Atopic Dermatitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Champion Star Roeontly Imported from Knplund with U Una-Lan- but Ol at the Westminster Show Considerable Difficulty in Deciding on the POMKRANIAN
DOG BREEDER TAKES NOW TOPIC OF CONTROVERSY "ON TO PHILADELPHIA." Nassau Country Clnb Mkely to et KENNEL DIRECTORY SLOGAN OF DOG WORLD May 23 lor Open Air Show. ISSUE ON SEALYHAM Preparations for tht summer shows, delayed the more which have been for MlSCllMANEOCS. urgent business of getting ready and tak- rOMEKANIAXa. Many Winners at Westminster ing part In the premier fixture Just closed, English Judge Says the Breed will ba under way within the next week Show to 11 Benched With or so. One thine which kept tho Nassau Should Have Crooked Legi Country selecting a date for POMERANIANS Good Fresh Lot. Club from 'snnnnssnnnnn' to Go to Earth. Its open sir fixture was tho failure of the Jockey Cub to announce tho sched- SALE bbbbbbbbbbbbbbbbbbbbbbH sssssssssB FOR fsssssT slssVl si Aaat t I ule for tho racing season. Tho Nassau "On to Philadelphia" Is the cry In the club Is eo well satisfied with Belmont ALL BLUE RIBBONS but one at THIS THEORY DISPUTED doi; wot Id, for tho cjuulter City is fol- Park ns u enu-- ) for the show that no low line In the wak? of New York, on other place was cutislderod and the dato WESTMINSTER jBBBBBBBBBBBBBBBtiaWaSBUi' SBBBBBBBBBBBBBBBBBBBBI question to be BBBBBBBBBWr Vfcf. tuinual show will open was tho only Important ? Tui'MlaV tin third settled. KENNEL CLUB SHOW. with the promise of lielna; tli best held show on Man Who Knows Breed Well In- bHHIB' bbbbbbbbbbssbbbbbbbbbbbbbbbK-?" It now Is proposed to hold tho In the City of llnitheily Love. The May 23, which will be tho Saturday be- tHHHHIIIIIIIIIIIIIIIIIIIH nus-ilc- Go allaH h.)w, which will bo held under the a races, which begin All .Colors at Stud and for 'Sale. -

Friday, June 21, 2013
COMBINED PREMIUM LIST GREAT WESTERN TERRIER ASSOCIATION Obedience and Rally Trial AND TWELVE TERRIER SPECIALTIES ON THE GREAT WESTERN TERRIER ASSOCIATION OF SOUTHERN CALIFORNIA Presented by: Border Terrier Club of Southern California Parson Russell Terrier Association of America Golden State Bull Terrier Club Scottish Terrier Club of California Cairn Terrier Club of Southern California Sealyham Terrier Club of Southern California Irish Terrier Club of Southern California Soft Coated Wheaten Terrier Club of Southern California Miniature Bull Terrier Club of America(2 Specialties) Staffordshire Bull Terrier Club of America Miniature Schnauzer Club of Southern California THE QUEEN MARY EVENTS PARK 1126 Queens Highway Long Beach, California 90802 Friday, June 21, 2013 ENTRIES CLOSE WEDNESDAY, JUNE 5, 2013 NOON PDT The American Kennel Club Rules and Regulations will govern this event Unbenched/Outdoors Event Hours 7:00 AM to 8:00 PM BENCH SHOW COMMITTEE Karla Baer Cohen, Dennis Broderick, Frances Sikorski, Jack Smith, Robert Widden VETERINARIAN ON CALL Long Beach Animal Hospital 3816 E. Anaheim St., Long Beach, CA 90804 (562)434-9966 Exhibitors should follow their veterinarians’ recommendation to assure their dogs are free of internal and external parasites, any communicable diseases, and have appropriate vaccinations. Directions From Queen Mary: Take Queens Hwy. out of the park and drive North on the Long Beach Freeway (710 Freeway) to the Anaheim St. Exit. Turn right on W. Anaheim St. 3.4 miles. The hospital is on the corner of Anaheim & Miramar on the right. OFFICIAL PHOTOGRAPHERS Rich Bergman [email protected], Kitten Rodwell [email protected] CERTIFICATION Permission has been granted by the American Kennel Club for the holding of this event under American Kennel Club rules and regulations. -

