Goserelin Versus Leuprolide in the Chemical Castration of Patients with Prostate Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

LHRH) Antagonist Cetrorelix and LHRH Agonist Triptorelin on the Gene Expression of Pituitary LHRH Receptors in Rats
Comparison of mechanisms of action of luteinizing hormone-releasing hormone (LHRH) antagonist cetrorelix and LHRH agonist triptorelin on the gene expression of pituitary LHRH receptors in rats Magdolna Kovacs*†‡ and Andrew V. Schally*†§ *Endocrine, Polypeptide, and Cancer Institute, Veterans Affairs Medical Center, New Orleans, LA 70112; and †Section of Experimental Medicine, Department of Medicine, Tulane University School of Medicine, New Orleans, LA 70112 Contributed by Andrew V. Schally, August 21, 2001 The mechanisms through which luteinizing hormone (LH)-releasing however, are different. LHRH agonists achieve the inhibition of hormone (LHRH) antagonists suppress pituitary gonadotroph func- gonadotropin secretion after a period of continuous exposure (1, tions and LHRH-receptor (LHRH-R) expression are incompletely un- 2, 11–14). In contrast, antagonists of LHRH produce a compet- derstood. Consequently, we investigated the direct effect of LHRH itive blockade of LHRH-R and cause an immediate cessation of antagonist cetrorelix in vitro on the expression of the pituitary the release of gonadotropins and sex steroids, reducing the time LHRH-R gene and its ability to counteract the exogenous LHRH and of the onset of therapeutic effects as compared with the agonists the agonist triptorelin in the regulation of this gene. We also com- (1, 2, 15–17). LHRH agonists such as triptorelin, leuprolide, pared the effects of chronic administration of cetrorelix and triptore- buserelin, or goserelin (1, 2, 14) have been used worldwide for lin on the LHRH-R mRNA level and gonadotropin secretion in ovari- nearly two decades, but LHRH antagonists such as cetrorelix, ectomized (OVX) and normal female rats. The exposure of pituitary ganirelix, and Abarelix have been introduced into the clinical cells in vitro to 3-min pulses of 1 nM LHRH or 0.1 nM triptorelin for 5 h practice relatively recently (1, 2, 15, 16). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -
Personalized ADT
Personalized ADT Thomas Keane MD Conflicts • Ferring • Tolemar • Bayer • Astellas • myriad Personalized ADT for the Specific Paent • Cardiac • OBesity and testosterone • Fsh • High volume metastac disease • Docetaxol • Significant LUTS Cardiovascular risk profile and ADT Is there a difference? Degarelix Belongs to a class of synthe@c drug, GnRH antagonist (Blocker) GnRH pGlu His Trp Ser Tyr Gly Leu Arg Pro Gly NH2 Leuprolide D-Leu NEt Goserelin D-Ser NH2 LHRH agonists Triptorelin D-Trp NH2 Buserelin D-Ser NEt Degarelix D-NaI D-Cpa D-PaI Aph D-Aph D-Ala NH2 N-Me ABarelix D-NaI D-Cpa D-PaI D-Asn Lys D-Ala NH2 Tyr GnRH antagonists Cetrorelix D-NaI D-Cpa D-PaI D-Cit D-Ala NH2 Ganirelix D-NaI D-CPa D-PaI D-hArg D-hArg D-Ala NH2 Millar RP, et al. Endocr Rev 2004;25:235–75 Most acute CVD events are caused By rupture of a vulnerable atherosclero@c plaque The vulnerable plaque – thin cap with inflammaon Inflammation Plaque instability is at the heart of cardiovascular disease Stable plaque Vulnerable plaque Lumen Lumen Lipid core Lipid core FiBrous cap FiBrous cap Thick Cap Thin Rich in SMC and matrix Composion Rich in inflammatory cells: proteoly@c ac@vity Poor Lipid Rich Inflammatory Inflammatory state Highly inflammatory LiBBy P. Circulaon 1995;91:2844-2850 Incidence of Both prostate cancer and CV events is highest in older men Prostate cancer CV events 3500 3500 Prostate cancer All CV disease Major CV events 3000 3000 2827.1 2500 2500 2338.9 2000 2000 1719.7 1500 1500 1152.6 1008.7 1038.7 1000 1000 641.2 545.2 571.1 Age-specific incidence per 100,000 person-years 500 500 246.9 133.7 4.3 0 0 40-49 50-59 60-69 70-79 80-89 90-99 40-49 50-59 60-69 70-79 80-89 90-99 CV, cardiovascular Major CV events = myocardial infarc@on, stroke, or death due to CV disease All CV disease = major CV events + self-reported angina or revascularisaon procedures Driver, et al. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

