Comparison of the Effects of Metformin and Goserelin in Patients with Polycystic Ovary Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

Altered Cognitive Function in Men Treated for Prostate
Altered Cognitive Function in Men Treated for Prostate Cancer with LHRH Analogues and Cyproterone Acetate: A Randomised Controlled Trial H. J. Green PhD1,2, K. I. Pakenham PhD1, B. C. Headley PhD3, J. Yaxley FRACS3, D. L. Nicol FRACS2,4, P. N. Mactaggart FRACS2,5, C. Swanson PhD2, R. B. W atson FRACS6, & R. A. Gardiner MD2,3 1School of Psychology and 2Department of Surgery, The University of Queensland, 3Royal Brisbane, 4Princess Alexandra, 5Queen Elizabeth II & 6Mater Hospitals, Brisbane, Queensland, Australia In conjunction with the Northern Section of the Urological Society of Australasia Correspondence should be addressed to: Dr R. A. Gardiner, Department of Surgery, The University of Queensland, Brisbane, Qld 4072, Australia Fax: +61 7 3365 5559; Phone: +61 7 3365 5233; Email: f.gardiner@ mailbox.uq.edu.au This work was wholly funded by Queensland Cancer Fund. **PREPRINT. Final version published in British Journal of Urology (BJU: International) (2002), 90, 427-432 ** Short Title: COGNITIVE CHANGES W ITH HORMONAL MEDICATION 2 Objective. Luteinising hormone releasing hormone (LHRH) analogues have been associated with memory impairments in women using these drugs for gynaecological conditions. This is the first systematic investigation of the cognitive effects of LHRH analogues in male patients. Methods. 82 men with non-localised prostate cancer were randomly assigned to receive continuous leuprorelin (LHRH analogue), goserelin (LHRH analogue), cyproterone acetate (steroidal antiandrogen) or close clinical monitoring. These patients underwent cognitive assessments at baseline and before commencement of treatment (77) then 6 months later (65). Results. Compared with baseline assessments, men administered androgen suppression monotherapy performed worse in 2/12 tests of attention and memory. -

Goserelin (Zoladex)
Goserelin (Zoladex) This booklet explains what goserelin is, when it may be prescribed, how it works and what side effects may occur. Goserelin is the generic (non‑branded) name of the drug and how it’s referred to in this booklet. Its current brand name is Zoladex. This information is by Breast Cancer Care. We are the only specialist UK‑wide charity that supports people affected by breast cancer. We’ve been supporting them, their family and friends and campaigning on their behalf since 1973. Today, we continue to offer reliable information and personal support, over the phone and online, from nurses and people who’ve been there. We also offer local support across the UK. From the moment you notice something isn’t right, through to treatment and beyond, we’re here to help you feel more in control. For breast cancer care, support and information, call us free on 0808 800 6000 or visit breastcancercare.org.uk Visit breastcancercare.org.uk 3 What is goserelin? Goserelin is a type of hormone therapy used to treat breast cancer in pre-menopausal women (women who have not been through the menopause). It is given as an injection into the abdomen (belly). It can also be used to try to preserve fertility during chemotherapy (see page 4). Goserelin as a treatment for breast cancer How does it work? Some breast cancers are stimulated to grow by the hormone oestrogen. Before the menopause, oestrogen is mainly produced in the ovaries. Goserelin switches off this production by interfering with hormone signals from the brain that control how the ovaries work. -
Triptorelin, Goserelin and Leuprorelin for Prostate
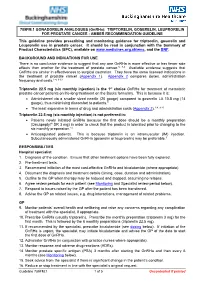
789FM.1 GONADORELIN ANALOGUES (GnRHa): TRIPTORELIN, GOSERELIN, LEUPRORELIN FOR PROSTATE CANCER - AMBER RECOMMENDATION GUIDELINE This guideline provides prescribing and monitoring guidance for triptorelin, goserelin and Leuprorelin use in prostate cancer. It should be read in conjunction with the Summary of Product Characteristics (SPC), available on www.medicines.org.uk/emc, and the BNF. BACKGROUND AND INDICATIONS FOR USE There is no conclusive evidence to suggest that any one GnRHa is more effective or has fewer side effects than another for the treatment of prostate cancer.5, 7-9 Available evidence suggests that GnRHa are similar in effectiveness to surgical castration. They have the same licensed indications in the treatment of prostate cancer (Appendix 1). Appendix 2 compares doses, administration frequency and costs.1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is the 1st choice GnRHa for treatment of metastatic prostate cancer patients on life-long treatment on the Bucks formulary. This is because it is: • Administered via a smaller sized needle (20 gauge) compared to goserelin LA 10.8 mg (14 gauge), thus minimising discomfort to patients.9 • The least expensive in terms of drug and administration costs (Appendix 2).1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is not preferred in: • Patients newly initiated GnRHa because the first dose should be a monthly preparation (Decapeptyl® SR 3 mg) in order to check that the product is tolerated prior to changing to the six monthly preparation.14 • Anticoagulated patients. This is because triptorelin is an intramuscular (IM) injection. Subcutaneously administered GnRHa (goserelin or leuprorelin) may be preferable.9 RESPONSIBILITIES Hospital specialist 1. -