DOG BREEDS Affenpinscher Afghan Hound Airedale Terrier Akita
DOG BREEDS English Foxhound Polish Lowland English Setter Sheepdog Affenpinscher English Springer Pomeranian Afghan Hound Spaniel Poodle Airedale Terrier English Toy Spaniel Portuguese Water Dog Akita Field Spaniel Pug Alaskan Malamute Finnish Spitz Puli American Eskimo Dog Flat-Coated Retriever Rhodesian Ridgeback American Foxhound French Bulldog Rottweiler American Staffordshire German Pinscher Saint Bernard Terrier German Shepherd Dog Saluki American Water German Shorthaired Samoyed Spaniel Pointer Schipperke Anatolian Shepherd German Wirehaired Scottish Deerhound Dog Pointer Scottish Terrier Australian Cattle Dog Giant Schnauzer Sealyham Terrier Australian Shepherd Glen of Imaal Terrier Shetland Sheepdog Australian Terrier Golden Retriever Shiba Inu Basenji Gordon Setter Shih Tzu Basset Hound Great Dane Siberian Husky Beagle Great Pyrenees Silky Terrier Bearded Collie Greater Swiss Mountain Skye Terrier Beauceron Dog Smooth Fox Terrier Bedlington Terrier Greyhound Soft Coated Wheaten Belgian Malinois Harrier Terrier Belgian Sheepdog Havanese Spinone Italiano Belgian Tervuren Ibizan Hound Staffordshire Bull Bernese Mountain Dog Irish Setter Terrier Bichon Frise Irish Terrier Standard Schnauzer Black and Tan Irish Water Spaniel Sussex Spaniel Coonhound Irish Wolfhound Swedish Vallhund Black Russian Terrier Italian Greyhound Tibetan Mastiff Bloodhound Japanese Chin Tibetan Spaniel Border Collie Keeshond Tibetan Terrier Border Terrier Kerry Blue Terrier Toy Fox Terrier Borzoi Komondor Vizsla Boston Terrier Kuvasz Weimaraner Bouvier des -
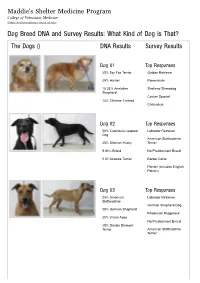
Dog Breed DNA and Survey Results: What Kind of Dog Is That? the Dogs () DNA Results Survey Results
Maddie's Shelter Medicine Program College of Veterinary Medicine (https://sheltermedicine.vetmed.ufl.edu) Dog Breed DNA and Survey Results: What Kind of Dog is That? The Dogs () DNA Results Survey Results Dog 01 Top Responses 25% Toy Fox Terrier Golden Retriever 25% Harrier Pomeranian 15.33% Anatolian Shetland Sheepdog Shepherd Cocker Spaniel 14% Chinese Crested Chihuahua Dog 02 Top Responses 50% Catahoula Leopard Labrador Retriever Dog American Staffordshire 25% Siberian Husky Terrier 9.94% Briard No Predominant Breed 5.07 Airedale Terrier Border Collie Pointer (includes English Pointer) Dog 03 Top Responses 25% American Labrador Retriever Staffordshire German Shepherd Dog 25% German Shepherd Rhodesian Ridgeback 25% Lhasa Apso No Predominant Breed 25% Dandie Dinmont Terrier American Staffordshire Terrier Dog 04 Top Responses 25% Border Collie Wheaten Terrier, Soft Coated 25% Tibetan Spaniel Bearded Collie 12.02% Catahoula Leopard Dog Briard 9.28% Shiba Inu Cairn Terrier Tibetan Terrier Dog 05 Top Responses 25% Miniature Pinscher Australian Cattle Dog 25% Great Pyrenees German Shorthaired Pointer 10.79% Afghan Hound Pointer (includes English 10.09% Nova Scotia Duck Pointer) Tolling Retriever Border Collie No Predominant Breed Dog 06 Top Responses 50% American Foxhound Beagle 50% Beagle Foxhound (including American, English, Treeing Walker Coonhound) Harrier Black and Tan Coonhound Pointer (includes English Pointer) Dog 07 Top Responses 25% Irish Water Spaniel Labrador Retriever 25% Siberian Husky American Staffordshire Terrier 25% Boston -

What's Your Dog's Tale?
