Phosphotyrosine Profiling of Curcumin-Induced Signaling
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SRC Antibody - N-Terminal Region (ARP32476 P050) Data Sheet
SRC antibody - N-terminal region (ARP32476_P050) Data Sheet Product Number ARP32476_P050 Product Name SRC antibody - N-terminal region (ARP32476_P050) Size 50ug Gene Symbol SRC Alias Symbols ASV; SRC1; c-SRC; p60-Src Nucleotide Accession# NM_005417 Protein Size (# AA) 536 amino acids Molecular Weight 60kDa Product Format Lyophilized powder NCBI Gene Id 6714 Host Rabbit Clonality Polyclonal Official Gene Full Name V-src sarcoma (Schmidt-Ruppin A-2) viral oncogene homolog (avian) Gene Family SH2D This is a rabbit polyclonal antibody against SRC. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Peptide Sequence Synthetic peptide located within the following region: QTPSKPASADGHRGPSAAFAPAAAEPKLFGGFNSSDTVTSPQRAGPLAGG This gene is highly similar to the v-src gene of Rous sarcoma virus. This proto-oncogene may play a role in the Description of Target regulation of embryonic development and cell growth. SRC protein is a tyrosine-protein kinase whose activity can be inhibited by phosphorylation by c-SRC kinase. Mutations in this gene could be involved in the -

Deregulated Gene Expression Pathways in Myelodysplastic Syndrome Hematopoietic Stem Cells
Leukemia (2010) 24, 756–764 & 2010 Macmillan Publishers Limited All rights reserved 0887-6924/10 $32.00 www.nature.com/leu ORIGINAL ARTICLE Deregulated gene expression pathways in myelodysplastic syndrome hematopoietic stem cells A Pellagatti1, M Cazzola2, A Giagounidis3, J Perry1, L Malcovati2, MG Della Porta2,MJa¨dersten4, S Killick5, A Verma6, CJ Norbury7, E Hellstro¨m-Lindberg4, JS Wainscoat1 and J Boultwood1 1LRF Molecular Haematology Unit, NDCLS, John Radcliffe Hospital, Oxford, UK; 2Department of Hematology Oncology, University of Pavia Medical School, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; 3Medizinische Klinik II, St Johannes Hospital, Duisburg, Germany; 4Division of Hematology, Department of Medicine, Karolinska Institutet, Stockholm, Sweden; 5Department of Haematology, Royal Bournemouth Hospital, Bournemouth, UK; 6Albert Einstein College of Medicine, Bronx, NY, USA and 7Sir William Dunn School of Pathology, University of Oxford, Oxford, UK To gain insight into the molecular pathogenesis of the the World Health Organization.6,7 Patients with refractory myelodysplastic syndromes (MDS), we performed global gene anemia (RA) with or without ringed sideroblasts, according to expression profiling and pathway analysis on the hemato- poietic stem cells (HSC) of 183 MDS patients as compared with the the French–American–British classification, were subdivided HSC of 17 healthy controls. The most significantly deregulated based on the presence or absence of multilineage dysplasia. In pathways in MDS include interferon signaling, thrombopoietin addition, patients with RA with excess blasts (RAEB) were signaling and the Wnt pathways. Among the most signifi- subdivided into two categories, RAEB1 and RAEB2, based on the cantly deregulated gene pathways in early MDS are immuno- percentage of bone marrow blasts. -

PTPRK Expression Is Downregulated in Drug Resistant Ovarian Cancer Cell Lines, and Especially in ALDH1A1 Positive Cscs-Like Popu
Article PTPRK Expression Is Downregulated in Drug Resistant Ovarian Cancer Cell Lines, and Especially in ALDH1A1 Positive CSCs‐Like Populations Monika Świerczewska 1,*, Karolina Sterzyńska 1, Karolina Wojtowicz 1, Dominika Kaźmierczak 1, Dariusz Iżycki 2, Michał Nowicki 1, Maciej Zabel 1,3 and Radosław Januchowski 1 1 Department of Histology and Embryology, Poznan University of Medical Sciences, Święcickiego 6 St., 61‐781 Poznań, Poland; [email protected] (K.S.); [email protected] (K.W.); [email protected] (D.K.); [email protected] (M.N.); [email protected] (M.Z.); [email protected] (R.J.) 2 Department of Cancer Immunology, Poznan University of Medical Sciences, Garbary 15 St., 61‐866 Poznań, Poland; [email protected] 3 Department of Anatomy and Histology, University of Zielona Góra, Licealna 9 St., 65‐417 Zielona Góra, Poland * Correspondence: [email protected]; Tel.: +48‐61‐8546428 Received: 26 March 2019; Accepted: 24 April 2019; Published: 25 April 2019 Abstract: Background: Ovarian cancer is the 7th most common cancer and 8th most mortal cancer among woman. The standard treatment includes cytoreduction surgery followed by chemotherapy. Unfortunately, in most cases, after treatment, cancer develops drug resistance. Decreased expression and/or activity of protein phosphatases leads to increased signal transduction and development of drug resistance in cancer cells. Methods: Using sensitive (W1, A2780) and resistant ovarian cancer cell lines, the expression of Protein Tyrosine Phosphatase Receptor Type K (PTPRK) was performed at the mRNA (real‐time PCR analysis) and protein level (Western blot, immunofluorescence analysis). The protein expression in ovarian cancer tissues was determined by immunohistochemistry. -