Altered Cognitive Function in Men Treated for Prostate
Altered Cognitive Function in Men Treated for Prostate Cancer with LHRH Analogues and Cyproterone Acetate: A Randomised Controlled Trial H. J. Green PhD1,2, K. I. Pakenham PhD1, B. C. Headley PhD3, J. Yaxley FRACS3, D. L. Nicol FRACS2,4, P. N. Mactaggart FRACS2,5, C. Swanson PhD2, R. B. W atson FRACS6, & R. A. Gardiner MD2,3 1School of Psychology and 2Department of Surgery, The University of Queensland, 3Royal Brisbane, 4Princess Alexandra, 5Queen Elizabeth II & 6Mater Hospitals, Brisbane, Queensland, Australia In conjunction with the Northern Section of the Urological Society of Australasia Correspondence should be addressed to: Dr R. A. Gardiner, Department of Surgery, The University of Queensland, Brisbane, Qld 4072, Australia Fax: +61 7 3365 5559; Phone: +61 7 3365 5233; Email: f.gardiner@ mailbox.uq.edu.au This work was wholly funded by Queensland Cancer Fund. **PREPRINT. Final version published in British Journal of Urology (BJU: International) (2002), 90, 427-432 ** Short Title: COGNITIVE CHANGES W ITH HORMONAL MEDICATION 2 Objective. Luteinising hormone releasing hormone (LHRH) analogues have been associated with memory impairments in women using these drugs for gynaecological conditions. This is the first systematic investigation of the cognitive effects of LHRH analogues in male patients. Methods. 82 men with non-localised prostate cancer were randomly assigned to receive continuous leuprorelin (LHRH analogue), goserelin (LHRH analogue), cyproterone acetate (steroidal antiandrogen) or close clinical monitoring. These patients underwent cognitive assessments at baseline and before commencement of treatment (77) then 6 months later (65). Results. Compared with baseline assessments, men administered androgen suppression monotherapy performed worse in 2/12 tests of attention and memory. -

