesis submitted to McGill in partial fulfillment of the requirements of the degree of Doctor of philosophy Copyright ©Eugénie Goupil, 2012 ''In theory, there is no difference between theory and practice. In practice, there is.'' -Lawrence Peter ''Yogi'' Berra ii Abstract G protein-coupled receptors (GPCRs) represent the largest family of cell surface receptors, and thus some of the most important targets for drug discovery. By binding to the orthosteric site where endogenous ligands bind, agonists and antagonists differentially modulate signals sent downstream from these receptors. New evidence suggests that GPCRs possess topographically distinct or allosteric binding sites, which may differentially modulate agonist- and antagonist-mediated responses to selectively affect distinct signalling pathways coupled to the same receptor. These sites may either positively or negatively regulate receptor activity, depending on the pathway in question, and thus can act as biased ligands, leading to functional selectivity (or ligand-directed signalling). Another way of allosterically regulating GPCR signalling is through receptor oligomerization, which has recently emerged as a common mechanism for regulating receptor function. The GPCR for prostaglandin F2 FP, is implicated in many important physiological responses, such as parturition, smooth muscle cell contraction and blood pressure regulation. Therefore, evaluating the potential use of allosteric modulators of FP to fine-tune PGF2-mediated signals, as well as generating a better understanding of its putative oligomerization partners would be of significant pharmacological and clinical interest. -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Deficits in Cholinergic Neurotransmission and Their Clinical
www.nature.com/npjparkd All rights reserved 2373-8057/16 REVIEW ARTICLE OPEN Deficits in cholinergic neurotransmission and their clinical correlates in Parkinson’s disease Santiago Perez-Lloret1 and Francisco J Barrantes2 In view of its ability to explain the most frequent motor symptoms of Parkinson’s Disease (PD), degeneration of dopaminergic neurons has been considered one of the disease’s main pathophysiological features. Several studies have shown that neurodegeneration also affects noradrenergic, serotoninergic, cholinergic and other monoaminergic neuronal populations. In this work, the characteristics of cholinergic deficits in PD and their clinical correlates are reviewed. Important neurophysiological processes at the root of several motor and cognitive functions remit to cholinergic neurotransmission at the synaptic, pathway, and circuital levels. The bulk of evidence highlights the link between cholinergic alterations and PD motor symptoms, gait dysfunction, levodopa-induced dyskinesias, cognitive deterioration, psychosis, sleep abnormalities, autonomic dysfunction, and altered olfactory function. The pathophysiology of these symptoms is related to alteration of the cholinergic tone in the striatum and/or to degeneration of cholinergic nuclei, most importantly the nucleus basalis magnocellularis and the pedunculopontine nucleus. Several results suggest the clinical usefulness of antimuscarinic drugs for treating PD motor symptoms and of inhibitors of the enzyme acetylcholinesterase for the treatment of dementia. Data also suggest that these inhibitors and pedunculopontine nucleus deep-brain stimulation might also be effective in preventing falls. Finally, several drugs acting on nicotinic receptors have proved efficacious for treating levodopa-induced dyskinesias and cognitive impairment and as neuroprotective agents in PD animal models. Results in human patients are still lacking. -
A Systematic Review of Combination and High-Dose Atypical
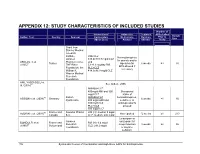
APPENDIX 12: STUDY CHARACTERISTICS OF INCLUDED STUDIES Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study Grant from Stanley Medical research Institute, RIS+CLZ Benzodiazepines Janssen 515.6±138.7 mg/d CLZ for anxiety and/or AKDEDE et al. Pharmaceutica, and 42 Turkey biperiden for 6 weeks ≥3 30 (2005) THE Ritter 5.1±1.3 mg/day RIS EPS allowed if Foundation, the PLC+CLZ necessary William K. 414.3±96.9 mg/d CLZ Warren Medical Research Foundation ANIL YAGCIOGLU et 45 See Akdede 2006 al. (2005) AMI400+CLZ 400mg/d AMI and 300 Occasional mg/d CLZ intake of 49 Sanofi- AMI600+CLZ benzodiazepines, ASSION et al. (2008) Germany 6 weeks ≥1 16 Synthelabo 600 mg/d AMI and sedatives, or 300mg/d CLZ antidepressants PLC+CLZ allowed 300 mg/d CLZ 60 France and Novartis Phama RIS (H): median 9 mg/d AZORIN et al. (2001) Not reported 12 weeks ≥1 273 Canada S.A. CLZ: median: 600 mg/d Lorazepam or Janssen oxazepam for BONDOLFI et al. France and RIS (H): 6.4 mg/d 66 Research sleep induction 8 weeks ≥2 86 (1998) Switzerland CLZ: 291.2 mg/d Foundation or daytime sedation; 156 Systematic Review of Combination and High-Dose AAPs for Schizophrenia Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study biperiden and procyclidine for EPS Supported by grants from Brain Research center, funded by the ARI+CLZ Antidepressants, Ministry of 15.5±7.1 mg/d ARI and 38 anticholinergics CHANG et al. -

