Determinants of Perinatal Mortality Among Cohorts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Districts of Ethiopia
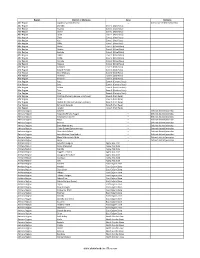
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

Next Stage for Dairy Development in Ethiopia
The NEXT STAGE IN DAIRY DEVELOPMENT FOR ETHIOPIA Dairy Value Chains, End Markets and Food Security Cooperative Agreement 663-A-00-05-00431-00 Submitted by Land O'Lakes, Inc. P.O. Box 3099 code 1250, Addis Ababa, Ethiopia November 2010 2 TABLE OF CONTENT Pages ACRONYMNS…………………………………………………………………………………. 5 EXECUTIVE SUMMARY …………………………………………………………………... 6 1. OVERVIEW OF THE DAIRY SUB-SECTOR STUDY………………………………….10 1.1. The Role of the Dairy Sub-Sector in the Economy of Ethiopia 1.1.1. Milk Production and its Allocation 1.1.2 Livestock and Milk in the household economy 1.2. The Challenges 1.3. A Value Chain Approach 1.4. The Tasks and the Study Team 2. DEMAND FOR MILK AND MILK PRODUCTS…………………………………….…. 15 2.1. Milk Consumption 2.1.1. Milk and Milk Product Consumption in Urban Areas 2.1.2. Milk and Milk Product Consumption in Rural Areas 2.1.3. Milk and Milk Product Consumption in Pastoral Areas 2.2. Milk Consumption Compared to Other Countries 2.3. Milk’s Role for Food Security and Household Nutrition 2.4. Consumption of Imported Milk Products by Areas and Product Categories – domestic and imported 2.5. Milk Consumption in 2020 2.5.1.. High Estimate 2.5.2. Middle of the Range Estimate 2.5.3. Low Estimate 2.6. Assessment 3. DAIRY PRODUCTION……………………………………………………………..…… 30 3.1. Current Situation 3.2. Milk Production Areas (waiting on the maps) 3.3. Production systems and Milk Sheds (see zonal data in annex 3.3.1. Commercial Production 3.3.2. Peri-Urban and Urban Production 3.3.3. -

11 HS 000 ETH 013013 A4.Pdf (English)
ETHIOPIA:Humanitarian Concern Areas Map (as of 04 February 2013) Eritrea > !ª !ª> Note: The following newly created woreda boundaries are not Tahtay !ª E available in the geo-database; hence not represented in this Nutrition Hotspot Priority Laelay Erob R R !ª Adiyabo Mereb Ahferom !ª Tahtay Gulomekeda !ª I E map regardless of their nutrition hot spot priority 1 & 2: Adiyabo Leke T D Adiyabo Adwa Saesie Dalul Priority one Asgede Tahtay R S Kafta Werei Tsaedaemba E E Priority 1: Dawa Sarar (Bale zone), Goro Dola (Guji zone), Abichu Tsimbila Maychew !ª A Humera Leke Hawzen Berahle A Niya( North Showa zone) and Burka Dintu (West Hararge Priority two > T I GR AY > Koneba Central Berahle zone) of Oromia region, Mekoy (Nuer zone) of Gambella Western Naeder Kola Ke>lete Awelallo Priority three Tselemti Adet Temben region, Kersadula and Raso (Afder zone), Ararso, Birkod, Tanqua > Enderta !ª Daror and Yo'ale (Degahabour zone), Kubi (Fik zone), Addi Tselemt Zone 2 No Priority given Arekay Abergele Southern Ab Ala Afdera Mersin (Korahe zone), Dhekasuftu and Mubarek (Liben Beyeda Saharti Erebti Debark Hintalo !ª zone), Hadigala (Shinille zone) and Daratole (Warder Abergele Samre > Megale Erebti Bidu Wejirat zone) of Somali region. Dabat Janamora > Bidu International Boundary Alaje Raya North Lay Sahla Azebo > Wegera Endamehoni > > Priority 2: Saba Boru (Guji zone) of Oromia region and Ber'ano Regional Boundary Gonder Armacho Ziquala > A FA R !ª East Sekota Raya Yalo Teru (Gode zone) and Tulu Guled (Jijiga zone) of Somali region. Ofla Kurri Belesa -