Atlas Antibodies in Breast Cancer Research Table of Contents
ATLAS ANTIBODIES IN BREAST CANCER RESEARCH TABLE OF CONTENTS The Human Protein Atlas, Triple A Polyclonals and PrecisA Monoclonals (4-5) Clinical markers (6) Antibodies used in breast cancer research (7-13) Antibodies against MammaPrint and other gene expression test proteins (14-16) Antibodies identified in the Human Protein Atlas (17-14) Finding cancer biomarkers, as exemplified by RBM3, granulin and anillin (19-22) Co-Development program (23) Contact (24) Page 2 (24) Page 3 (24) The Human Protein Atlas: a map of the Human Proteome The Human Protein Atlas (HPA) is a The Human Protein Atlas consortium cell types. All the IHC images for Swedish-based program initiated in is mainly funded by the Knut and Alice the normal tissue have undergone 2003 with the aim to map all the human Wallenberg Foundation. pathology-based annotation of proteins in cells, tissues and organs expression levels. using integration of various omics The Human Protein Atlas consists of technologies, including antibody- six separate parts, each focusing on References based imaging, mass spectrometry- a particular aspect of the genome- 1. Sjöstedt E, et al. (2020) An atlas of the based proteomics, transcriptomics wide analysis of the human proteins: protein-coding genes in the human, pig, and and systems biology. mouse brain. Science 367(6482) 2. Thul PJ, et al. (2017) A subcellular map of • The Tissue Atlas shows the the human proteome. Science. 356(6340): All the data in the knowledge resource distribution of proteins across all eaal3321 is open access to allow scientists both major tissues and organs in the 3. -