Congratulations! You’re about to uncover the story of your dog’s ancestry. What’s In this report, you will find detailed results from Tulip’s Wisdom Panel® Professional DNA analysis. Your In the following pages, you will learn about: BREED DETECTION Dog’s APPEARANCE, BEHAVIOR & HISTORY BREED APPEARANCE Tale? SHARING YOUR DOG’S STORY It is important to carefully review your entire report and discuss the results with your veterinarian to gain the most valuable insight into Tulip. Owner Name: Jennifer Smith Test Report Code: 4000049604 Date Printed: June 23, 2014 TULIP Tulip Breed Detection You have a American Staffordshire Terrier, Parson Russell Terrier Mix! The Wisdom Panel® Professional computer algorithm performed over seven million calculations using 11 different models (from a single breed to complex combinations of breeds) to predict the most likely combination of pure and mixed breed dogs in the last 3 ancestral generations that best fit the DNA marker pattern observed in Tulip. The ancestry chart depicting the best statistical result of this analysis is shown in the picture below. American Staffs. American Staffs. American Staffs. American Staffs. Parson Russell Parson Russell Mixed Mixed Terrier Terrier Terrier Terrier Terrier Terrier Breed† Breed† American Staffs. American Staffs. Parson Russell Mixed Terrier Terrier Terrier Breed† Tulip American Staffs. Parson Russell Terrier Terrier Mix Tulip Appearance, Behavior & History American Staffordshire Terrier Height: 17 - 19 in Weight (Show): 40 - 60 lb Weight (Pet): Terrier 38 - 68 lb Ears: Muzzle: Tail: American Staffordshire The American Staffordshire Terrier can trace its roots all the way back to the nineteenth century in England. -

Quiz Sheets BDB JWB 0513.Indd
2. A-Z Dog Breeds Quiz Write one breed of dog for each letter of the alphabet and receive one point for each correct answer. There’s an extra five points on offer for those that can find correct answers for Q, U, X and Z! A N B O C P D Q E R F S G T H U I V J W K X L Y M Z Dogs for the Disabled The Frances Hay Centre, Blacklocks Hill, Banbury, Oxon, OX17 2BS Tel: 01295 252600 www.dogsforthedisabled.org supporting Registered Charity No. 1092960 (England & Wales) Registered in Scotland: SCO 39828 ANSWERS 2. A-Z Dog Breeds Quiz Write a breed of dog for each letter of the alphabet (one point each). Additional five points each if you get the correct answers for letters Q, U, X or Z. Or two points each for the best imaginative breed you come up with. A. Curly-coated Retriever I. P. Tibetan Spaniel Affenpinscher Cuvac Ibizan Hound Papillon Tibetan TerrieR Afghan Hound Irish Terrier Parson Russell Terrier Airedale Terrier D Irish Setter Pekingese U. Akita Inu Dachshund Irish Water Spaniel Pembroke Corgi No Breed Found Alaskan Husky Dalmatian Irish Wolfhound Peruvian Hairless Dog Alaskan Malamute Dandie Dinmont Terrier Italian Greyhound Pharaoh Hound V. Alsatian Danish Chicken Dog Italian Spinone Pointer Valley Bulldog American Bulldog Danish Mastiff Pomeranian Vanguard Bulldog American Cocker Deutsche Dogge J. Portugese Water Dog Victorian Bulldog Spaniel Dingo Jack Russel Terrier Poodle Villano de Las American Eskimo Dog Doberman Japanese Akita Pug Encartaciones American Pit Bull Terrier Dogo Argentino Japanese Chin Puli Vizsla Anatolian Shepherd Dogue de Bordeaux Jindo Pumi Volpino Italiano Dog Vucciriscu Appenzeller Moutain E. -

Great Western Terrier Association of Southern California, Inc