Prioritization of Shelter/NFI Needs
Prioritization of Shelter/NFI needs Date: 31st May 2018 Shelter and NFI Needs As of 18 May 2018, the overall number of displaced people is 345,000 households. This figure is based on DTM round 10, partner’s assessments, government requests, as well as the total of HH supported since July 2017. The S/NFI updated its prioritisation in early May and SNFI Cluster partners agreed on several criteria to guide prioritisation which include: - 1) type of emergency, 2) duration of displacement, and 3) sub-standard shelter conditions including IDPS hosted in collective centres and open-air sites and 4) % of vulnerable HH at IDP sites. Thresholds for the criteria were also agreed and in the subsequent analysis the cluster identified 193 IDP hosting woredas mostly in Oromia and Somali regions, as well as Tigray, Gambella and Addis Ababa municipality. A total of 261,830 HH are in need of urgent shelter and NFI assistance. At present the Cluster has a total of 57,000 kits in stocks and pipeline. The Cluster requires urgent funding to address the needs of 204,830 HHs that are living in desperate displacement conditions across the country. This caseload is predicted to increase as the flooding continues in the coming months. Shelter and NFI Priority Activities In terms of priority activities, the SNFI Cluster is in need of ES/NFI support for 140,259 HH displaced mainly due to flood and conflict under Pillar 2, primarily in Oromia and Somali Regions. In addition, the Shelter and NFI Cluster requires immediate funding for recovery activities to support 14,000 HH (8,000 rebuild and 6,000 repair) with transitional shelter support and shelter repair activities under Pillar 3. -

Oromia Region Administrative Map(As of 27 March 2013)
ETHIOPIA: Oromia Region Administrative Map (as of 27 March 2013) Amhara Gundo Meskel ! Amuru Dera Kelo ! Agemsa BENISHANGUL ! Jangir Ibantu ! ! Filikilik Hidabu GUMUZ Kiremu ! ! Wara AMHARA Haro ! Obera Jarte Gosha Dire ! ! Abote ! Tsiyon Jars!o ! Ejere Limu Ayana ! Kiremu Alibo ! Jardega Hose Tulu Miki Haro ! ! Kokofe Ababo Mana Mendi ! Gebre ! Gida ! Guracha ! ! Degem AFAR ! Gelila SomHbo oro Abay ! ! Sibu Kiltu Kewo Kere ! Biriti Degem DIRE DAWA Ayana ! ! Fiche Benguwa Chomen Dobi Abuna Ali ! K! ara ! Kuyu Debre Tsige ! Toba Guduru Dedu ! Doro ! ! Achane G/Be!ret Minare Debre ! Mendida Shambu Daleti ! Libanos Weberi Abe Chulute! Jemo ! Abichuna Kombolcha West Limu Hor!o ! Meta Yaya Gota Dongoro Kombolcha Ginde Kachisi Lefo ! Muke Turi Melka Chinaksen ! Gne'a ! N!ejo Fincha!-a Kembolcha R!obi ! Adda Gulele Rafu Jarso ! ! ! Wuchale ! Nopa ! Beret Mekoda Muger ! ! Wellega Nejo ! Goro Kulubi ! ! Funyan Debeka Boji Shikute Berga Jida ! Kombolcha Kober Guto Guduru ! !Duber Water Kersa Haro Jarso ! ! Debra ! ! Bira Gudetu ! Bila Seyo Chobi Kembibit Gutu Che!lenko ! ! Welenkombi Gorfo ! ! Begi Jarso Dirmeji Gida Bila Jimma ! Ketket Mulo ! Kersa Maya Bila Gola ! ! ! Sheno ! Kobo Alem Kondole ! ! Bicho ! Deder Gursum Muklemi Hena Sibu ! Chancho Wenoda ! Mieso Doba Kurfa Maya Beg!i Deboko ! Rare Mida ! Goja Shino Inchini Sululta Aleltu Babile Jimma Mulo ! Meta Guliso Golo Sire Hunde! Deder Chele ! Tobi Lalo ! Mekenejo Bitile ! Kegn Aleltu ! Tulo ! Harawacha ! ! ! ! Rob G! obu Genete ! Ifata Jeldu Lafto Girawa ! Gawo Inango ! Sendafa Mieso Hirna -

