Neurobiology of Behavioral Control in Drug Abuse
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Amnestic Concentrations of Sevoflurane Inhibit Synaptic
Anesthesiology 2008; 108:447–56 Copyright © 2008, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Amnestic Concentrations of Sevoflurane Inhibit Synaptic Plasticity of Hippocampal CA1 Neurons through ␥-Aminobutyric Acid–mediated Mechanisms Junko Ishizeki, M.D.,* Koichi Nishikawa, M.D., Ph.D.,† Kazuhiro Kubo, M.D.,‡ Shigeru Saito, M.D., Ph.D.,§ Fumio Goto, M.D., Ph.D. Background: The cellular mechanisms of anesthetic-induced for surgical procedures do not have recollection of ac- amnesia are still poorly understood. The current study exam- tually being awake despite being awake and cooperative ined sevoflurane at various concentrations in the CA1 region of during the procedure.1 Galinkin et al.2 compared sub- rat hippocampal slices for effects on excitatory synaptic trans- Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/108/3/447/366512/0000542-200803000-00017.pdf by guest on 29 September 2021 mission and on long-term potentiation (LTP), as a possible jective, psychomotor, cognitive, and analgesic effects of mechanism contributing to anesthetic-induced loss of recall. sevoflurane (0.3% and 0.6%) with those of nitrous oxide Methods: Population spikes and field excitatory postsynaptic at equal minimum alveolar concentrations (MACs) in potentials were recorded using extracellular electrodes after healthy volunteers. They found that sevoflurane pro- electrical stimulation of Schaffer-collateral-commissural fiber inputs. Paired pulse facilitation was used as a measure of pre- duced a greater degree of amnesia and psychomotor synaptic effects of the anesthetic. LTP was induced using tetanic impairment than did an equal MAC of nitrous oxide but stimulation (100 Hz, 1 s). Sevoflurane at concentrations from had no analgesic actions. -

Picrotoxin-Like Channel Blockers of GABAA Receptors
COMMENTARY Picrotoxin-like channel blockers of GABAA receptors Richard W. Olsen* Department of Molecular and Medical Pharmacology, Geffen School of Medicine, University of California, Los Angeles, CA 90095-1735 icrotoxin (PTX) is the prototypic vous system. Instead of an acetylcholine antagonist of GABAA receptors (ACh) target, the cage convulsants are (GABARs), the primary media- noncompetitive GABAR antagonists act- tors of inhibitory neurotransmis- ing at the PTX site: they inhibit GABAR Psion (rapid and tonic) in the nervous currents and synapses in mammalian neu- system. Picrotoxinin (Fig. 1A), the active rons and inhibit [3H]dihydropicrotoxinin ingredient in this plant convulsant, struc- binding to GABAR sites in brain mem- turally does not resemble GABA, a sim- branes (7, 9). A potent example, t-butyl ple, small amino acid, but it is a polycylic bicyclophosphorothionate, is a major re- compound with no nitrogen atom. The search tool used to assay GABARs by compound somehow prevents ion flow radio-ligand binding (10). through the chloride channel activated by This drug target appears to be the site GABA in the GABAR, a member of the of action of the experimental convulsant cys-loop, ligand-gated ion channel super- pentylenetetrazol (1, 4) and numerous family. Unlike the competitive GABAR polychlorinated hydrocarbon insecticides, antagonist bicuculline, PTX is clearly a including dieldrin, lindane, and fipronil, noncompetitive antagonist (NCA), acting compounds that have been applied in not at the GABA recognition site but per- huge amounts to the environment with haps within the ion channel. Thus PTX major agricultural economic impact (2). ͞ appears to be an excellent example of al- Some of the other potent toxicants insec- losteric modulation, which is extremely ticides were also radiolabeled and used to important in protein function in general characterize receptor action, allowing and especially for GABAR (1). -

