Botulism Importance Botulism Is Caused by Botulinum Toxins, Neurotoxins Produced by Clostridium Botulinum and a Few Other Clostridial Species
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tetrodotoxin
Niharika Mandal et al. / Journal of Pharmacy Research 2012,5(7),3567-3570 Review Article Available online through ISSN: 0974-6943 http://jprsolutions.info Tetrodotoxin: An intriguing molecule Niharika Mandal*, Samanta Sekhar Khora, Kanagaraj Mohanapriya, and Soumya Jal School of Biosciences and Technology, VIT University, Vellore-632013 Tamil Nadu, India Received on:07-04-2012; Revised on: 12-05-2012; Accepted on:16-06-2012 ABSTRACT Tetrodotoxin (TTX) is one of the most potent neurotoxin of biological origin. It was first isolated from puffer fish and it has been discovered in various arrays of organism since then. Its origin is still unclear though some reports indicate towards microbial origin. TTX selectively blocks the sodium channel, inhibiting action potential thereby, leading to respiratory paralysis. TTX toxicity is mainly caused due to consumption of puffer fish. No Known antidote for TTX exists. Treatment is symptomatic. The present review is therefore, an effort to give an idea about the distribution, origin, structure, pharmacol- ogy, toxicity, symptoms, treatment, resistance and application of TTX. Key words: Tetrodotoxin, Neurotoxin, Puffer fish. INTRODUCTION One of the most intriguing biotoxins isolated and described in the twentieth cantly more toxic than TTX. Palytoxin and maitotoxin have potencies nearly century is the neurotoxin, Tetrodotoxin (TTX, CAS Number [4368-28-9]). 100 times that of TTX and Saxitoxin, and all four toxins are unusual in being A neurotoxin is a toxin that acts specifically on neurons usually by interact- non-proteins. Interestingly, there is also some evidence for a bacterial bio- ing with membrane proteins and ion channels mostly resulting in paralysis. -

Hawaii State Department of Health Tetanus Factsheet
TETANUS ABOUT THIS DISEASE Tetanus is an infection caused by a bacterium called Clostridium tetani. Spores of tetanus bacteria are everywhere in the environment, including soil, dust, and manure. These spores develop into bacteria when they enter the body through breaks in the skin, usually through injuries from contaminated objects. Clostridium tetani produce a toxin (poison) that causes painful muscle contractions. Tetanus is often called “lockjaw” because the first sign is most commonly spasms of the jaw muscles. Tetanus can lead to serious health problems, including being unable to open the mouth and having trouble swallowing and breathing, possibly leading to death (10% to 20% of cases). Tetanus is uncommon in the United States, with an average of 30 reported cases each year. Nearly all cases of tetanus in the U.S. are among people who have never received a tetanus vaccine, or adults who don’t stay up to date on their 10-year booster shots. SIGNS AND SYMPTOMS Symptoms of tetanus include: • Jaw cramping • Sudden, involuntary muscle tightening (muscle spasms) – often in the stomach • Painful muscle stiffness all over the body • Trouble swallowing • Jerking or staring (seizures) • Headache • Fever and sweating • Changes in blood pressure and a fast heart rate. Serious health problems that can happen because of tetanus include: • Laryngospasm (uncontrolled/involuntary tightening of the vocal cords) • Fractures (broken bones) • Hospital-acquired infections (Infections caught by a patient during a hospital stay) • Pulmonary embolism (blockage of the main artery of the lung or one of its branches by a blood clot that has travelled from elsewhere in the body through the bloodstream) • Aspiration pneumonia (lung infection that develops by breathing in foreign materials) • Breathing difficulty, possibly leading to death (1 to 2 in 10 cases are fatal) TRANSMISSION Tetanus is different from other vaccine-preventable diseases because it does not spread from person to person. -