PREMIUM LIST __________________________________________________________________________________ Two Terrier Group Shows GREAT WESTERN TERRIER ASSOCIATION of Southern California, Inc. ____________________________________________________________________________________ SANTA FE DAM RECREATIONAL AREA 15501 East Arrow Highway Irwindale, CA 91706 Major Sponsor ~ Please see last page for 30% discounts on products Saturday, June 24, 2017 NOHS, 4-6 Mo Beginner Competition, Bred By Exhibitor Groups Offered Sunday, June 25, 2017 NOHS, Sweepstakes Group Offered ENTRIES CLOSE WEDNESDAY - JUNE 7, 2017 - AT NOON PDT This is a condensed premium list as authorized by the American Kennel Club, "Rules Applying to Registration and Dog Shows", Chapter 9, Section 2A. A complete list of trophies and prizes is available upon request to the Show Superintendent. Trophy donors will be named in the catalog. HIGHLIGHTING TERRIERS IN SOUTHERN CALIFORNIA GWTA - Saturday, June 24, 2017 Specialty Shows with Puppy Sweepstakes and/or Veteran Sweepstakes(*) Irish Terrier Club of Southern California* Skye Terrier Club of Southern California Miniature Schnauzer Club of So. California* Welsh Terrier Club of Southern California* Supported Entries - with Puppy and/or Veteran Sweepstakes(*) So. California Airedale Association Norwich Terrier Club of America Australian Terrier Club of America Parson Russell Terrier Association of America* Border Terrier Club of Southern California Southern California Rat Terrier Club Golden State Bull Terrier Club* Scottish Terrier Club of California* Cairn Terrier Club of So. California Sealyham Terrier Club of Southern California Kerry Blue Terrier Club of Southern California Soft Coated Wheaten Terrier Club of America Miniature Bull Terrier Club of America* Staffordshire Bull Terrier Club of America* West Highland White Terrier Club of California* GWTA - Sunday, June 25, 2017 Specialty Shows with Veteran Sweepstakes(*) So. -
Domestic Dog Breeding Has Been Practiced for Centuries Across the a History of Dog Breeding Entire Globe
ANCESTRY GREY WOLF TAYMYR WOLF OF THE DOMESTIC DOG: Domestic dog breeding has been practiced for centuries across the A history of dog breeding entire globe. Ancestor wolves, primarily the Grey Wolf and Taymyr Wolf, evolved, migrated, and bred into local breeds specific to areas from ancient wolves to of certain countries. Local breeds, differentiated by the process of evolution an migration with little human intervention, bred into basal present pedigrees breeds. Humans then began to focus these breeds into specified BREED Basal breed, no further breeding Relation by selective Relation by selective BREED Basal breed, additional breeding pedigrees, and over time, became the modern breeds you see Direct Relation breeding breeding through BREED Alive migration BREED Subsequent breed, no further breeding Additional Relation BREED Extinct Relation by Migration BREED Subsequent breed, additional breeding around the world today. This ancestral tree charts the structure from wolf to modern breeds showing overlapping connections between Asia Australia Africa Eurasia Europe North America Central/ South Source: www.pbs.org America evolution, wolf migration, and peoples’ migration. WOLVES & CANIDS ANCIENT BREEDS BASAL BREEDS MODERN BREEDS Predate history 3000-1000 BC 1-1900 AD 1901-PRESENT S G O D N A I L A R T S U A L KELPIE Source: sciencemag.org A C Many iterations of dingo-type dogs have been found in the aborigine cave paintings of Australia. However, many O of the uniquely Australian breeds were created by the L migration of European dogs by way of their owners. STUMPY TAIL CATTLE DOG Because of this, many Australian dogs are more closely related to European breeds than any original Australian breeds. -