Fisiopatologia Dei Tremori
FISIOPATOLOGIA DEI TREMORI Enrico Alfonsi Neurofisiopatologia IRCCS-Istituto Neurologico Nazionale «Casimiro Mondino» Pavia TREMOR A rhythmic involuntary movement of one or several regions of the body. It represents the most common neurological sign, as everyone has a ‘’physiological’’ tremor, which can only be measured with instrumental tools. 1 BACKGROUND Relation to Voluntary Movement Relation to Body Part Rest tremor Head tremor Parkinson’s disease Cerebellar disease Other parkinsonian syndromes Dystonia Tardive (drug-induced) parkinsonism Essential tremor (rarely when isolated) Vascular parkinsonism Chin tremor Hydrocephalus Parkinson’s disease Common Psychogenic (functional) tremor Hereditary geniospasm tremor Action tremor Jaw tremor disorders Postural tremor Parkinson’s disease classified Physiologic tremor and enhanced physiologic tremor Dystonia according Essential tremor Palatal tremor to two main Dystonic tremor Idiopathic (essential) criteria Parkinsonism Owing to brainstem lesions (secondary) Fragile X premutation (fragile X tremor–ataxia syndrome) Owing to degenerative disease (adult-onset Alexander’s disease) Neuropathies Arm tremor Tardive tremor Cerebellar disease Toxins (e.g., mercury) Dystonia Metabolic disorder (e.g., hyperthyroidism, hypoglycemia) Essential tremor Psychogenic (functional) tremor Parkinson’s disease Kinetic tremor Leg tremor Cerebellar disease Parkinson’s disease Holmes’ tremor Orthostatic tremor Wilson’s disease Psychogenic (functional) tremor 2 Essential tremor Features considered typical of the essential tremor syndrome Feature Description Tremor 4–12 Hz action tremor that occurs when patients voluntarily attempt • A resting tremor can appear only in advanced to maintain a steady posture stages. Other neurological signs (with the against gravity (postural tremor) or move (kinetic tremor) exception of cog-wheel phenomenon and Tremor may be suppressed by difficulties with tandem gait) are typically performing skilled manual tasks absent. -

Neuroenhancement in Healthy Adults, Part I: Pharmaceutical
l Rese ca arc ni h li & C f B o i o l e Journal of a t h n Fond et al., J Clinic Res Bioeth 2015, 6:2 r i c u s o J DOI: 10.4172/2155-9627.1000213 ISSN: 2155-9627 Clinical Research & Bioethics Review Article Open Access Neuroenhancement in Healthy Adults, Part I: Pharmaceutical Cognitive Enhancement: A Systematic Review Fond G1,2*, Micoulaud-Franchi JA3, Macgregor A2, Richieri R3,4, Miot S5,6, Lopez R2, Abbar M7, Lancon C3 and Repantis D8 1Université Paris Est-Créteil, Psychiatry and Addiction Pole University Hospitals Henri Mondor, Inserm U955, Eq 15 Psychiatric Genetics, DHU Pe-psy, FondaMental Foundation, Scientific Cooperation Foundation Mental Health, National Network of Schizophrenia Expert Centers, F-94000, France 2Inserm 1061, University Psychiatry Service, University of Montpellier 1, CHU Montpellier F-34000, France 3POLE Academic Psychiatry, CHU Sainte-Marguerite, F-13274 Marseille, Cedex 09, France 4 Public Health Laboratory, Faculty of Medicine, EA 3279, F-13385 Marseille, Cedex 05, France 5Inserm U1061, Idiopathic Hypersomnia Narcolepsy National Reference Centre, Unit of sleep disorders, University of Montpellier 1, CHU Montpellier F-34000, Paris, France 6Inserm U952, CNRS UMR 7224, Pierre and Marie Curie University, F-75000, Paris, France 7CHU Carémeau, University of Nîmes, Nîmes, F-31000, France 8Department of Psychiatry, Charité-Universitätsmedizin Berlin, Campus Benjamin Franklin, Eschenallee 3, 14050 Berlin, Germany *Corresponding author: Dr. Guillaume Fond, Pole de Psychiatrie, Hôpital A. Chenevier, 40 rue de Mesly, Créteil F-94010, France, Tel: (33)178682372; Fax: (33)178682381; E-mail: [email protected] Received date: January 06, 2015, Accepted date: February 23, 2015, Published date: February 28, 2015 Copyright: © 2015 Fond G, et al. -