Zetekitoxin AB
Zetekitoxin AB Kate Wilkin Laura Graham Background of Zetekitoxin AB Potent water-soluble guanidinium toxin extracted from the skin of the Panamanian golden frog, Atelopus zeteki. Identified by Harry S. Mosher and colleagues at Stanford University, 1969. Originally named 1,2- atelopidtoxin. Progression 1975 – found chiriquitoxin in a Costa Rican Atelopus frog. 1977 – Mosher isolated 2 components of 1,2-atelopidtoxin. AB major component, more toxic C minor component, less toxic 1986 – purified from skin extracts by Daly and Kim. 1990 – the major component was renamed after the frog species zeteki. Classification Structural Identification Structural Identification - IR -1 Cm Functional Groups 1268 OSO3H 1700 Carbamate 1051 – 1022 C – N Structural Identification – MS Structural Identification – 13C Carbon Number Ppm Assignment 2 ~ 159 C = NH 4 ~ 85 Quaternary Carbon 5 ~ 59 Tertiary Carbon 6 ~ 54 Tertiary Carbon 8 ~ 158 C = NH Structural Identification – 13C Carbon Number Ppm Assignment 10 55 / 43 C H2 - more subst. on ZTX 11 89 / 33 Ring and OSO3H on ZTX 12 ~ 98 Carbon attached to 2 OH groups 19 / 13 70 / 64 ZTX: C – N STX: C – C 20 / 14 ~ 157 Carbamate Structural Identification – 13C Carbon Number Ppm Assignment 13 156 Amide 14 34 CH2 15 54 C – N 16 47 Tertiary Carbon 17 69 C – O – N 18 62 C – OH Structural Identification - 1H Synthesis Synthesis O. Iwamoto and Dr. K. Nagasawa Tokyo University of Agriculture and Technology. October 10th, 2007 “Further work to synthesize natural STXs and various derivatives is in progress with the aim of developing isoform-selective sodium-channel inhibitors” Therapeutic Applications Possible anesthetic, but has poor therapeutic index. -

Safety and Immunogenicity of Capsular Polysaccharide–Tetanus Toxoid Conjugate Vaccines for Group B Streptococcal Types Ia and Ib
142 Safety and Immunogenicity of Capsular Polysaccharide±Tetanus Toxoid Conjugate Vaccines for Group B Streptococcal Types Ia and Ib Carol J. Baker, Lawrence C. Paoletti, Section of Infectious Diseases, Departments of Pediatrics and of Michael R. Wessels, Hilde-Kari Guttormsen, Microbiology and Immunology, Baylor College of Medicine, Houston, Marcia A. Rench, Melissa E. Hickman, Texas; Channing Laboratory, Department of Medicine, Brigham and Women's Hospital, and Department of Microbiology and Molecular and Dennis L. Kasper Genetics, Harvard Medical School, Boston, Massachusetts About 40% of invasive group B streptococcal (GBS) isolates are capsular polysaccharide Downloaded from https://academic.oup.com/jid/article/179/1/142/877598 by guest on 01 October 2021 (CPS) types Ia or Ib. Because infant and maternal GBS infections may be preventable by maternal vaccination, individual GBS CPS have been coupled to tetanus toxoid (TT) to prepare vaccines with enhanced immunogenicity. Immunogenicity in rabbits and protective capacity in mice of a series of type Ia- and Ib-TT conjugates increased with the degree of polysaccharide-to-protein cross-linking. In total, 190 healthy, nonpregnant women aged 18±40 years were randomized in four trials to receive Ia- or Ib-TT conjugate (dose range, 3.75±63 mg of CPS component), uncoupled Ia or Ib CPS, or saline. All vaccines were well-tolerated. CPS-speci®c IgG serum concentrations peaked 4±8 weeks after vaccination and were signif- icantly higher in recipients of conjugated than of uncoupled CPS. Immune responses to the conjugates were dose-dependent and correlated in vitro with opsonophagocytosis. These re- sults support inclusion of Ia- and Ib-TT conjugates when formulating a multivalent GBS vaccine. -