Drug Class Review Newer Drugs for Insomnia
Drug Class Review Newer Drugs for Insomnia Final Update 2 Report October 2008 The Agency for Healthcare Research and Quality has not yet seen or approved this report. The purpose of Drug Effectiveness Review Project reports is to make available information regarding the comparative clinical effectiveness and harms of different drugs. Reports are not usage guidelines, nor should they be read as an endorsement of or recommendation for any particular drug, use, or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Update 1: July 2006 Original: December 2005 Susan Carson, MPH Marian S. McDonagh, PharmD Sujata Thakurta, MPA:HA Po-Yin Yen, MS Drug Effectiveness Review Project Marian McDonagh, PharmD, Principal Investigator Oregon Evidence-based Practice Center Mark Helfand, MD, MPH, Director Copyright © 2008 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 2 Drug Effectiveness Review Project The medical literature relating to the topic is scanned periodically (see http://www.ohsu.edu/xd/research/centers-institutes/evidence-based-policy- center/derp/documents/methods.cfm for scanning process description). Upon review of the last scan, the Drug Effectiveness Review Project governance group elected not to proceed with another full update of this report based on the information contained in the scan. Some portions of the report may not be up to date. Prior versions of this report can be accessed at the DERP website. Insomnia Page 2 of 87 Final Report Update 2 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION ............................................................................................................. 6 Scope and Key Questions ...................................................................................................................... -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

GABA Receptors
D Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews Review No.7 / 1-2011 GABA receptors Wolfgang Froestl , CNS & Chemistry Expert, AC Immune SA, PSE Building B - EPFL, CH-1015 Lausanne, Phone: +41 21 693 91 43, FAX: +41 21 693 91 20, E-mail: [email protected] GABA Activation of the GABA A receptor leads to an influx of chloride GABA ( -aminobutyric acid; Figure 1) is the most important and ions and to a hyperpolarization of the membrane. 16 subunits with γ most abundant inhibitory neurotransmitter in the mammalian molecular weights between 50 and 65 kD have been identified brain 1,2 , where it was first discovered in 1950 3-5 . It is a small achiral so far, 6 subunits, 3 subunits, 3 subunits, and the , , α β γ δ ε θ molecule with molecular weight of 103 g/mol and high water solu - and subunits 8,9 . π bility. At 25°C one gram of water can dissolve 1.3 grams of GABA. 2 Such a hydrophilic molecule (log P = -2.13, PSA = 63.3 Å ) cannot In the meantime all GABA A receptor binding sites have been eluci - cross the blood brain barrier. It is produced in the brain by decarb- dated in great detail. The GABA site is located at the interface oxylation of L-glutamic acid by the enzyme glutamic acid decarb- between and subunits. Benzodiazepines interact with subunit α β oxylase (GAD, EC 4.1.1.15). It is a neutral amino acid with pK = combinations ( ) ( ) , which is the most abundant combi - 1 α1 2 β2 2 γ2 4.23 and pK = 10.43. -

Exploring the Activity of an Inhibitory Neurosteroid at GABAA Receptors
1 Exploring the activity of an inhibitory neurosteroid at GABAA receptors Sandra Seljeset A thesis submitted to University College London for the Degree of Doctor of Philosophy November 2016 Department of Neuroscience, Physiology and Pharmacology University College London Gower Street WC1E 6BT 2 Declaration I, Sandra Seljeset, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I can confirm that this has been indicated in the thesis. 3 Abstract The GABAA receptor is the main mediator of inhibitory neurotransmission in the central nervous system. Its activity is regulated by various endogenous molecules that act either by directly modulating the receptor or by affecting the presynaptic release of GABA. Neurosteroids are an important class of endogenous modulators, and can either potentiate or inhibit GABAA receptor function. Whereas the binding site and physiological roles of the potentiating neurosteroids are well characterised, less is known about the role of inhibitory neurosteroids in modulating GABAA receptors. Using hippocampal cultures and recombinant GABAA receptors expressed in HEK cells, the binding and functional profile of the inhibitory neurosteroid pregnenolone sulphate (PS) were studied using whole-cell patch-clamp recordings. In HEK cells, PS inhibited steady-state GABA currents more than peak currents. Receptor subtype selectivity was minimal, except that the ρ1 receptor was largely insensitive. PS showed state-dependence but little voltage-sensitivity and did not compete with the open-channel blocker picrotoxinin for binding, suggesting that the channel pore is an unlikely binding site. By using ρ1-α1/β2/γ2L receptor chimeras and point mutations, the binding site for PS was probed. -

