Effect of Perinatal Alcohol Exposure on Ibotenic Acid-Induced Excitotoxic Cortical Lesions in Newborn Hamsters
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tetrodotoxin
Niharika Mandal et al. / Journal of Pharmacy Research 2012,5(7),3567-3570 Review Article Available online through ISSN: 0974-6943 http://jprsolutions.info Tetrodotoxin: An intriguing molecule Niharika Mandal*, Samanta Sekhar Khora, Kanagaraj Mohanapriya, and Soumya Jal School of Biosciences and Technology, VIT University, Vellore-632013 Tamil Nadu, India Received on:07-04-2012; Revised on: 12-05-2012; Accepted on:16-06-2012 ABSTRACT Tetrodotoxin (TTX) is one of the most potent neurotoxin of biological origin. It was first isolated from puffer fish and it has been discovered in various arrays of organism since then. Its origin is still unclear though some reports indicate towards microbial origin. TTX selectively blocks the sodium channel, inhibiting action potential thereby, leading to respiratory paralysis. TTX toxicity is mainly caused due to consumption of puffer fish. No Known antidote for TTX exists. Treatment is symptomatic. The present review is therefore, an effort to give an idea about the distribution, origin, structure, pharmacol- ogy, toxicity, symptoms, treatment, resistance and application of TTX. Key words: Tetrodotoxin, Neurotoxin, Puffer fish. INTRODUCTION One of the most intriguing biotoxins isolated and described in the twentieth cantly more toxic than TTX. Palytoxin and maitotoxin have potencies nearly century is the neurotoxin, Tetrodotoxin (TTX, CAS Number [4368-28-9]). 100 times that of TTX and Saxitoxin, and all four toxins are unusual in being A neurotoxin is a toxin that acts specifically on neurons usually by interact- non-proteins. Interestingly, there is also some evidence for a bacterial bio- ing with membrane proteins and ion channels mostly resulting in paralysis. -

Zetekitoxin AB
Zetekitoxin AB Kate Wilkin Laura Graham Background of Zetekitoxin AB Potent water-soluble guanidinium toxin extracted from the skin of the Panamanian golden frog, Atelopus zeteki. Identified by Harry S. Mosher and colleagues at Stanford University, 1969. Originally named 1,2- atelopidtoxin. Progression 1975 – found chiriquitoxin in a Costa Rican Atelopus frog. 1977 – Mosher isolated 2 components of 1,2-atelopidtoxin. AB major component, more toxic C minor component, less toxic 1986 – purified from skin extracts by Daly and Kim. 1990 – the major component was renamed after the frog species zeteki. Classification Structural Identification Structural Identification - IR -1 Cm Functional Groups 1268 OSO3H 1700 Carbamate 1051 – 1022 C – N Structural Identification – MS Structural Identification – 13C Carbon Number Ppm Assignment 2 ~ 159 C = NH 4 ~ 85 Quaternary Carbon 5 ~ 59 Tertiary Carbon 6 ~ 54 Tertiary Carbon 8 ~ 158 C = NH Structural Identification – 13C Carbon Number Ppm Assignment 10 55 / 43 C H2 - more subst. on ZTX 11 89 / 33 Ring and OSO3H on ZTX 12 ~ 98 Carbon attached to 2 OH groups 19 / 13 70 / 64 ZTX: C – N STX: C – C 20 / 14 ~ 157 Carbamate Structural Identification – 13C Carbon Number Ppm Assignment 13 156 Amide 14 34 CH2 15 54 C – N 16 47 Tertiary Carbon 17 69 C – O – N 18 62 C – OH Structural Identification - 1H Synthesis Synthesis O. Iwamoto and Dr. K. Nagasawa Tokyo University of Agriculture and Technology. October 10th, 2007 “Further work to synthesize natural STXs and various derivatives is in progress with the aim of developing isoform-selective sodium-channel inhibitors” Therapeutic Applications Possible anesthetic, but has poor therapeutic index. -
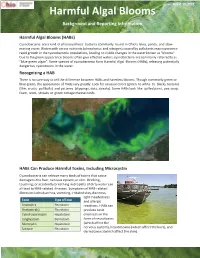
Harmful Algal Blooms Background and Reporting Information
Rev 8-12-2019 Harmful Algal Blooms Background and Reporting Information Harmful Algal Blooms (HABs) Cyanobacteria are a kind of photosynthetic bacteria commonly found in Ohio’s lakes, ponds, and slow- moving rivers. Waters with excess nutrients (phosphorus and nitrogen) caused by pollutants may experience rapid growth in the cyanobacteria populations, leading to visible changes in the water known as “blooms”. Due to the green appearance blooms often give effected waters, cyanobacteria are commonly referred to as “blue-green algae”. Some species of cyanobacteria form Harmful Algal Blooms (HABs), releasing potentially dangerous cyanotoxins in the water. Recognizing a HAB There is no sure way to tell the difference between HABs and harmless blooms. Though commonly green or blue-green, the appearance of HABs vary greatly. Look for unusual colors (green to white to black), textures (film, crusts, puffballs) and patterns (clippings, dots, streaks). Some HABs look like spilled paint, pea soup, foam, wool, streaks or green cottage cheese curds. HABs Can Produce Harmful Toxins, Including Microcystin Cyanobacteria can release many kinds of toxins that cause damage to the liver, nervous system, or skin. Drinking, touching, or accidently breathing in droplets of dirty water can all lead to HAB-related illnesses. Symptoms of HAB-related illness includes diarrhea, vomiting, irritated skin, dizziness, light-headedness Toxin Type of Toxin and allergic Anatoxin-a Neurotoxin reactions. HABs can Anatoxin-a(s) Neurotoxin produce toxic Cylindrospermopsin Hepatotoxin chemicals in the Lyngbyatoxin Dermatoxin form of neurotoxins Microcystin Hepatotoxin (which affect the Saxitoxin Neurotoxin nervous system), hepatotoxins (which affect the liver), and dermatoxins (which affect the skin). -