Partial Agreement in the Social and Public Health Field
COUNCIL OF EUROPE COMMITTEE OF MINISTERS (PARTIAL AGREEMENT IN THE SOCIAL AND PUBLIC HEALTH FIELD) RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies, and superseding Resolution AP (82) 2) AND APPENDIX I Alphabetical list of medicines adopted by the Public Health Committee (Partial Agreement) updated to 1 July 1988 APPENDIX II Pharmaco-therapeutic classification of medicines appearing in the alphabetical list in Appendix I updated to 1 July 1988 RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (superseding Resolution AP (82) 2) (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies) The Representatives on the Committee of Ministers of Belgium, France, the Federal Republic of Germany, Italy, Luxembourg, the Netherlands and the United Kingdom of Great Britain and Northern Ireland, these states being parties to the Partial Agreement in the social and public health field, and the Representatives of Austria, Denmark, Ireland, Spain and Switzerland, states which have participated in the public health activities carried out within the above-mentioned Partial Agreement since 1 October 1974, 2 April 1968, 23 September 1969, 21 April 1988 and 5 May 1964, respectively, Considering that the aim of the Council of Europe is to achieve greater unity between its members and that this -

Phencyclidine: an Update
Phencyclidine: An Update U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse and Mental Health Administration Phencyclidine: An Update Editor: Doris H. Clouet, Ph.D. Division of Preclinical Research National Institute on Drug Abuse and New York State Division of Substance Abuse Services NIDA Research Monograph 64 1986 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administratlon National Institute on Drug Abuse 5600 Fishers Lane Rockville, Maryland 20657 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National lnstitute on Drug Abuse and published by its Office of Science The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. SIDNEY COHEN, M.D. Temple University School of Medicine Los Angeles, California Philadelphia, Pennsylvania SYDNEY ARCHER, Ph.D. MARY L. JACOBSON Rensselaer Polytechnic lnstitute National Federation of Parents for Troy, New York Drug Free Youth RICHARD E. BELLEVILLE, Ph.D. Omaha, Nebraska NB Associates, Health Sciences Rockville, Maryland REESE T. JONES, M.D. KARST J. BESTEMAN Langley Porter Neuropsychiatric lnstitute Alcohol and Drug Problems Association San Francisco, California of North America Washington, D.C. DENISE KANDEL, Ph.D GILBERT J. BOTV N, Ph.D. College of Physicians and Surgeons of Cornell University Medical College Columbia University New York, New York New York, New York JOSEPH V. -

Identification of Potentially Inappropriate Medications with Risk
Journal name: Clinical Interventions in Aging Article Designation: Original Research Year: 2019 Volume: 14 Clinical Interventions in Aging Dovepress Running head verso: Aguiar et al Running head recto: Aguiar et al open access to scientific and medical research DOI: 192252 Open Access Full Text Article ORIGINAL RESEARCH Identification of potentially inappropriate medications with risk of major adverse cardiac and cerebrovascular events among elderly patients in ambulatory setting and long-term care facilities This article was published in the following Dove Medical Press journal: Clinical Interventions in Aging João Pedro Aguiar1 Purpose: Cardiovascular diseases (CVDs) are extremely common among the elderly, but Luís Heitor Costa2 information on the use of potentially inappropriate medications (PIMs) with cardiovascular Filipa Alves da Costa3,4 risk is scarce. We aimed to determine the prevalence of PIMs with risk of cardiac and cere- Hubert GM Leufkens5 brovascular adverse events (CCVAEs), including major adverse cardiac and cerebrovascular Ana Paula Martins1 events (MACCE). Patients and methods: A cross-sectional study was performed using a convenience sample 1Research Institute for Medicines (iMED.ULisboa), Faculdade de from four long-term care facilities and one community pharmacy in Portugal. Patients were For personal use only. Farmácia, Universidade de Lisboa, included if they were aged 65 or older and presented at least one type of medication in their 2 Lisboa, Portugal; Serviço de medical and pharmacotherapeutic records from 2015 until December 2017. The main outcome Medicina Interna, Centro Hospitalar Psiquiátrico de Lisboa (CHPL), Lisboa, was defined as the presence of PIMs with risk of MACCE and was assessed by applying a Portugal; 3Centro de Investigação PIM-MACCE list that was developed from a previous study. -