Toxicological and Pharmacological Profile of Amanita Muscaria (L.) Lam
Pharmacia 67(4): 317–323 DOI 10.3897/pharmacia.67.e56112 Review Article Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine Maria Voynova1, Aleksandar Shkondrov2, Magdalena Kondeva-Burdina1, Ilina Krasteva2 1 Laboratory of Drug metabolism and drug toxicity, Department “Pharmacology, Pharmacotherapy and Toxicology”, Faculty of Pharmacy, Medical University of Sofia, Bulgaria 2 Department of Pharmacognosy, Faculty of Pharmacy, Medical University of Sofia, Bulgaria Corresponding author: Magdalena Kondeva-Burdina ([email protected]) Received 2 July 2020 ♦ Accepted 19 August 2020 ♦ Published 26 November 2020 Citation: Voynova M, Shkondrov A, Kondeva-Burdina M, Krasteva I (2020) Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine. Pharmacia 67(4): 317–323. https://doi.org/10.3897/pharmacia.67. e56112 Abstract Amanita muscaria, commonly known as fly agaric, is a basidiomycete. Its main psychoactive constituents are ibotenic acid and mus- cimol, both involved in ‘pantherina-muscaria’ poisoning syndrome. The rising pharmacological and toxicological interest based on lots of contradictive opinions concerning the use of Amanita muscaria extracts’ neuroprotective role against some neurodegenerative diseases such as Parkinson’s and Alzheimer’s, its potent role in the treatment of cerebral ischaemia and other socially significant health conditions gave the basis for this review. Facts about Amanita muscaria’s morphology, chemical content, toxicological and pharmacological characteristics and usage from ancient times to present-day’s opportunities in modern medicine are presented. Keywords Amanita muscaria, muscimol, ibotenic acid Introduction rica, the genus had an ancestral origin in the Siberian-Be- ringian region in the Tertiary period (Geml et al. -
A Systematic Review of Combination and High-Dose Atypical
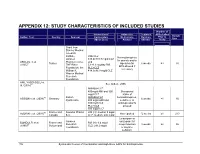
APPENDIX 12: STUDY CHARACTERISTICS OF INCLUDED STUDIES Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study Grant from Stanley Medical research Institute, RIS+CLZ Benzodiazepines Janssen 515.6±138.7 mg/d CLZ for anxiety and/or AKDEDE et al. Pharmaceutica, and 42 Turkey biperiden for 6 weeks ≥3 30 (2005) THE Ritter 5.1±1.3 mg/day RIS EPS allowed if Foundation, the PLC+CLZ necessary William K. 414.3±96.9 mg/d CLZ Warren Medical Research Foundation ANIL YAGCIOGLU et 45 See Akdede 2006 al. (2005) AMI400+CLZ 400mg/d AMI and 300 Occasional mg/d CLZ intake of 49 Sanofi- AMI600+CLZ benzodiazepines, ASSION et al. (2008) Germany 6 weeks ≥1 16 Synthelabo 600 mg/d AMI and sedatives, or 300mg/d CLZ antidepressants PLC+CLZ allowed 300 mg/d CLZ 60 France and Novartis Phama RIS (H): median 9 mg/d AZORIN et al. (2001) Not reported 12 weeks ≥1 273 Canada S.A. CLZ: median: 600 mg/d Lorazepam or Janssen oxazepam for BONDOLFI et al. France and RIS (H): 6.4 mg/d 66 Research sleep induction 8 weeks ≥2 86 (1998) Switzerland CLZ: 291.2 mg/d Foundation or daytime sedation; 156 Systematic Review of Combination and High-Dose AAPs for Schizophrenia Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study biperiden and procyclidine for EPS Supported by grants from Brain Research center, funded by the ARI+CLZ Antidepressants, Ministry of 15.5±7.1 mg/d ARI and 38 anticholinergics CHANG et al. -