Toxicological and Pharmacological Profile of Amanita Muscaria (L.) Lam
Pharmacia 67(4): 317–323 DOI 10.3897/pharmacia.67.e56112 Review Article Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine Maria Voynova1, Aleksandar Shkondrov2, Magdalena Kondeva-Burdina1, Ilina Krasteva2 1 Laboratory of Drug metabolism and drug toxicity, Department “Pharmacology, Pharmacotherapy and Toxicology”, Faculty of Pharmacy, Medical University of Sofia, Bulgaria 2 Department of Pharmacognosy, Faculty of Pharmacy, Medical University of Sofia, Bulgaria Corresponding author: Magdalena Kondeva-Burdina ([email protected]) Received 2 July 2020 ♦ Accepted 19 August 2020 ♦ Published 26 November 2020 Citation: Voynova M, Shkondrov A, Kondeva-Burdina M, Krasteva I (2020) Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine. Pharmacia 67(4): 317–323. https://doi.org/10.3897/pharmacia.67. e56112 Abstract Amanita muscaria, commonly known as fly agaric, is a basidiomycete. Its main psychoactive constituents are ibotenic acid and mus- cimol, both involved in ‘pantherina-muscaria’ poisoning syndrome. The rising pharmacological and toxicological interest based on lots of contradictive opinions concerning the use of Amanita muscaria extracts’ neuroprotective role against some neurodegenerative diseases such as Parkinson’s and Alzheimer’s, its potent role in the treatment of cerebral ischaemia and other socially significant health conditions gave the basis for this review. Facts about Amanita muscaria’s morphology, chemical content, toxicological and pharmacological characteristics and usage from ancient times to present-day’s opportunities in modern medicine are presented. Keywords Amanita muscaria, muscimol, ibotenic acid Introduction rica, the genus had an ancestral origin in the Siberian-Be- ringian region in the Tertiary period (Geml et al. -