Sealyham Terrier
GROUP IV TERRIERS IV-23 Sealyham Terrier Origin and Purpose The Sealyham Terrier was originally developed in the region of Haverfordwest in South Wales for the purpose of digging out badger and fox, and later was used in otter hunting also. His short legs were ideal for “going to earth”, and his rough coat protected him from attack by his prey. General Appearance A well let-down, strong, sturdily built, active working terrier of Welsh origin. The Sealyham should be the embodiment of power and determination, ever keen and alert, presenting a balanced picture of great substance in a small compass. The Sealyham should not be so heavily boned as to be coarse, or slight boned as to appear racy. General outline oblong, not square. Temperament A keen, reliable working terrier, making an ideal companion and pet. Size Height at withers about 10-1/2 inches (26 cm). Weight 23-25 lb. (10-11 kg) for dogs, bitches slightly less. Size is more important than weight. General conformation, overall balance, type and substance are the main criteria. Faults: Much oversized or undersized. Coat and Colour Coat weather-resisting, comprised of a soft dense undercoat and hard, straight, wiry topcoat. Colour: All white or with lemon, tan, badger, or blue badger markings on head and ears. Heavy body markings and excessive undercoat ticking are to be discouraged. Faults: Silky or curly coat. Heavy body markings. Head Long, broad, and powerful without coarseness. It should be in perfect balance with the body, joining the neck smoothly. Length of head roughly three-quarters height at withers. -
View the 2020 National Dog Show Program
The National Dog Show Hosted by A Thanksgiving Tradition NOVEMBER 14 & 15, 2020 Broadcast at Noon Thanksgiving Day November 26 WELCOME Welcome to the National Dog Show hosted by the Kennel Club of Philadelphia. On behalf of the members of the Kennel Club of Philadelphia, I thank you for joining us today as we once again celebrate showing purebred dogs in the Philadelphia area. The show was founded in 1879 and became an annual event in 1933. The Kennel Club of Philadelphia proudly supports a number of canine related organizations and has donated over $500,000 to these groups in the past 5 years. The National Dog Show, airing annually on Thanksgiving Day at noon on NBC, has been thrilling dog lovers ever since it began in 2002, and we estimate that since then, one quarter of a billion people have watched! Enjoy the dog show, and let us know about your experience at www.facebook.com/ kennelclubofphiladogshows/. Happy Thanksgiving! WATCH THE Wayne Ferguson, President Kennel Club of Philadelphia NATIONAL DOG SHOW THANKSGIVING DAY HOSTED BY AT NOON, NOVEMBER 26, ON NBC. 1 personnel will not have access to the premises of viewers over Thanksgiving weekend, delivering WHAT’S DIFFERENT THIS YEAR? the Greater Philadelphia Expo Center in Oaks, Pa. its third-best score in total viewers since the first Still, dog shows have been organized around the broadcast in 2002. The show is part of a five-hour country throughout the summer and many of the block of family programming on NBC, offering EXPECT ANOTHER GRAND CELEBRATION best dogs in America live with their owners and the country’s 65 million pet-owning households a OF THE CANINE, MAN’S BEST FRIEND handlers in the northeast and mid-Atlantic states. -