Interplay Between Coding and Exonic Splicing Regulatory Sequences
Downloaded from genome.cshlp.org on October 4, 2021 - Published by Cold Spring Harbor Laboratory Press Research Interplay between coding and exonic splicing regulatory sequences Nicolas Fontrodona,1,4 Fabien Aubé,1,4 Jean-Baptiste Claude,1 Hélène Polvèche,1,5 Sébastien Lemaire,1 Léon-Charles Tranchevent,2 Laurent Modolo,3 Franck Mortreux,1 Cyril F. Bourgeois,1 and Didier Auboeuf1 1Université Lyon, ENS de Lyon, Université Claude Bernard, CNRS UMR 5239, INSERM U1210, Laboratory of Biology and Modelling of the Cell, F-69007, Lyon, France; 2Proteome and Genome Research Unit, Department of Oncology, Luxembourg Institute of Health (LIH), L-1445 Strassen, Luxembourg; 3LBMC Biocomputing Center, CNRS UMR 5239, INSERM U1210, F-69007, Lyon, France The inclusion of exons during the splicing process depends on the binding of splicing factors to short low-complexity reg- ulatory sequences. The relationship between exonic splicing regulatory sequences and coding sequences is still poorly un- derstood. We demonstrate that exons that are coregulated by any given splicing factor share a similar nucleotide composition bias and preferentially code for amino acids with similar physicochemical properties because of the nonran- domness of the genetic code. Indeed, amino acids sharing similar physicochemical properties correspond to codons that have the same nucleotide composition bias. In particular, we uncover that the TRA2A and TRA2B splicing factors that bind to adenine-rich motifs promote the inclusion of adenine-rich exons coding preferentially for hydrophilic amino acids that correspond to adenine-rich codons. SRSF2 that binds guanine/cytosine-rich motifs promotes the inclusion of GC-rich exons coding preferentially for small amino acids, whereas SRSF3 that binds cytosine-rich motifs promotes the inclusion of exons coding preferentially for uncharged amino acids, like serine and threonine that can be phosphorylated. -
Sample Lab Report
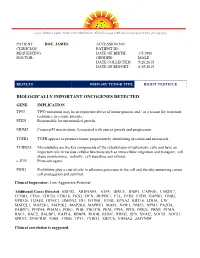
3030 Venture Lane, Suite 108 ● Melbourne, Florida 32934 ● Phone 321-253-5197 ● Fax 321-253-5199 PATIENT: DOE, JAMES ACCESSION NO: CLINICIAN/ PATIENT ID: REQUESTING DATE OF BIRTH: 1/5/1986 DOCTOR: GENDER: MALE DATE COLLECTED: 5/26/2015 DATE OF REPORT: 6/15/2015 RESULTS PRIMARY TUMOR TYPE RIGHT TESTICLE BIOLOGICALLY IMPORTANT ONCOGENES DETECTED GENE IMPLICATION TP53 TP53 mutations may be an important driver of tumorigenesis and / or a reason for treatment resistance in a some patients. PTEN Responsible for uncontrolled growth. MDM2 Causes p53 inactivation. Associated with cancer growth and progression. TGFB1 TGFB appears to promote tumor progession by stimulating invasion and metastasis. TUBB2A Microtubules are the key components of the cytoskeleton of eukaryotic cells and have an important role in various cellular functions such as intracellular migration and transport, cell shape maintenance, polarity, cell signaling and mitosis. c-JUN Proto-oncogene PHB2 Prohibitins play a crucial role in adhesion processes in the cell and thereby sustaining cancer cell propagation and survival. Clinical Impression: Low Aggressive Potential Additional Genes Detected: ABCG2, ARHGAP5, ATF4, BIRC5, BNIP3, CAPNS1, CARD17, CCNB1, CD24, CDC20, CDK18, CKS2, DCN, DEPDC1, FTL, FZD5, FZD9, GAPDH, GNB2, GPR126, H2AFZ, HDAC1, HMGN2, ID1, IFITM1, JUNB, KPNA2, KRT18, LDHA, LTF, MAD2L1, MAP2K1, MAP2K2, MAP2K4, MAPRE1, MAS1, NME1, NME3, NPM1, PA2G4, PABPC1, PFDN4, PGAM1, PGK1, PHB, PIK3CB, PKM, PPIA, PPIH, PRKX, PRNP, PTMA, RAC1, RAC2, RALBP1, RAP1A, RBBP4, RHOB, RHOC, -

Stefano Sellitto 19-05-2020.Pdf
RNA Binding Proteins: from physiology to pathology An update Stefano Sellitto RBPs regulate the RNA metabolism A ‘conventional’ RNA-Binding Protein (RBP) participates in the formation of ribonucleoprotein (RNP) complexes that are principally involved in gene expression. Keene, 2007 High-Throughuput sequencing to study the RBPs world RIP-Seq (i)CLIP PAR-CLIP Hentze et al., 2018 The concept of RNA operon The RBPs profile is highly dynamic The combinatorial association of many RBPs acting in trans on RNA molecules results in the metabolic regulation of a distinct RNA subpopulations. Keene, 2007 The molecular features of protein-RNA interactions "Classical" RNA-Binding Domains Lunde et al., 2007 "Classical" RNA-Binding Domains RNA-recognition motif (RRM) double-stranded RNA-binding motif (dsRBM) Zinc-finger motif Stefl et al., 2005 Modularity of RBPs RBPs are usually composed by several repeated domains Lunde et al., 2007 Expanding the concept of the RNA Binding Hentze et al., 2018 Novel types of RNA binding Hentze et al., 2018 Lunde et al., 2007 RNA metabolism and neurological diseases RNA binding proteins preserves neuronal integrity De Conti et al., 2017 Alterations of RBPs in neurological disorders Nussbacher et al., 2019 Microsatellite expansion in FXS: reduced FMR1 transcription The reduction of FMRP levels induces an overexpressed LTD activity Bassell & Warren, 2008 Huber et al., 2002 Microsatellite expansion in FXTAS: FMR1 RNA-meidated toxicity FMR1 expanded RNA impairs the miRNA processing Sellier et al., 2013 Loss-of-function VS Gain-of-function Park et al., 2015 TDP-43 and FUS/TLS Ling et al., 2013 TDP-43 and FUS/TLS in ALS and FTD Ling et al., 2013 Cookson, 2017 Loss-of-function VS Gain-of-function Nucelar clearance (LOF) TDP-43 Nuclear TDP-43 (LOF) Loss of TDP-43 negative autoregulation Nucleus Abolishing RNA binding ability Cytoplasmatic stress (GOF) mitigates mutant TDP-43 toxicity Prevent mutant TDP-43 toxic activity on RNAs (GOF) Ihara et al., 2013 . -

Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma
ARTICLE https://doi.org/10.1038/s41467-020-16164-1 OPEN Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma Nayoung Kim 1,2,3,13, Hong Kwan Kim4,13, Kyungjong Lee 5,13, Yourae Hong 1,6, Jong Ho Cho4, Jung Won Choi7, Jung-Il Lee7, Yeon-Lim Suh8,BoMiKu9, Hye Hyeon Eum 1,2,3, Soyean Choi 1, Yoon-La Choi6,10,11, Je-Gun Joung1, Woong-Yang Park 1,2,6, Hyun Ae Jung12, Jong-Mu Sun12, Se-Hoon Lee12, ✉ ✉ Jin Seok Ahn12, Keunchil Park12, Myung-Ju Ahn 12 & Hae-Ock Lee 1,2,3,6 1234567890():,; Advanced metastatic cancer poses utmost clinical challenges and may present molecular and cellular features distinct from an early-stage cancer. Herein, we present single-cell tran- scriptome profiling of metastatic lung adenocarcinoma, the most prevalent histological lung cancer type diagnosed at stage IV in over 40% of all cases. From 208,506 cells populating the normal tissues or early to metastatic stage cancer in 44 patients, we identify a cancer cell subtype deviating from the normal differentiation trajectory and dominating the metastatic stage. In all stages, the stromal and immune cell dynamics reveal ontological and functional changes that create a pro-tumoral and immunosuppressive microenvironment. Normal resident myeloid cell populations are gradually replaced with monocyte-derived macrophages and dendritic cells, along with T-cell exhaustion. This extensive single-cell analysis enhances our understanding of molecular and cellular dynamics in metastatic lung cancer and reveals potential diagnostic and therapeutic targets in cancer-microenvironment interactions. 1 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea. -
Conditional Ablation of P130cas/BCAR1 Adaptor Protein
Camacho Leal et al. Cell Communication and Signaling (2018) 16:73 https://doi.org/10.1186/s12964-018-0289-z RESEARCH Open Access Conditional ablation of p130Cas/BCAR1 adaptor protein impairs epidermal homeostasis by altering cell adhesion and differentiation Maria del Pilar Camacho Leal†, Andrea Costamagna†, Beatrice Tassone, Stefania Saoncella, Matilde Simoni, Dora Natalini, Aurora Dadone, Marianna Sciortino, Emilia Turco, Paola Defilippi, Enzo Calautti‡ and Sara Cabodi*‡ Abstract Background: p130 Crk-associated substrate (p130CAS; also known as BCAR1) is a scaffold protein that modulates many essential cellular processes such as cell adhesion, proliferation, survival, cell migration, and intracellular signaling. p130Cas has been shown to be highly expressed in a variety of human cancers of epithelial origin. However, few data are available regarding the role of p130Cas during normal epithelial development and homeostasis. Methods: To this end, we have generated a genetically modified mouse in which p130Cas protein was specifically ablated in the epidermal tissue. Results: By using this murine model, we show that p130Cas loss results in increased cell proliferation and reduction of cell adhesion to extracellular matrix. In addition, epidermal deletion of p130Cas protein leads to premature expression of “late” epidermal differentiation markers, altered membrane E-cadherin/catenin proteins localization and aberrant tyrosine phosphorylation of E-cadherin/catenin complexes. Interestingly, these alterations in adhesive properties in absence -