Amanita Muscaria: Ecology, Chemistry, Myths
Entry Amanita muscaria: Ecology, Chemistry, Myths Quentin Carboué * and Michel Lopez URD Agro-Biotechnologies Industrielles (ABI), CEBB, AgroParisTech, 51110 Pomacle, France; [email protected] * Correspondence: [email protected] Definition: Amanita muscaria is the most emblematic mushroom in the popular representation. It is an ectomycorrhizal fungus endemic to the cold ecosystems of the northern hemisphere. The basidiocarp contains isoxazoles compounds that have specific actions on the central nervous system, including hallucinations. For this reason, it is considered an important entheogenic mushroom in different cultures whose remnants are still visible in some modern-day European traditions. In Siberian civilizations, it has been consumed for religious and recreational purposes for millennia, as it was the only inebriant in this region. Keywords: Amanita muscaria; ibotenic acid; muscimol; muscarine; ethnomycology 1. Introduction Thanks to its peculiar red cap with white spots, Amanita muscaria (L.) Lam. is the most iconic mushroom in modern-day popular culture. In many languages, its vernacular names are fly agaric and fly amanita. Indeed, steeped in a bowl of milk, it was used to Citation: Carboué, Q.; Lopez, M. catch flies in houses for centuries in Europe due to its ability to attract and intoxicate flies. Amanita muscaria: Ecology, Chemistry, Although considered poisonous when ingested fresh, this mushroom has been consumed Myths. Encyclopedia 2021, 1, 905–914. as edible in many different places, such as Italy and Mexico [1]. Many traditional recipes https://doi.org/10.3390/ involving boiling the mushroom—the water containing most of the water-soluble toxic encyclopedia1030069 compounds is then discarded—are available. In Japan, the mushroom is dried, soaked in brine for 12 weeks, and rinsed in successive washings before being eaten [2]. -

Swaminathan (Article)
© 2000 Nature America Inc. • http://structbio.nature.com articles Structural analysis of the catalytic and binding sites of Clostridium botulinum neurotoxin B Subramanyam Swaminathan and Subramaniam Eswaramoorthy Clostridium botulinum neurotoxins are among the most potent toxins to humans. The crystal structures of intact C. botulinum neurotoxin type B (BoNT/B) and its complex with sialyllactose, determined at 1.8 and 2.6 Å resolution, respectively, provide insight into its catalytic and binding sites. The position of the belt region in BoNT/B is different from that in BoNT/A; this observation presents interesting possibilities for designing specific inhibitors that could be used to block the activity of this neurotoxin. The structures of BoNT/B and its complex with sialyllactose provide a detailed description of the active site and a model for interactions between the toxin and its cell surface receptor. The latter may provide valuable information for recombinant vaccine development. Botulinum and tetanus neurotoxins are solely responsible for the neuroparalytic syndromes of botulism and tetanus. These toxins .com are among the most poisonous known, with LD50 values in humans in the range of 0.1–1 ng kg-1 (ref. 1). Clostridium botu- linum cells produce seven serotypes of botulinum neurotoxin (BoNT, EC 3.4.24.69), called A–G, while tetanus neurotoxin (TeNT, EC 3.4.24.68) is produced by Clostridium tetani. These toxins are all produced as single inactive polypetide chains of ∼150 kDa that are cleaved by tissue proteinases into two chains: a heavy (H) chain of ∼100 kDa and a light (L) chain of ∼50 kDa http://structbio.nature • linked by a single disulfide bond. -

A Review of Chemical Defense in Poison Frogs (Dendrobatidae): Ecology, Pharmacokinetics, and Autoresistance
Chapter 21 A Review of Chemical Defense in Poison Frogs (Dendrobatidae): Ecology, Pharmacokinetics, and Autoresistance Juan C. Santos , Rebecca D. Tarvin , and Lauren A. O’Connell 21.1 Introduction Chemical defense has evolved multiple times in nearly every major group of life, from snakes and insects to bacteria and plants (Mebs 2002 ). However, among land vertebrates, chemical defenses are restricted to a few monophyletic groups (i.e., clades). Most of these are amphibians and snakes, but a few rare origins (e.g., Pitohui birds) have stimulated research on acquired chemical defenses (Dumbacher et al. 1992 ). Selective pressures that lead to defense are usually associated with an organ- ism’s limited ability to escape predation or conspicuous behaviors and phenotypes that increase detectability by predators (e.g., diurnality or mating calls) (Speed and Ruxton 2005 ). Defended organisms frequently evolve warning signals to advertise their defense, a phenomenon known as aposematism (Mappes et al. 2005 ). Warning signals such as conspicuous coloration unambiguously inform predators that there will be a substantial cost if they proceed with attack or consumption of the defended prey (Mappes et al. 2005 ). However, aposematism is likely more complex than the simple pairing of signal and defense, encompassing a series of traits (i.e., the apose- matic syndrome) that alter morphology, physiology, and behavior (Mappes and J. C. Santos (*) Department of Zoology, Biodiversity Research Centre , University of British Columbia , #4200-6270 University Blvd , Vancouver , BC , Canada , V6T 1Z4 e-mail: [email protected] R. D. Tarvin University of Texas at Austin , 2415 Speedway Stop C0990 , Austin , TX 78712 , USA e-mail: [email protected] L. -