14 3W Food123017 A4.Pdf (English)
Ethiopia: 3W - Food Cluster Ongoing and Planned Activities map (as of December 2017) ERITREA Tahtay Adiyabo REST Total Number of Partners Laelay DPPB 8 DPPB Erob Dalul REST REST Adiyabo Gulomekeda DPPB Medebay REST DPPB Zana DPPB Red Sea Asgede DPPB DPPB Werei DPPB Hawzen Tsimbila DPPB Leke Koneba REST REST DPPB DPPB TIGRAY DPPB DPPB DPPB REST REST Berahile Kola DPPB DPPB REST Kelete SUDAN Temben Tselemti Awelallo DPPB DPPB Afdera DPPB DPPB Tselemt Ab Ala DPPB DPPB REST REST DPPB Erebti DPPB Abergele Hintalo Saharti DPPB DPPB Bidu Wejirat DPPB DPPB SCI SCI Samre Gulf of DPPB DPPB DPPB Dabat Megale Aden Janamora Alaje Wegera Sahla SCI Raya FHE DPPB DPPB Azebo DPPB Teru Gonder East Ziquala Ofla REST Kurri Zuria DPPB Belesa Sekota DPPB DPPB DPPB Dehana Yalo DPPB DPPB FHE DPPB AMHARA FHE Alamata DPPB Ebenat Gaz Gulina FHE Kobo DPPB Gibla DPPB Elidar DPPB Bugna SCI FHE DPPB Awra AFAR SCI Lasta Gidan DPPB Lay Guba Meket Lafto Gayint SCI Ewa DPPB FHE DPPB FHE Tach Ambasel SCI Aysaita Gayint Wadla DPPB Habru Dubti DPPB FHE Chifra Mile DPPB Delanta DPPB DPPB DPPB DPPB DPPB DPPB FHE Mekdela DPPB Adaa'r DPPB DPPB DPPB Simada DPPB Kutaber DPPB Afambo DJIBOUTI Sayint Bati Tenta DPPB DPPB Telalak DPPB DPPB DPPB DPPB Were Ilu Enarj Argoba DPPB DPPB DPPB Enawga Legehida DPPB Gewane Ayisha DPPB Albuko Dewe DPPB Debresina DPPB DPPB DPPB DPPB Wegde DPPB Artuma DPPB BENISHANGUL DPPB DPPB Debay DPPB Fursi DPPB Kelela DPPB GUMUZ Telatgen DPPB DPPB Jama DPPB DPPB Amuru Dera DPPB DPPB Afdem Erer SOMALI DPPB Menz Mama Jille Hadelela Shinile DPPB DPPB Dembel DPPB -