Shelf-Stable Food Safety
United States Department of Agriculture Food Safety and Inspection Service Food Safety Information PhotoDisc Shelf-Stable Food Safety ver since man was a hunter-gatherer, he has sought ways to preserve food safely. People living in cold climates Elearned to freeze food for future use, and after electricity was invented, freezers and refrigerators kept food safe. But except for drying, packing in sugar syrup, or salting, keeping perishable food safe without refrigeration is a truly modern invention. What does “shelf stable” Foods that can be safely stored at room temperature, or “on the shelf,” mean? are called “shelf stable.” These non-perishable products include jerky, country hams, canned and bottled foods, rice, pasta, flour, sugar, spices, oils, and foods processed in aseptic or retort packages and other products that do not require refrigeration until after opening. Not all canned goods are shelf stable. Some canned food, such as some canned ham and seafood, are not safe at room temperature. These will be labeled “Keep Refrigerated.” How are foods made In order to be shelf stable, perishable food must be treated by heat and/ shelf stable? or dried to destroy foodborne microorganisms that can cause illness or spoil food. Food can be packaged in sterile, airtight containers. All foods eventually spoil if not preserved. CANNED FOODS What is the history of Napoleon is considered “the father” of canning. He offered 12,000 French canning? francs to anyone who could find a way to prevent military food supplies from spoiling. Napoleon himself presented the prize in 1795 to chef Nicholas Appert, who invented the process of packing meat and poultry in glass bottles, corking them, and submerging them in boiling water. -
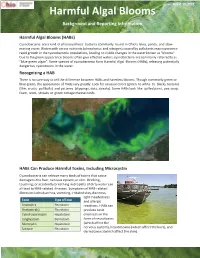
Harmful Algal Blooms Background and Reporting Information
Rev 8-12-2019 Harmful Algal Blooms Background and Reporting Information Harmful Algal Blooms (HABs) Cyanobacteria are a kind of photosynthetic bacteria commonly found in Ohio’s lakes, ponds, and slow- moving rivers. Waters with excess nutrients (phosphorus and nitrogen) caused by pollutants may experience rapid growth in the cyanobacteria populations, leading to visible changes in the water known as “blooms”. Due to the green appearance blooms often give effected waters, cyanobacteria are commonly referred to as “blue-green algae”. Some species of cyanobacteria form Harmful Algal Blooms (HABs), releasing potentially dangerous cyanotoxins in the water. Recognizing a HAB There is no sure way to tell the difference between HABs and harmless blooms. Though commonly green or blue-green, the appearance of HABs vary greatly. Look for unusual colors (green to white to black), textures (film, crusts, puffballs) and patterns (clippings, dots, streaks). Some HABs look like spilled paint, pea soup, foam, wool, streaks or green cottage cheese curds. HABs Can Produce Harmful Toxins, Including Microcystin Cyanobacteria can release many kinds of toxins that cause damage to the liver, nervous system, or skin. Drinking, touching, or accidently breathing in droplets of dirty water can all lead to HAB-related illnesses. Symptoms of HAB-related illness includes diarrhea, vomiting, irritated skin, dizziness, light-headedness Toxin Type of Toxin and allergic Anatoxin-a Neurotoxin reactions. HABs can Anatoxin-a(s) Neurotoxin produce toxic Cylindrospermopsin Hepatotoxin chemicals in the Lyngbyatoxin Dermatoxin form of neurotoxins Microcystin Hepatotoxin (which affect the Saxitoxin Neurotoxin nervous system), hepatotoxins (which affect the liver), and dermatoxins (which affect the skin). -

Broiler Chickens
The Life of: Broiler Chickens Chickens reared for meat are called broilers or broiler chickens. They originate from the jungle fowl of the Indian Subcontinent. The broiler industry has grown due to consumer demand for affordable poultry meat. Breeding for production traits and improved nutrition have been used to increase the weight of the breast muscle. Commercial broiler chickens are bred to be very fast growing in order to gain weight quickly. In their natural environment, chickens spend much of their time foraging for food. This means that they are highly motivated to perform species specific behaviours that are typical for chickens (natural behaviours), such as foraging, pecking, scratching and feather maintenance behaviours like preening and dust-bathing. Trees are used for perching at night to avoid predators. The life of chickens destined for meat production consists of two distinct phases. They are born in a hatchery and moved to a grow-out farm at 1 day-old. They remain here until they are heavy enough to be slaughtered. This document gives an overview of a typical broiler chicken’s life. The Hatchery The parent birds (breeder birds - see section at the end) used to produce meat chickens have their eggs removed and placed in an incubator. In the incubator, the eggs are kept under optimum atmosphere conditions and highly regulated temperatures. At 21 days, the chicks are ready to hatch, using their egg tooth to break out of their shell (in a natural situation, the mother would help with this). Chicks are precocial, meaning that immediately after hatching they are relatively mature and can walk around. -