Goserelin (Zoladex)
Goserelin (Zoladex) This booklet explains what goserelin is, when it may be prescribed, how it works and what side effects may occur. Goserelin is the generic (non‑branded) name of the drug and how it’s referred to in this booklet. Its current brand name is Zoladex. This information is by Breast Cancer Care. We are the only specialist UK‑wide charity that supports people affected by breast cancer. We’ve been supporting them, their family and friends and campaigning on their behalf since 1973. Today, we continue to offer reliable information and personal support, over the phone and online, from nurses and people who’ve been there. We also offer local support across the UK. From the moment you notice something isn’t right, through to treatment and beyond, we’re here to help you feel more in control. For breast cancer care, support and information, call us free on 0808 800 6000 or visit breastcancercare.org.uk Visit breastcancercare.org.uk 3 What is goserelin? Goserelin is a type of hormone therapy used to treat breast cancer in pre-menopausal women (women who have not been through the menopause). It is given as an injection into the abdomen (belly). It can also be used to try to preserve fertility during chemotherapy (see page 4). Goserelin as a treatment for breast cancer How does it work? Some breast cancers are stimulated to grow by the hormone oestrogen. Before the menopause, oestrogen is mainly produced in the ovaries. Goserelin switches off this production by interfering with hormone signals from the brain that control how the ovaries work. -
Triptorelin, Goserelin and Leuprorelin for Prostate
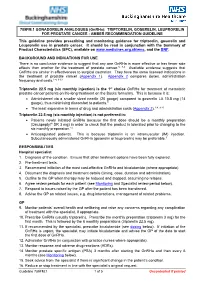
789FM.1 GONADORELIN ANALOGUES (GnRHa): TRIPTORELIN, GOSERELIN, LEUPRORELIN FOR PROSTATE CANCER - AMBER RECOMMENDATION GUIDELINE This guideline provides prescribing and monitoring guidance for triptorelin, goserelin and Leuprorelin use in prostate cancer. It should be read in conjunction with the Summary of Product Characteristics (SPC), available on www.medicines.org.uk/emc, and the BNF. BACKGROUND AND INDICATIONS FOR USE There is no conclusive evidence to suggest that any one GnRHa is more effective or has fewer side effects than another for the treatment of prostate cancer.5, 7-9 Available evidence suggests that GnRHa are similar in effectiveness to surgical castration. They have the same licensed indications in the treatment of prostate cancer (Appendix 1). Appendix 2 compares doses, administration frequency and costs.1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is the 1st choice GnRHa for treatment of metastatic prostate cancer patients on life-long treatment on the Bucks formulary. This is because it is: • Administered via a smaller sized needle (20 gauge) compared to goserelin LA 10.8 mg (14 gauge), thus minimising discomfort to patients.9 • The least expensive in terms of drug and administration costs (Appendix 2).1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is not preferred in: • Patients newly initiated GnRHa because the first dose should be a monthly preparation (Decapeptyl® SR 3 mg) in order to check that the product is tolerated prior to changing to the six monthly preparation.14 • Anticoagulated patients. This is because triptorelin is an intramuscular (IM) injection. Subcutaneously administered GnRHa (goserelin or leuprorelin) may be preferable.9 RESPONSIBILITIES Hospital specialist 1. -

Recent Development of Non-Peptide Gnrh Antagonists
Review Recent Development of Non-Peptide GnRH Antagonists Feng-Ling Tukun 1, Dag Erlend Olberg 1,2, Patrick J. Riss 2,3,4, Ira Haraldsen 4, Anita Kaass 5 and Jo Klaveness 1,* 1 School of Pharmacy, University of Oslo, 0316 Oslo, Norway; [email protected] (F.-L.T.); [email protected] (D.E.O.) 2 Norsk Medisinsk Syklotronsenter AS, Postboks 4950 Nydalen, 0424 Oslo, Norway; [email protected] 3 Realomics SFI, Department of Chemistry, University of Oslo, 0316 Oslo, Norway 4 Department of neuropsychiatry and psychosomatic medicine, Oslo University Hospital, 4950 Oslo, Norway; [email protected] 5 Betanien Hospital, 3722 Skien, Norway; [email protected] * Correspondence: [email protected]; Tel.: +47-9177-6204 Received: 16 November 2017; Accepted: 4 December 2017; Published: 9 December 2017 Abstract: The decapeptide gonadotropin-releasing hormone, also referred to as luteinizing hormone-releasing hormone with the sequence (pGlu-His-Trp-Ser-Tyr-Gly-Leu-Arg-Pro-Gly-NH2) plays an important role in regulating the reproductive system. It stimulates differential release of the gonadotropins FSH and LH from pituitary tissue. To date, treatment of hormone-dependent diseases targeting the GnRH receptor, including peptide GnRH agonist and antagonists are now available on the market. The inherited issues associate with peptide agonists and antagonists have however, led to significant interest in developing orally active, small molecule, non-peptide antagonists. In this review, we will summarize all developed small molecule GnRH antagonists along with the most recent clinical data and therapeutic applications. Keywords: GnRH receptor; non-peptide GnRH antagonist 1. -