Administrative Region, Zone and Woreda Map of Oromia a M Tigray a Afar M H U Amhara a Uz N M
35°0'0"E 40°0'0"E Administrative Region, Zone and Woreda Map of Oromia A m Tigray A Afar m h u Amhara a uz N m Dera u N u u G " / m r B u l t Dire Dawa " r a e 0 g G n Hareri 0 ' r u u Addis Ababa ' n i H a 0 Gambela m s Somali 0 ° b a K Oromia Ü a I ° o A Hidabu 0 u Wara o r a n SNNPR 0 h a b s o a 1 u r Abote r z 1 d Jarte a Jarso a b s a b i m J i i L i b K Jardega e r L S u G i g n o G A a e m e r b r a u / K e t m uyu D b e n i u l u o Abay B M G i Ginde e a r n L e o e D l o Chomen e M K Beret a a Abe r s Chinaksen B H e t h Yaya Abichuna Gne'a r a c Nejo Dongoro t u Kombolcha a o Gulele R W Gudetu Kondole b Jimma Genete ru J u Adda a a Boji Dirmeji a d o Jida Goro Gutu i Jarso t Gu J o Kembibit b a g B d e Berga l Kersa Bila Seyo e i l t S d D e a i l u u r b Gursum G i e M Haro Maya B b u B o Boji Chekorsa a l d Lalo Asabi g Jimma Rare Mida M Aleltu a D G e e i o u e u Kurfa Chele t r i r Mieso m s Kegn r Gobu Seyo Ifata A f o F a S Ayira Guliso e Tulo b u S e G j a e i S n Gawo Kebe h i a r a Bako F o d G a l e i r y E l i Ambo i Chiro Zuria r Wayu e e e i l d Gaji Tibe d lm a a s Diga e Toke n Jimma Horo Zuria s e Dale Wabera n a w Tuka B Haru h e N Gimbichu t Kutaye e Yubdo W B Chwaka C a Goba Koricha a Leka a Gidami Boneya Boshe D M A Dale Sadi l Gemechis J I e Sayo Nole Dulecha lu k Nole Kaba i Tikur Alem o l D Lalo Kile Wama Hagalo o b r Yama Logi Welel Akaki a a a Enchini i Dawo ' b Meko n Gena e U Anchar a Midega Tola h a G Dabo a t t M Babile o Jimma Nunu c W e H l d m i K S i s a Kersana o f Hana Arjo D n Becho A o t -

Ethiopia: Administrative Map (August 2017)
Ethiopia: Administrative map (August 2017) ERITREA National capital P Erob Tahtay Adiyabo Regional capital Gulomekeda Laelay Adiyabo Mereb Leke Ahferom Red Sea Humera Adigrat ! ! Dalul ! Adwa Ganta Afeshum Aksum Saesie Tsaedaemba Shire Indasilase ! Zonal Capital ! North West TigrayTahtay KoraroTahtay Maychew Eastern Tigray Kafta Humera Laelay Maychew Werei Leke TIGRAY Asgede Tsimbila Central Tigray Hawzen Medebay Zana Koneba Naeder Adet Berahile Region boundary Atsbi Wenberta Western Tigray Kelete Awelallo Welkait Kola Temben Tselemti Degua Temben Mekele Zone boundary Tanqua Abergele P Zone 2 (Kilbet Rasu) Tsegede Tselemt Mekele Town Special Enderta Afdera Addi Arekay South East Ab Ala Tsegede Mirab Armacho Beyeda Woreda boundary Debark Erebti SUDAN Hintalo Wejirat Saharti Samre Tach Armacho Abergele Sanja ! Dabat Janamora Megale Bidu Alaje Sahla Addis Ababa Ziquala Maychew ! Wegera Metema Lay Armacho Wag Himra Endamehoni Raya Azebo North Gondar Gonder ! Sekota Teru Afar Chilga Southern Tigray Gonder City Adm. Yalo East Belesa Ofla West Belesa Kurri Dehana Dembia Gonder Zuria Alamata Gaz Gibla Zone 4 (Fantana Rasu ) Elidar Amhara Gelegu Quara ! Takusa Ebenat Gulina Bugna Awra Libo Kemkem Kobo Gidan Lasta Benishangul Gumuz North Wello AFAR Alfa Zone 1(Awsi Rasu) Debre Tabor Ewa ! Fogera Farta Lay Gayint Semera Meket Guba Lafto DPubti DJIBOUTI Jawi South Gondar Dire Dawa Semen Achefer East Esite Chifra Bahir Dar Wadla Delanta Habru Asayita P Tach Gayint ! Bahir Dar City Adm. Aysaita Guba AMHARA Dera Ambasel Debub Achefer Bahirdar Zuria Dawunt Worebabu Gambela Dangura West Esite Gulf of Aden Mecha Adaa'r Mile Pawe Special Simada Thehulederie Kutaber Dangila Yilmana Densa Afambo Mekdela Tenta Awi Dessie Bati Hulet Ej Enese ! Hareri Sayint Dessie City Adm. -