Luteinising Hormone-Releasing Hormone (LHRH) Agonists in Prostate Cancer This Bulletin Focuses on Luteinising Hormone-Releasing Hormone (LHRH) Agonists
B88 | April 2015 | 2.1 Community Interest Company Luteinising hormone-releasing hormone (LHRH) agonists in prostate cancer This bulletin focuses on luteinising hormone-releasing hormone (LHRH) agonists. Currently goserelin and leuprorelin (administered 4 weekly or 12 weekly and monthly or 3 monthly respectively) are the two LHRH agonists used primarily in the management of prostate cancer across England (88% share, ePACT October to December 2014). Triptorelin is also used for prostate cancer and has published data to confirm its efficacy. However triptorelin only accounts for 12% (ePACT October to December 2014) of all LHRH agonist usage. Across England, a switch from 12 weekly goserelin and 3 monthly leuprorelin to 12 weekly or 6 monthly triptorelin could result in an annual saving of £6.8 million (ePACT October to December 2014). Support materials (including the secondary care bulletin: Bulletin 28 Secondary care KPI support bulletins. Gonadorelin analogues – reduced usage of Zoladex) are available at http://www.prescqipp.info Recommendations • Engage and establish opinion with local Trust urologists on preferred formulary choices of LHRH agonists. This should take into account dosage intervals, administration, product price, and fees paid for administration. Local decision making may also be affected by local discounts and rebate scheme activity. • 3 monthly and 6 monthly triptorelin and 3 monthly leuprorelin are the preferred cost effective LHRH agonists for prostate cancer in new patients. • Switch guidance will need to be agreed by local Trust urologists for existing patients and should be considered at the next clinic appointment. • Use 12 weekly/3 monthly or 6 monthly injections in preference to 4 weekly/monthly injections to support administration, convenience to the patient and costs. -

Gonadotropin-Releasing Hormone Antagonists Versus Standard Androgen Suppression Therapy for Advanced Prostate Cancer a Systematic Review with Meta-Analysis
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2015-008217 on 13 November 2015. Downloaded from Gonadotropin-releasing hormone antagonists versus standard androgen suppression therapy for advanced prostate cancer A systematic review with meta-analysis Frank Kunath,1,2 Hendrik Borgmann,2,3 Anette Blümle,4 Bastian Keck,1 Bernd Wullich,1,2 Christine Schmucker,4 Danijel Sikic,1 Catharina Roelle,1 Stefanie Schmidt,2 Amr Wahba,5 Joerg J Meerpohl4 To cite: Kunath F, ABSTRACT et al Strengths and limitations of this study Borgmann H, Blümle A, . Objectives: To evaluate efficacy and safety of Gonadotropin-releasing gonadotropin-releasing hormone (GnRH) antagonists ▪ hormone antagonists versus We searched CENTRAL, MEDLINE, Web of compared to standard androgen suppression therapy standard androgen Science, EMBASE, trial registries and conference suppression therapy for for advanced prostate cancer. books. Two authors independently screened advanced prostate cancer A Setting: The international review team included identified articles, extracted data, evaluated risk systematic review with meta- methodologists of the German Cochrane Centre and of bias and rated quality of evidence according analysis. BMJ Open 2015;5: clinical experts. to GRADE. e008217. doi:10.1136/ Participants: We searched CENTRAL, MEDLINE, Web ▪ There were no statistically significant differences bmjopen-2015-008217 of Science, EMBASE, trial registries and conference in overall mortality, treatment failure, or prostate- books for randomised controlled trials (RCT) for specific antigen progression and no study ▸ Prepublication history for effectiveness data analysis, and randomised or non- reported cancer-specific survival or clinical this paper is available online. randomised controlled studies (non-RCT) for safety progression. To view these files please data analysis (March 2015). -

Shared Care Guideline Gonadorelin Analogues
SHARED CARE GUIDELINE GONADORELIN ANALOGUES INTRODUCTION Metastatic cancer of the Prostate usually responds to hormonal treatments aimed at androgen depletion. Gonadorelin analogues such as Goserelin and Leuprorelin may be given. During the initial stages of treatment with a gonadorelin analogue, it can cause tumour ‘flare’ which may lead to spinal cord compression, ureteric obstruction or increased bone pain. It is therefore important that the first injection is covered by an appropriate anti-androgen. INDICATIONS GOSERELIN ( Zoladex ) LEUPRORELIN ACETATE ( Prostap ) Goserelin is indicated in the management of Leuprorelin Acetate is indicated for the treatment of Prostate cancer suitable for hormonal advanced prostatic cancer. manipulation. Available as: Available as: Goserelin 3.6mg depot injection Leuprorelin Acetate (Prostap SR) 3.7mg depot injection Goserelin LA 10.8mg depot injection Leuprorelin Acetate (Prostap 3) 11.25mg depot injection DOSE AND ADMINISTRATION GOSERELIN ( Zoladex ) LEUPRORELIN ACETATE ( Prostap ) Goserelin 3.6mg depot injected subcutaneously Leuprorelin 3.75mg injection by subcutaneous into the anterior wall, every 28 days or or intramuscular injection every 4 weeks or goserelin LA 10.8mg depot injected Leuprorelin 11.25mg subcutaneously every 12 subcutaneously every 12 weeks. weeks. No dosage adjustment is necessary for patients with renal or hepatic impairment or in the elderly CONTRA-INDICATIONS • Gonadorelin analogues should not be given to patients with a known hypersensitivity to either goserelin or leuprorelin or to other luteinizing hormone releasing hormone ( LHRH ) analogues. • Pregnancy and lactation. SHARED CARE GUIDELINE SPECIAL WARNINGS AND PRECAUTIONS FOR USE The potential risk of developing ureteric obstruction or spinal cord compression should be considered and the patients should be monitored during the first month. -