CNS Drug Reviews Vol
CNS Drug Reviews Vol. 10, No. 1, pp. 45–76 © 2004 Neva Press, Branford, Connecticut Clinical Pharmacology, Clinical Efficacy, and Behavioral Toxicity of Alprazolam: A Review of the Literature Joris C. Verster and Edmund R. Volkerts Utrecht Institute for Pharmaceutical Sciences, Department of Psychopharmacology, University of Utrecht, Utrecht, The Netherlands Keywords: Alprazolam — Benzodiazepines — Anxiety — Depression — Panic — Sedation. ABSTRACT Alprazolam is a benzodiazepine derivative that is currently used in the treatment of generalized anxiety, panic attacks with or without agoraphobia, and depression. Alprazo- lam has a fast onset of symptom relief (within the first week); it is unlikely to produce de- pendency or abuse. No tolerance to its therapeutic effect has been reported. At discontinu- ation of alprazolam treatment, withdrawal and rebound symptoms are common. Hence, alprazolam discontinuation must be tapered. An exhaustive review of the literature showed that alprazolam is significantly superior to placebo, and is at least equally effective in the relief of symptoms as tricyclic antide- pressants (TCAs), such as imipramine. However, although alprazolam and imipramine are significantly more effective than placebo in the treatment of panic attacks, Selective Sero- tonin Reuptake Inhibitors (SSRIs) appear to be superior to either of the two drugs. Therefore, alprazolam is recommended as a second line treatment option, when SSRIs are not effective or well tolerated. In addition to its therapeutic effects, alprazolam produces adverse effects, such as drowsiness and sedation. Since alprazolam is widely used, many clinical studies investi- gated its cognitive and psychomotor effects. It is evident from these studies that alprazo- lam may impair performance in a variety of skills in healthy volunteers as well as in pa- tients. -

Partial Agreement in the Social and Public Health Field
COUNCIL OF EUROPE COMMITTEE OF MINISTERS (PARTIAL AGREEMENT IN THE SOCIAL AND PUBLIC HEALTH FIELD) RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies, and superseding Resolution AP (82) 2) AND APPENDIX I Alphabetical list of medicines adopted by the Public Health Committee (Partial Agreement) updated to 1 July 1988 APPENDIX II Pharmaco-therapeutic classification of medicines appearing in the alphabetical list in Appendix I updated to 1 July 1988 RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (superseding Resolution AP (82) 2) (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies) The Representatives on the Committee of Ministers of Belgium, France, the Federal Republic of Germany, Italy, Luxembourg, the Netherlands and the United Kingdom of Great Britain and Northern Ireland, these states being parties to the Partial Agreement in the social and public health field, and the Representatives of Austria, Denmark, Ireland, Spain and Switzerland, states which have participated in the public health activities carried out within the above-mentioned Partial Agreement since 1 October 1974, 2 April 1968, 23 September 1969, 21 April 1988 and 5 May 1964, respectively, Considering that the aim of the Council of Europe is to achieve greater unity between its members and that this -