Expression Profiling of KLF4
Expression Profiling of KLF4 AJCR0000006 Supplemental Data Figure S1. Snapshot of enriched gene sets identified by GSEA in Klf4-null MEFs. Figure S2. Snapshot of enriched gene sets identified by GSEA in wild type MEFs. 98 Am J Cancer Res 2011;1(1):85-97 Table S1: Functional Annotation Clustering of Genes Up-Regulated in Klf4 -Null MEFs ILLUMINA_ID Gene Symbol Gene Name (Description) P -value Fold-Change Cell Cycle 8.00E-03 ILMN_1217331 Mcm6 MINICHROMOSOME MAINTENANCE DEFICIENT 6 40.36 ILMN_2723931 E2f6 E2F TRANSCRIPTION FACTOR 6 26.8 ILMN_2724570 Mapk12 MITOGEN-ACTIVATED PROTEIN KINASE 12 22.19 ILMN_1218470 Cdk2 CYCLIN-DEPENDENT KINASE 2 9.32 ILMN_1234909 Tipin TIMELESS INTERACTING PROTEIN 5.3 ILMN_1212692 Mapk13 SAPK/ERK/KINASE 4 4.96 ILMN_2666690 Cul7 CULLIN 7 2.23 ILMN_2681776 Mapk6 MITOGEN ACTIVATED PROTEIN KINASE 4 2.11 ILMN_2652909 Ddit3 DNA-DAMAGE INDUCIBLE TRANSCRIPT 3 2.07 ILMN_2742152 Gadd45a GROWTH ARREST AND DNA-DAMAGE-INDUCIBLE 45 ALPHA 1.92 ILMN_1212787 Pttg1 PITUITARY TUMOR-TRANSFORMING 1 1.8 ILMN_1216721 Cdk5 CYCLIN-DEPENDENT KINASE 5 1.78 ILMN_1227009 Gas2l1 GROWTH ARREST-SPECIFIC 2 LIKE 1 1.74 ILMN_2663009 Rassf5 RAS ASSOCIATION (RALGDS/AF-6) DOMAIN FAMILY 5 1.64 ILMN_1220454 Anapc13 ANAPHASE PROMOTING COMPLEX SUBUNIT 13 1.61 ILMN_1216213 Incenp INNER CENTROMERE PROTEIN 1.56 ILMN_1256301 Rcc2 REGULATOR OF CHROMOSOME CONDENSATION 2 1.53 Extracellular Matrix 5.80E-06 ILMN_2735184 Col18a1 PROCOLLAGEN, TYPE XVIII, ALPHA 1 51.5 ILMN_1223997 Crtap CARTILAGE ASSOCIATED PROTEIN 32.74 ILMN_2753809 Mmp3 MATRIX METALLOPEPTIDASE -

Domain Requires the Gab2 Pleckstrin Homology Negative Regulation Of
Ligation of CD28 Stimulates the Formation of a Multimeric Signaling Complex Involving Grb-2-Associated Binder 2 (Gab2), Src Homology Phosphatase-2, and This information is current as Phosphatidylinositol 3-Kinase: Evidence That of October 1, 2021. Negative Regulation of CD28 Signaling Requires the Gab2 Pleckstrin Homology Domain Richard V. Parry, Gillian C. Whittaker, Martin Sims, Downloaded from Christine E. Edmead, Melanie J. Welham and Stephen G. Ward J Immunol 2006; 176:594-602; ; doi: 10.4049/jimmunol.176.1.594 http://www.jimmunol.org/content/176/1/594 http://www.jimmunol.org/ References This article cites 59 articles, 38 of which you can access for free at: http://www.jimmunol.org/content/176/1/594.full#ref-list-1 Why The JI? Submit online. by guest on October 1, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2006 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Ligation of CD28 Stimulates the Formation of a Multimeric Signaling Complex Involving Grb-2-Associated Binder 2 (Gab2), Src Homology Phosphatase-2, and Phosphatidylinositol 3-Kinase: Evidence That Negative Regulation of CD28 Signaling Requires the Gab2 Pleckstrin Homology Domain1 Richard V. -

Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration Through Promotion of P130cas Membrane Localization Andmembrane Ruffling
Research Article Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration through Promotion of p130Cas Membrane Localization andMembrane Ruffling Randy S. Schrecengost,1 Rebecca B. Riggins,2 Keena S. Thomas,1 Michael S. Guerrero,1 and Amy H. Bouton1 1Department of Microbiology, University of Virginia Health System, Charlottesville, Virginia and 2Department of Oncology, Lombardi Comprehensive Cancer Center, Georgetown University, Washington, District of Columbia Abstract antiestrogen resistance-1 (BCAR1; also known as p130Cas; refs. 2, 3). Antiestrogens such as tamoxifen are widely used in the clinic A second protein, BCAR3 (the human homologue of the murine to treat estrogen receptor–positive breast tumors. Resistance protein AND-34), was identified in a genetic screen along with to tamoxifen can occur either de novo or develop over time in BCAR1 as a gene product whose overexpression conferred tamoxifen resistance in vitro (4). BCAR3 is a member of the novel a large proportion of these tumors. Additionally, resistance is S p associated with enhanced motility and invasiveness in vitro. rc homology 2 (SH2)–containing rotein (NSP) family that One molecule that has been implicated in tamoxifen resis- includes two other members, Chat/SHEP1 and NSP1. These tance, breast cancer antiestrogen resistance-3 (BCAR3), has proteins share a common domain structure consisting of an also been shown to regulate migration of fibroblasts. In this amino-terminal SH2 domain and a carboxyl-terminal domain with study, we investigated the role of BCAR3 in breast cancer cell sequence homology to the Cdc25-family of guanine nucleotide exchange factors (GEF). Several studies have shown that BCAR3 migration and invasion.