The Home Flock
The Home Flock The development and management of a small flock of chickens for the production of eggs and meat is a favorite activity of many rural families. This publication addresses many topics that the beginning poultry owner will eventually confront. These topics include: • Start With Healthy Chicks • Preparing the Brooder House • Brooding Chicks • Management of Broiler Chicks • Feeding Schedules • Pullet Rearing • Vaccination Program • Lighting Programs • Layer Management • Roosters • Disease and Parasite Control • Care of Eggs Start With Healthy Chicks The "Home Flock" usually consists of 20 to 40 chickens kept to supply eggs and an occasional fat hen. An average family of five persons will require about 30 hens. To produce 30 pullets, start with 100 straight-run chicks or 50 sexed pullet chicks. Pullet chicks should be purchased if only layers are desired. Chicks can be started at any time during the year. Baby chicks started in March or April are normally the easiest to raise up to laying age (6 months). The problem with starting birds then is that they begin production in late summer or early fall. Birds started in March or April generally do not lay as many total eggs as do birds started in November and begin production in April. The disadvantage of starting birds in November is that they are harder to raise through the winter months to laying age in April. Usually the most desirable birds for a small flock are dual-purpose breeds such as Rhode Island Reds, Barred Rocks or Plymouth Rocks. However, if birds are to be kept for egg production only, it is best to choose birds bred only for that purpose (White Leghorn or Leghorn crosses). -

Skin and Soft Tissue Infections Ohsuerin Bonura, MD, MCR Oregon Health & Science University Objectives
Difficult Skin and Soft tissue Infections OHSUErin Bonura, MD, MCR Oregon Health & Science University Objectives • Compare and contrast the epidemiology and clinical presentation of common skin and soft tissue diseases • State the management for skin and soft tissue infections OHSU• Differentiate true infection from infectious disease mimics of the skin Casey Casey is a 2 year old boy who presents with this rash. What is the best treatment? A. Soap and Water B. Ibuprofen, it will self OHSUresolve C. Dicloxacillin D. Mupirocin OHSUImpetigo Impetigo Epidemiology and Treatment OHSU Ellen Ellen is a 54 year old morbidly obese woman with DM, HTN and venous stasis who presented with a painful left leg and fever. She has had 3 episodes in the last 6 months. What do you recommend? A. Cefazolin followed by oral amoxicillin prophylaxis B. Vancomycin – this is likely OHSUMRSA C. Amoxicillin – this is likely erysipelas D. Clindamycin to cover staph and strep cellulitis Impetigo OHSUErysipelas Erysipelas Risk: lymphedema, stasis, obesity, paresis, DM, ETOH OHSURecurrence rate: 30% in 3 yrs Treatment: Penicillin Impetigo Erysipelas OHSUCellulitis Cellulitis • DEEPER than erysipelas • Microbiology: – 6-48hrs post op: think GAS… too early for staph (days in the making)! – Periorbital – Staph, Strep pneumoniae, GAS OHSU– Post Varicella - GAS – Skin popping – Staph + almost anything! Framework for Skin and Soft Tissue Infections (SSTIs) NONPurulent Purulent Necrotizing/Cellulitis/Erysipelas Furuncle/Carbuncle/Abscess Severe Moderate Mild Severe Moderate Mild I&D I&D I&D I&D IV Rx Oral Rx C&S C&S C&S C&S Vanc + Pip-tazo OHSUEmpiric IV Empiric MRSA Oral MRSA TMP/SMX Doxy What Are Your “Go-To” Oral Options For Non-Purulent SSTI? Amoxicillin Doxycycline OHSUCephalexin Doxycycline Trimethoprim-Sulfamethoxazole OHSU Miller LG, et al. -

Botulism Fact Sheet
Botulism Fact Sheet 1. What is botulism? - Botulism is a rare but serious paralytic illness caused by a nerve toxin (poison) produced by the bacterium Clostridium botulinum. There are three main kinds of botulism. (a) Foodborne botulism is caused by eating foods that contain the botulism toxin. (b) Wound botulism is caused by toxin produced from a wound infected with Clostridium botulinum. (c) Infant botulism is caused when Clostridium botulinum bacteria grow in the immature infant intestines and release toxin. All forms of botulism can be fatal and are considered medical emergencies. Foodborne botulism can be especially dangerous because widespread illness can occur from eating a contaminated food. 2. What is Clostridium botulinum? - Clostridium botulinum belongs to is a group of bacteria commonly found in soil. They grow best in low oxygen conditions. The bacteria form spores which allow them to survive in a dormant state in the soil until exposed to conditions that can support their growth. In low oxygen conditions, the growing bacteria release botulinum toxin. There are seven types of botulism toxin designated by the letters A through G; only types A, B, E and F cause illness in humans. 3. How common is botulism? - In the United States an average of 45 cases are reported each year. Of these, approximately 15% are foodborne, 65% are infant botulism, and the rest are wound botulism. Outbreaks of foodborne botulism involving two or more persons occur most years and usually are caused by eating improperly processed home-canned foods. The number of Foodborne and Infant botulism cases has changed little in recent years, but wound botulism has increased because of the use of black-tar heroin. -