In the Treatment of Generalised Anxiety Disorder Does Pharmacology
Characteristics Table for The Clinical Question: In the treatment of generalised anxiety disorder does 6/18/2010 12:21:10 pharmacology improve outcome? Comparisons Included in this Clinical Question Anticonvulsants versus Placebo Anticonvulsants vs Venlafaxine (SNRI) Antihistamine vs Placebo Benzodiazepines versus vs Placebo Anticonvulsants FELTNER2003 DARCIS1995 KASPER2009 KASPER2009 LADER1998 FELTNER2003 MONTGOMERY2006 MONTGOMERY2006 LLORCA2002 PANDE2003 MONTGOMERY2008 PFIZER2005 PANDE2003 RICKELS2005 PFIZER2005 POHL2005 RICKELS2005 Benzodiazepines versus Azapirones Benzodiazepines versus Placebo Buspirone vs Placebo Duloxetine (SNRI) vs. placebo BOURIN1992 ANDREATINI2002 DAVIDSON1999 HARTFORD2007 ANSSEAU2001 LADER1998 KOPONEN2007 CUTLER1993A MAJERCSIK2003 NICOLINI2009 FELTNER2003 POLLACK1997 RYNN2008 FRESQUET2000 SRAMEK1996 HACKETT2003 LYDIARD1997 MCLEOD1992 MOLLER2001 PANDE2003 PFIZER2008 RICKELS2000B RICKELS2005 Duloxetine (SNRI) vs. Venlafaxine Quetiapine versus Placebo SSRI vs Venlafaxine SSRIs versus Placebo (SNRI) ASTRAZENECA2007A BOSE2008 ALLGULANDER2004 HARTFORD2007 ASTRAZENECA2007B ASTRAZENECA2007A NICOLINI2009 ASTRAZENECA2007C ASTRAZENECA2007B ASTRAZENECA2008 BALDWIN2006 BOSE2008 BRAWMAN-MINTZER2006 DAVIDSON2004 GOODMAN2005 GSK2002 GSK2005 HEWETT2001 LENZE2005 LENZE2009 PFIZER2008 POLLACK2001 RICKELS2003 SSRIs versus SSRIs TCA vs Placebo Venlafaxine (SNRI) versus Azapirones Venlafaxine (SNRI) versus placebo BALDWIN2006 MCLEOD1992 DAVIDSON1999 ALLGULANDER2001 BALL2005 BOSE2008 BIELSKI2005 DAVIDSON1999 GELENBERG2000 HACKETT2003 -

Bicuculline and Gabazine Are Allosteric Inhibitors of Channel Opening of the GABAA Receptor
The Journal of Neuroscience, January 15, 1997, 17(2):625–634 Bicuculline and Gabazine Are Allosteric Inhibitors of Channel Opening of the GABAA Receptor Shinya Ueno,1 John Bracamontes,1 Chuck Zorumski,2 David S. Weiss,3 and Joe Henry Steinbach1 Departments of 1Anesthesiology and 2Psychiatry, Washington University School of Medicine, St. Louis, Missouri 63110, and 3University of Alabama at Birmingham, Neurobiology Research Center and Department of Physiology and Biophysics, Birmingham, Alabama 35294-0021 Anesthetic drugs are known to interact with GABAA receptors, bicuculline only partially blocked responses to pentobarbital. both to potentiate the effects of low concentrations of GABA and These observations indicate that the blockers do not compete to directly gate open the ion channel in the absence of GABA; with alphaxalone or pentobarbital for a single class of sites on the however, the site(s) involved in direct gating by these drugs is not GABAA receptor. Finally, at receptors containing a1b2(Y157S)g2L known. We have studied the ability of alphaxalone (an anesthetic subunits, both bicuculline and gabazine showed weak agonist steroid) and pentobarbital (an anesthetic barbiturate) to directly activity and actually potentiated responses to alphaxalone. These activate recombinant GABAA receptors containing the a1, b2, and observations indicate that the blocking drugs can produce allo- g2L subunits. Steroid gating was not affected when either of two steric changes in GABAA receptors, at least those containing this mutated b2 subunits [b2(Y157S) and b2(Y205S)] are incorporated mutated b2 subunit. We conclude that the sites for binding ste- into the receptors, although these subunits greatly reduce the roids and barbiturates do not overlap with the GABA-binding site.