OROMIA REGION - Regional 3W Map 07 December 2010
OROMIA REGION - Regional 3W Map 07 December 2010 CRS I SC-UK V Legend W Amhara S d S Farm Africa R S i E R C Benishangul R A V E CRS CARE MfM C GOAL C P n R W S o i I International Boundary SC-Denmark A , t Gumuz Afar C L c C P K Action Aid C A CARE Welthungerhilfe A CRS S U I M - I ! O C C IMC S S G S a CARE A WVE S Regional Boundary , SC-Denmark R R c m i SC-Denmark Dera C C a S r R f u u u c i C U E A Action Aid t r S m r n u f GOAL e R m R a r A m E IMC r i E C A b a I L L a R R Zonal Boundary K CARE ! f F o C Action Aid H s A a Hidabu Abote m r ! A A g a A r J x a a e A a C r Christian Aid C O d a C d r m O a r b O IMC Action Aid i W a M CA RE o J e I a G F G G G u e ! g L t n b r b e i a i i n i J o E S m u D a d Farm Africa Gerar Jarso R CARE Woreda Boundary E IMC u e p Kuyu E a ! Kiltu Kara m A i n ! o R ! S R C r ! a L Abay Chomen B Debre Libanos o ! Abuna G/Beret A M m M e A H e l o C en a m ks e ina r u Yaya Gulele Abichuna Gne'a C Ch Abe Dongoro ! a h s ! e i t c r a g f a u Nejo t IMC a ! r CRS No Data /No Intervention g E J ! W ! l a x Kombolcha o e R o ! d V e O b B i o ! ! s Guduru G J ib it Goro Gutu ! a r m b a Gudetu Kondole FHI Ke W a Mercy Corps b a s B u i ! r B Boji Dirmeji o t a Bila Seyo e i ! a r Jimma Genete l J d K L e g t s l Jeldu u E a ! d D ! u F Haro Maya e Guto Gida b M S u A m A o e B e M l R i d ! Boji Chekorsa Jimma Rare S ! D CARE GOAL CRS b a B b u A o Aleltu l e ! Kurfa Chele A g I O u f e e y G i u a S Mieso r Agriculture & Livestock i C r s t ! T a Mida KegnA a M Lalo Asabi im r K a ! ! G S Gobu -

The Case of Hidabu Abote District, North Shoa Zone of Oromia Region, Ethiopia Fekadu Adamu Negussie*
ISSN: 2455-815X DOI: https://dx.doi.org/10.17352/ijasft LIFE SCIENCES GROUP Received: 23 July, 2020 Research Article Accepted: 29 October, 2020 Published: 31 October, 2020 *Corresponding author: Fekadu Adamu Negussie, Impact of row planting teff Department of Agricultural Economics, College of Ag- riculture, Oda Bultum University, Chiro, Ethiopia, E-mail: fi [email protected] technology adoption on Keywords: Adoption; Impact; Probit; PSM; Row planting; Teff the income of smallholder https://www.peertechz.com farmers: The case of Hidabu Abote District, North Shoa Zone of Oromia Region, Ethiopia Fekadu Adamu Negussie* Department of Agricultural Economics, College of Agriculture, Oda Bultum University, Chiro, Ethiopia Abstract In Ethiopia, improved agricultural technologies, like row planting are promoted in the recent times in order to address low agricultural productivity. However, despite such production enhancing technologies, utilization of such technologies remained low in Ethiopia. This study is focusedon the impact of row planting teff technology adoption on the income of smallholder farmer in the context of Hidabu Abote District, North Shoa zone. The study uses cross-sectional data that were collected from 181 randomly selected smallholder farmers. The data were analyzed using descriptive, inferential statistics,and econometrics models. From the descriptive statistics, it was found that out of thirteen explanatory variables seven of them were a signifi cant difference among the groups. Results of the probit model revealed that, distance to central market, extension contact,off/non-farm income,farm size,household size, access to mass media,and access to credit affected the farmer’s adoption decision of the row planting of teff signifi cantly. -