Interaction of Batrachotoxin with the Local Anesthetic Receptor Site in Transmembrane Segment IVS6 of the Voltage-Gated Sodium Channel
Proc. Natl. Acad. Sci. USA Vol. 95, pp. 13947–13952, November 1998 Pharmacology Interaction of batrachotoxin with the local anesthetic receptor site in transmembrane segment IVS6 of the voltage-gated sodium channel NANCY J. LINFORD,ANGELA R. CANTRELL,YUSHENG QU,TODD SCHEUER, AND WILLIAM A. CATTERALL* Department of Pharmacology, Box 357280, University of Washington, Seattle, WA 98195-7280 Contributed by William A. Catterall, September 28, 1998 ABSTRACT The voltage-gated sodium channel is the site these sodium channel binding sites are distinct, allosteric of action of more than six classes of neurotoxins and drugs interactions among the sites modulate drug and toxin binding that alter its function by interaction with distinct, allosteri- (10–15). Neurotoxin receptor site 2 binds neurotoxins that cally coupled receptor sites. Batrachotoxin (BTX) is a steroi- cause persistent activation of sodium channels, including ba- dal alkaloid that binds to neurotoxin receptor site 2 and trachotoxin (BTX), veratridine, aconitine, and grayanotoxin causes persistent activation. BTX binding is inhibited allos- (10, 12, 16). BTX is a steroidal alkaloid from the skin secre- terically by local anesthetics. We have investigated the inter- tions of South American frogs of the genus Phyllobates (16). action of BTX with amino acid residues I1760, F1764, and Binding of BTX shifts the voltage dependence of sodium Y1771, which form part of local anesthetic receptor site in channel activation in the negative direction, blocks inactiva- transmembrane segment IVS6 of type IIA sodium channels. tion, and alters ion selectivity (17–20). Its binding to site 2 is Alanine substitution for F1764 (mutant F1764A) reduces a nearly irreversible and is highly dependent on the state of the tritiated BTX-A-20- -benzoate binding affinity, causing a channel with a strong preference for open sodium channels. -

Botulism Importance Botulism Is Caused by Botulinum Toxins, Neurotoxins Produced by Clostridium Botulinum and a Few Other Clostridial Species
Botulism Importance Botulism is caused by botulinum toxins, neurotoxins produced by Clostridium botulinum and a few other clostridial species. By binding to nerve endings, these Shaker Foal Syndrome, toxins cause progressive flaccid paralysis in humans and animals. Many untreated Limberneck, cases end in death from paralysis of the respiratory muscles. C. botulinum spores are Western Duck Sickness, common in the environment, but they can germinate and grow only under certain Bulbar Paralysis, anaerobic conditions. Foodborne botulism results from the ingestion of preformed Loin Disease, toxins after the organism has grown in food or other organic matter. Foodborne Lamziekte outbreaks may be extensive in some animals, especially farmed mink or foxes and wild waterfowl. Losses that may threaten survival of the species have been reported in endangered wild birds. Sporadic cases of botulism also occur when botulinum- producing organisms grow inside the body, particularly in the immature Last Updated: January 2018 gastrointestinal tracts of human infants and foals, or in anaerobic wounds. Botulism can be treated successfully, but human or animal patients may require weeks or months of intensive care, sometimes including mechanical ventilation, while the nerve endings regenerate. Treatment may be impractical in adult livestock unless the case is mild. The potential for botulinum toxins to be used in bioterrorism is an additional concern. Etiology Botulism is caused by botulinum toxin, a potent neurotoxin produced by Clostridium botulinum, a few strains of C. baratii and C. butyricum, and C. argentinense. All of these organisms are anaerobic, Gram-positive, spore-forming rods. C. botulinum is currently divided into three genotypically and phenotypically distinct groups, I through III. -