Prior Authorization Gonadotropin-Releasing Hormone Agonists Implant - Zoladex® (Goserelin Acetate Subcutaneous Implant)
Cigna National Formulary Coverage Policy Prior Authorization Gonadotropin-Releasing Hormone Agonists Implant - Zoladex® (goserelin acetate subcutaneous implant) Table of Contents Product Identifer(s) National Formulary Medical Necessity ................ 1 66292 Conditions Not Covered....................................... 2 Background .......................................................... 2 References .......................................................... 3 Revision History ................................................... 3 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the Coverage Policies. In the absence of a controlling federal or state coverage mandate, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of 1) the terms of the applicable benefit plan document in effect on the date of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including Coverage Policies and; 4) the specific facts of the particular situation. -

Controversies in the Management of Advanced Prostate Cancer
British Journal of Cancer (1999) 79(1), 146–155 © 1999 Cancer Research Campaign Controversies in the management of advanced prostate cancer CJ Tyrrell Oncology Research Unit, Derriford Hospital, Plymouth, UK Summary For advanced prostate cancer, the main hormone treatment against which other treatments are assessed is surgical castration. It is simple, safe and effective, however it is not acceptable to all patients. Medical castration by means of luteinizing hormone-releasing hormone (LH-RH) analogues such as goserelin acetate provides an alternative to surgical castration. Diethylstilboestrol, previously the only non-surgical alternative to orchidectomy, is no longer routinely used. Castration reduces serum testosterone by around 90%, but does not affect androgen biosynthesis in the adrenal glands. Addition of an anti-androgen to medical or surgical castration blocks the effect of remaining testosterone on prostate cells and is termed combined androgen blockade (CAB). CAB has now been compared with castration alone (medical and surgical) in numerous clinical trials. Some trials show advantage of CAB over castration, whereas others report no significant difference. The author favours the view that CAB has an advantage over castration. No study has reported that CAB is less effective than castration. Of the anti-androgens which are available for use in CAB, bicalutamide may be associated with a lower incidence of side-effects compared with the other non-steroidal anti-androgens and, in common with nilutamide, has the advantage of once-daily dosing. Only one study has compared anti-androgens within CAB: bicalutamide plus LH-RH analogue and flutamide plus LH-RH analogue. At 160- week follow-up, the groups were equivalent in terms of survival and time to progression. -

Tutorial Article Management of the Transition Period: Hormone Therapy P
EQUINE VETERINARY EDUCATION / AE / MAY 2007 215 Tutorial Article Management of the transition period: hormone therapy P. M . M CCUE*, N. L. LOGAN AND C. MAGEE Equine Reproduction Laboratory, Colorado State University, Fort Collins, Colorado 80523, USA. Keywords: horse; equine transition; hormone therapy; reproduction Introduction TABLE 1: Medications and dosage regimens that have been used in the management of transitional mares Economic pressures exist in the broodmare industry to produce Medication Brand name Dosage foals early in the year. Consequently, owners want to begin breeding mares in North America by the middle of February at Altrenogest Regumate 0.044 mg/kg bwt, per os, a time when fertile matings are prevented by the seasonal s.i.d. absence of follicular activity. Exposure of mares to an artificial Buserelin (GnRH agonist) Compounded 10–100 µg, i.m. or subcut., b.i.d. photoperiod is the most common and predictable technique Deslorelin (GnRH agonist) Ovuplant 2.1 mg, subcut. implant used to induce follicular development early in the year. Deslorelin (GnRH agonist) Compounded 125 µg, i.m., b.i.d. However, light therapy does not work in all situations. Improper Domperidone Equidone 1.1 mg/kg bwt, per os, s.i.d. or inappropriate use of phototherapy may limit efficacy, and Equine FSH eFSH 6.25–12.5 mg, i.m., b.i.d. GnRH (native) LHRH a) 2–50 µg/h, subcut., not all mares respond to light therapy by ovulating early in the pulsatile or continuous season. In addition, many mares are not maintained under infusion lights in the winter months and yet owners still want them bred b) 50–500 µg, i.m., b.i.d.