Ethiopia Administrative Map As of 2013
(as of 27 March 2013) ETHIOPIA:Administrative Map R E Legend E R I T R E A North D Western \( Erob \ Tahtay Laelay National Capital Mereb Ahferom Gulomekeda Adiyabo Adiyabo Leke Central Ganta S Dalul P Afeshum Saesie Tahtay Laelay Adwa E P Tahtay Tsaedaemba Regional Capital Kafta Maychew Maychew Koraro Humera Asgede Werei Eastern A Leke Hawzen Tsimbila Medebay Koneba Zana Kelete Berahle Western Atsbi International Boundary Welkait Awelallo Naeder Tigray Wenberta Tselemti Adet Kola Degua Tsegede Temben Mekele Temben P Zone 2 Undetermined Boundary Addi Tselemt Tanqua Afdera Abergele Enderta Arekay Ab Ala Tsegede Beyeda Mirab Armacho Debark Hintalo Abergele Saharti Erebti Regional Boundary Wejirat Tach Samre Megale Bidu Armacho Dabat Janamora Alaje Lay Sahla Zonal Boundary Armacho Wegera Southern Ziquala Metema Sekota Endamehoni Raya S U D A N North Wag Azebo Chilga Yalo Amhara East Ofla Teru Woreda Boundary Gonder West Belesa Himra Kurri Gonder Dehana Dembia Belesa Zuria Gaz Alamata Zone 4 Quara Gibla Elidar Takusa I Libo Ebenat Gulina Lake Kemkem Bugna Kobo Awra Afar T Lake Tana Lasta Gidan (Ayna) Zone 1 0 50 100 200 km Alfa Ewa U Fogera North Farta Lay Semera ¹ Meket Guba Lafto Semen Gayint Wollo P O Dubti Jawi Achefer Bahir Dar East Tach Wadla Habru Chifra B G U L F O F A D E N Delanta Aysaita Creation date:27 Mar.2013 P Dera Esite Gayint I Debub Bahirdar Ambasel Dawunt Worebabu Map Doc Name:21_ADM_000_ETH_032713_A0 Achefer Zuria West Thehulederie J Dangura Simada Tenta Sources:CSA (2007 population census purpose) and Field Pawe Mecha -

Determinants of Smallholder Farmers' Decision to Adopt Adaptation
Amare and Simane Agric & Food Secur (2017) 6:64 DOI 10.1186/s40066-017-0144-2 Agriculture & Food Security RESEARCH Open Access Determinants of smallholder farmers’ decision to adopt adaptation options to climate change and variability in the Muger Sub basin of the Upper Blue Nile basin of Ethiopia Abayineh Amare* and Belay Simane Abstract Smallholder farmers’ decisions to adopt adaptation options in response to climate change and variability are infu- enced by socioeconomic, institutional, and environmental factors, indicating that decision patterns can be very specifc to a given locality. The prime objective of this research is to identify factors afecting smallholder farmers’ decisions to adopt adaptation options to climate change and variability in the Muger River sub-basin of the Blue Nile basin of Ethiopia. Both quantitative and qualitative data were collected using a semi-structured questionnaire, focused group discussions, and key informant interviews from 442 sampled households. Frequency, mean, Chi-square test, and one-way ANOVA were used for analysis. Furthermore, a multinomial logit model was employed to analyze the data. Results signifed that small-scale irrigation, agronomic practices, livelihood diversifcation, and soil and water conservation measures are the dominant adaptation options that smallholder farmers used to limit the negative impact of climate change and variability in the study area. The results further revealed that adoption of small-scale irrigation as an adaptation to climate change and variability is signifcantly and positively infuenced by access to credit, social capital, and the educational status of household heads. Greater distance to marketplace and size of farmland negatively afected the use of agronomic practices, whereas crop failure experience and access to early warning systems have a positive infuence.