WO 2009/137104 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 12 November 2009 (12.11.2009) WO 2009/137104 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/137 (2006.01) A61K 31/5685 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/138 (2006.01) A61P 35/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, A61K 31/4196 (2006.01) CA, CH, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, (21) International Application Number: HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, PCT/US2009/002885 KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, (22) International Filing Date: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, 7 May 2009 (07.05.2009) NZ, OM, PG, PH, PL, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, TZ, UA, (25) Filing Language: English UG, US, UZ, VC, VN, ZA, ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/127,025 9 May 2008 (09.05.2008) US GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, (71) Applicant (for all designated States except US): RA¬ TM), European (AT, BE, BG, CH, CY, CZ, DE, DK, EE, DIUS HEALTH, INC. -

April 16,2004 Steve E. Phurrough, MD, MPA Office of Clinical Standards & Quality Centers for Medicare and Medicaid Services
April 16,2004 Steve E. Phurrough, MD, MPA Office of Clinical Standards & Quality Centers for Medicare and Medicaid Services 7500 Security Boulevard Mail Stop C1-09-06 Baltimore, MD 21244-1850 Dear Dr. Phurrough: This is a formal request for a national coverage determination ("NCD") on the use of Plenaxis™ (abarelix for injectable suspension) under the Medicare program. This request is being made pursuant to NCD development Track #1 - Requests for New National Coverage Determinations Initiated by Any Party, Including Beneficiaries, Manufacturers, Providers, or Suppliers. We believe that Plenaxis meets the qualifications for coverage in the Medicare benefit category of "drugs or biologicals," as defined under § 1861(t)(1) of the Social Security Act. Plenaxis (abarelix for injectable suspension) is a synthetic decapeptide with potent antagonistic activity against naturally occurring gonadotropin releasing-hormones (GnRH). It is the only GnRH antagonist ever to have been approved by the Food and Drug Administration ("FDA") as a treatment for prostate cancer. Specifically, Plenaxis was first approved by FDA on November 25, 2003 for the palliative treatment of men with advanced symptomatic prostate cancer, in whom LHRH agonist therapy is not appropriate and who refuse surgical castration, and have one or more of the following: (1) risk of neurological compromise due to metastases, (2) ureteral or bladder outlet obstruction due to local encroachment or metastatic disease, or (3) severe bone pain from skeletal metastases persisting on narcotic analgesia. On March 31, 2004, Plenaxis was approved for inclusion in the United States Pharmacopeia Drug Information.® Enclosed you will find three copies of a two compact disc ("CD") set containing the supporting documentation for this NCD request. -

214621Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 214621Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA/BLA Multi-disciplinary Review and Evaluation: NDA 214, 621 Relugolix NDA/BLA Multi-disciplinary Review and Evaluation Disclaimer: In this document, the sections labeled as “The Applicant’s Position” are completed by the Applicant, which do not necessarily reflect the positions of the FDA. Application Type NDA Application Number(s) NDA 214621 Priority or Standard Priority Submit Date(s) April 20, 2020 Received Date(s) April 20, 2020 PDUFA Goal Date December 20, 2020 Division/Office OND/CDER/OOD/DO1 Review Completion Date Established Name Relugolix (b) (4) (Proposed) Trade Name Pharmacologic Class Gonadotropin-releasing hormone (GnRH) receptor antagonist Code name TAK-385 Applicant Myovant Sciences, Inc. Formulation(s) oral tablet Dosing Regimen One time loading dose of 360 mg followed by 120 mg daily Applicant Proposed RELUGOLIX is a gonadotropin-releasing hormone Indication(s)/Population(s) (GnRH) antagonist indicated for the treatment of patients with advanced prostate cancer. Recommendation on Regular approval Regulatory Action Recommended RELUGOLIX is a gonadotropin-releasing hormone Indication(s)/Population(s) (GnRH) antagonist indicated for the treatment of (if applicable) patients with advanced prostate cancer. 1 Version date: January 2020 (ALL NDA/ BLA reviews) Disclaimer: In this document, the sections labeled as “The Applicant’s Position” are completed by the Applicant and do not necessarily reflect the positions of the FDA. Reference ID: 4719259 NDA/BLA Multi-disciplinary Review and Evaluation: NDA 214, 621 Relugolix Table of Contents Reviewers of Multi-Disciplinary Review and Evaluation ..................................................