Neurotoxin Pre & Post Care Patient Instructions
NEUROTOXIN PRE & POST CARE PATIENT INSTRUCTIONS What Is A Neurotoxin? Neurotoxins are used for the temporary relief of wrinkles (rhytids), most typically of the forehead, brow, and "crow’s feet" region. There are 4 commonly utilized neurotoxins in the United States: Botox, Dysport, Jeaveau, and Xeomin. Our practice offers the first 3. All these products are very similar in nature and effect with subtle differences between them. A small percentage of people will be resistant to one or more of these toxins. Therefore, when treated, if the utilized agent is either ineffective or less than fully effective, you may respond better to one of the others. The toxin itself is a medically manufactured drug which has its initial origin from bacteria that produces a toxin and is associated with botulism. While that sounds scary, these toxins have been utilized in medicine for decades and have many different uses in addition to the above including treatment of migraine headaches and muscle spasticity. Their safety and efficacy have been proven extensively. The effects of these toxins last for 2 to 4 months. The toxin itself blocks the transmission of information from a local nerve to the associated muscle, and, therefore, with the muscle unable to fully flex, there are fewer lines associated with the commonly treated areas. There are other areas of the facial region that are treated with Botox, such as the upper lip or even the neck. These treatments are what are considered FDA off-label, and your provider will explain in more detail what that means. In general, it is that the drug is safe and effective for that use, but it has not been specifically queried to and approved by the FDA for that use. -

Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology
1521-0081/69/2/200–235$25.00 https://doi.org/10.1124/pr.116.012658 PHARMACOLOGICAL REVIEWS Pharmacol Rev 69:200–235, April 2017 Copyright © 2017 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: JEFFREY M. WITKIN Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology Marco Pirazzini, Ornella Rossetto, Roberto Eleopra, and Cesare Montecucco Department of Biomedical Sciences, University of Padova, Italy (M.P., O.R., C.M.); Neurologic Department, University-Hospital S. Maria della Misericordia, Udine, Italy (R.E.); and Consiglio Nazionale delle Ricerche, Institute of Neuroscience, University of Padova, Italy (C.M.) Abstract. ....................................................................................201 I. Introduction. ..............................................................................201 A. Genetics and Structure of Botulinum Neurotoxins and Their Progenitor Toxin Complexes. ..............................................................................202 B. Molecular Architecture of Botulinum Neurotoxins . .....................................203 C. Metalloproteolytic Activity . ............................................................204 II. Biology. ....................................................................................204 Downloaded from A. Molecular Mechanism of Nerve Terminal Paralysis . .....................................204 1. Binding and Specificity. ............................................................204 -

Download Product Insert (PDF)
PRODUCT INFORMATION Ibotenic Acid Item No. 14584 CAS Registry No.: 2552-55-8 Formal Name: α-amino-2,3-dihydro-3-oxo-5-isoxazoleacetic acid H H N O Synonym: NSC 204850 2 N MF: C5H6N2O4 FW: 158.1 O O Purity: ≥98% Supplied as: A solid OH Storage: -20°C Stability: ≥1 year Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Ibotenic acid is supplied as a solid. A stock solution may be made by dissolving the ibotenic acid in water. The solubility of ibotenic acid in water is approximately 10 mM. We do not recommend storing the aqueous solution for more than one day. Description Ibotenic acid is a neuroexcitatory amino acid originally isolated from Amanita species that functions as a NMDA and metabotropic glutamate receptor agonist.1 As a neurotoxin, ibotenic acid is often used to induce brain lesions in animals that model cognitive dysfunctions resulting from neurodegenerative diseases, traumatic brain injury, and stroke.2 References 1. Curtis, D.R., Lodge, D., and McLennan, H. The excitation and depression of spinal neurones by ibotenic acid. J. Physiol. 291, 19-28 (1979). 2. Tayebati, S.K. Animal models of cognitive dysfunction. Mech. Ageing Dev. 127(2), 100-108 (2005). WARNING CAYMAN CHEMICAL THIS PRODUCT IS FOR RESEARCH ONLY - NOT FOR HUMAN OR VETERINARY DIAGNOSTIC OR THERAPEUTIC USE. 1180 EAST ELLSWORTH RD SAFETY DATA ANN ARBOR, MI 48108 · USA This material should be considered hazardous until further information becomes available. Do not ingest, inhale, get in eyes, on skin, or on clothing.