National Ribat University Institute of Forensic Evidence Sciences
National Ribat University Institute of Forensic Evidence Sciences Assessment of Trihexyphenidyl (kharsha) Knowledge and Abuse Among Students of one of Khartoum state Universities Bsc. Pharmacy,University of Science andTechnology (2005) A Thesis Submitted to National Ribat University for Partial Fulfillment of the Requirements for the Master Degree in Forensic Science Submitted By Hawari Salih AbdElrahman Supervised By Associate Prof. Ahmed AwadElgamel 2016 I Dedication I dedicate this work to my father who generously dedicated his life for us. To my dear mother that the secret of my success is her du'aa. To my wife and my beautiful children who are the joy of my life for their patience and support. To my friend Musaab for his support and endless help. HawariSalih I Acknowledgment I wish to record my thanks to all those who assisted me in the completion of this work either by support or consultation. I owe a great deal to my academic supervisor Dr.Ahmed AwadElgamel for the patience careful direction and never-ending support. II الملخ صِ بنزهكسول ِهيدروكلوريد ِ)تريهكسفينيديل(، ِيعتبراحد ِمضادات ِالكولين ِالقوية ِ ِوقد ِاكتسب ِاستخدام ِعلىِ نطاقِواسعِفيِعﻻجِمرضِالشللِالرعاشِوفيِالسيطرةِعلىِاﻵثارِالجانبيةِﻻدويةِالشللِالرعاش.ِعلىِ الرغمِمنِالتقاريرالتيِتحدثتِفيِوقتِمبكرِﻻفتةِاﻻنتباهِإلىِتاثيراتهِالنفسيةِوإمكانيةِادمانهِمنِالناحيةِ النظريةِعليِاﻻقل،ِحيثِانهِلمِيتمِاثباتهِسريرياِحتىِوقتِقريب،ِقدِلوحظِسوءِاستخدامِبنزهكسولِبوتيرةِ متزايدةِفيِالسنواتِاﻷخيرةِبينِالشبانِالساخطينِوالمحرومينِالمترددينِعلىِعياداتِالطبِالنفسي،ِوقدِ أفادوا ِأن ِاستخدامهم -

Lysergic Acid Diethylamide (LSD) Promotes Social Behavior Through Mtorc1 in the Excitatory Neurotransmission
Lysergic acid diethylamide (LSD) promotes social behavior through mTORC1 in the excitatory neurotransmission Danilo De Gregorioa,b,1, Jelena Popicb,2,3, Justine P. Ennsa,3, Antonio Inserraa,3, Agnieszka Skaleckab, Athanasios Markopoulosa, Luca Posaa, Martha Lopez-Canula, He Qianzia, Christopher K. Laffertyc, Jonathan P. Brittc, Stefano Comaia,d, Argel Aguilar-Vallese, Nahum Sonenbergb,1,4, and Gabriella Gobbia,f,1,4 aNeurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, QC, Canada, H3A 1A1; bDepartment of Biochemistry, McGill University, Montreal, QC, Canada, H3A 1A3; cDepartment of Psychology, McGill University, Montreal, QC, Canada, H3A 1B1; dDivision of Neuroscience, Vita Salute San Raffaele University, 20132 Milan, Italy; eDepartment of Neuroscience, Carleton University, Ottawa, ON, Canada, K1S 5B6; and fMcGill University Health Center, Montreal, QC, Canada, H3A 1A1 Contributed by Nahum Sonenberg, November 10, 2020 (sent for review October 5, 2020; reviewed by Marc G. Caron and Mark Geyer) Clinical studies have reported that the psychedelic lysergic acid receptor (6), but also displays affinity for the 5-HT1A receptor diethylamide (LSD) enhances empathy and social behavior (SB) in (7–9). Several studies have demonstrated that LSD modulates humans, but its mechanism of action remains elusive. Using a glutamatergic neurotransmission and, indirectly, the α-amino- multidisciplinary approach including in vivo electrophysiology, 3-hydroxy-5-methyl-4-isoxazole propionate (AMPA) receptors. optogenetics, behavioral paradigms, and molecular biology, the Indeed, in vitro studies have shown that LSD increased the ex- effects of LSD on SB and glutamatergic neurotransmission in the citatory response of interneurons in the piriform cortex following medial prefrontal cortex (mPFC) were studied in male mice.