Capt. John Owen Tucker-Edwardes and the Sealyham Terrier Most Dogs Were Developed After Hundreds of Years of Evolution and Lengthy Selection by Breeders
Masterminds by Ria Hörter illustrations courtesy Ria Hörter Sealyham House Capt. John Owen Tucker-Edwardes and the Sealyham Terrier Most dogs were developed after hundreds of years of evolution and lengthy selection by breeders. However, some breeds owe their existence to just one person. t’s no coincidence that almost every dog family had been connected to Pembroke- Ibreed creator descended from a military shire for more than six centuries. or noble family. These families had the time, John Owen Tucker-Edwardes’ father money and opportunity to develop a breed was William Tucker-Edwardes, Esq. (1784- and work the dogs. John Owen Tucker-Ed- 1858) of Sealyham, High Sherrif of Pem- wardes (1808-91) was no exception. brokeshire and representative of the mon- It is said that the first Tucker travelled arch in that part of Wales. to England with William the Conqueror in John Owen’s mother, Anna Martha Phil- 1066. Around 1356, when Thomas Tucker lipps (1788-1878), was the second daughter was a captain in the army of King Edward of George Phillipps, Esq., of Cwmgwilli and III, the king gave him land in Sealyham, Istradwrallt, Member of Parliament. Wil- Pembrokeshire (Wales). Thomas and his liam and Anna Martha married in Novem- descendants became known as “the Tuck- ber 1807; their eldest son, John Owen, was ers of Sealyham.” born in 1808. Capt. John Owen Tucker-Edwardes John Owen and his brothers and sisters Family grew up at Sealyham (also “Sealy Ham”) The Edwardes family was one of the oldest and wealthiest in Estate, located between Haverfordwest and Fishguard, on the Wales. -

A B C D E F Pricing by Breed
PRICING BY BREED Please choose the closest breed to your pet. If your breed is not listed, please call us at 480.399.3789 for a price quote. A C Affenpinscher $75 Cats (All Breeds) $90 Afghan Hound $120 Canaan Dog $100 Airedale Terrier -Standard $120 Cairn Terrier $75 Airedale Terrier - Minature $85 Cavalier King Charles Spaniel $75 Akita $120 Chesapeake Bay Retriever $100 Alaskan Malamute $130 Chihuahua $65 American English Coonhound $75 Chinese Crested American Eskimo $90 • Hairless $70 American Foxhound $75 • Powder-Puff $70 American Staffordshire Terrier $75 Chinese Shar-Pei $85 American Water Spaniel $85 Chow Chow $110 Anatolian Shepard $90 Clumber Spaniel $85 Australian Cattle Dog $90 Cocker Spaniel $85 Australian Shepherd Coonhound $75 • Full Size $110 Collie $105 • Mini $90 Corgi $80 Australian Terrier $75 Coton De Tulaer $80 Curly-Coated Retriever $100 B Basenji $75 D Basset Hound $75 Dachshund/Dotson $65 Beagle $75 Dalmatian $75 Bearded Collie $120 Dandie Dinmont Terrier $75 Beauceron $85 Doberman Pinscher $75 Bedlington Terrier $80 Dogo Argentino $85 Belgian Malinois $120 Doodle Belgian Sheepdog $120 • Full Size (30+) $110 Belgian Tervuren $120 • Half Size (0-29lbs) $85 Bernese Mountain Dog $140 Bichon Frise $80 Bloodhound $80 E Blue Heeler $100 English Cocker Spaniel $85 Border Collie $110 English Foxhound $75 Border Terrier $75 English Setter $90 Borzoi $110 English Springer Spaniel $90 Boston Terrier $75 English Toy Spaniel $75 Bouvier des Flandres $120 Boxer $75 F Boykin Spaniel $100 Flat-Coated Retriever $110 Briard $100 Brittany $100 Brussels Griffon $80 Bull Dog • American $75 • English $75 • French $70 Bull Terrier $75 PRICING BY BREED Please choose the closest breed to your pet.