Toxicological and Pharmacological Profile of Amanita Muscaria (L.) Lam
Pharmacia 67(4): 317–323 DOI 10.3897/pharmacia.67.e56112 Review Article Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine Maria Voynova1, Aleksandar Shkondrov2, Magdalena Kondeva-Burdina1, Ilina Krasteva2 1 Laboratory of Drug metabolism and drug toxicity, Department “Pharmacology, Pharmacotherapy and Toxicology”, Faculty of Pharmacy, Medical University of Sofia, Bulgaria 2 Department of Pharmacognosy, Faculty of Pharmacy, Medical University of Sofia, Bulgaria Corresponding author: Magdalena Kondeva-Burdina ([email protected]) Received 2 July 2020 ♦ Accepted 19 August 2020 ♦ Published 26 November 2020 Citation: Voynova M, Shkondrov A, Kondeva-Burdina M, Krasteva I (2020) Toxicological and pharmacological profile of Amanita muscaria (L.) Lam. – a new rising opportunity for biomedicine. Pharmacia 67(4): 317–323. https://doi.org/10.3897/pharmacia.67. e56112 Abstract Amanita muscaria, commonly known as fly agaric, is a basidiomycete. Its main psychoactive constituents are ibotenic acid and mus- cimol, both involved in ‘pantherina-muscaria’ poisoning syndrome. The rising pharmacological and toxicological interest based on lots of contradictive opinions concerning the use of Amanita muscaria extracts’ neuroprotective role against some neurodegenerative diseases such as Parkinson’s and Alzheimer’s, its potent role in the treatment of cerebral ischaemia and other socially significant health conditions gave the basis for this review. Facts about Amanita muscaria’s morphology, chemical content, toxicological and pharmacological characteristics and usage from ancient times to present-day’s opportunities in modern medicine are presented. Keywords Amanita muscaria, muscimol, ibotenic acid Introduction rica, the genus had an ancestral origin in the Siberian-Be- ringian region in the Tertiary period (Geml et al. -

TETANUS in ANIMALS — SUMMARY of KNOWLEDGE Malinovská, Z
DOI: 10.2478/fv-2020-0027 FOLIA VETERINARIA, 64, 3: 54—60, 2020 TETANUS IN ANIMALS — SUMMARY OF KNOWLEDGE Malinovská, Z., Čonková, E., Váczi, P. Department of Pharmacology and Toxicology University of Veterinary Medicine and Pharmacy in Košice, Komenského 73, 041 81 Košice Slovakia [email protected] ABSTRACT the effects of the neurotoxin. The treatment is difficult with an unclear prognosis. Tetanus is a neurologic non-transmissible disease (often fatal) of humans and other animals with a world- Key words: animal; Clostridium tetani; toxin; spasm; wide occurrence. Clostridium tetani is the spore produc- treatment ing bacillus which causes the bacterial disease. In deep penetrating wounds the spores germinate and produce a toxin called tetanospasmin. The main characteristic sign INTRODUCTION of tetanus is a spastic paralysis. A diagnosis is usually based on the clinical signs because the detection in the Of the clostridial neurotoxins, botulinum neurotoxin wound and the cultivation of C. tetani is very difficult. and tetanus neurotoxin are the most potent toxins [15]. Between animal species there is considerable variabili- Their extraordinary toxicity is caused by neurospecificity ty in the susceptibility to the bacillus. The most sensi- and metalloprotease activity, which results in the paralysis. tive animal species to the neurotoxin are horses. Sheep Tetanus is potentially a fatal disease and in some countries and cattle are less sensitive and tetanus in these animal it is still very active. Tetanus is a traumatic clostridiosis, species are less common. Tetanus in cats and dogs are an infection in humans and other animals with worldwide rare and dogs are less sensitive than cats.