Methods for Identifying Culprit Drugs in Cutaneous Drug Eruptions: a Scoping Review Reetesh Bose M.D., B.Sc1,2, Selam Ogbalidet3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Implementation of the Operating Room Black Box Research Program at the Ottawa Hospital Through Patient, Clinical, and Organizational Engagement: Case Study
JOURNAL OF MEDICAL INTERNET RESEARCH Boet et al Original Paper Implementation of the Operating Room Black Box Research Program at the Ottawa Hospital Through Patient, Clinical, and Organizational Engagement: Case Study Sylvain Boet1,2,3,4, MD, PhD; Cole Etherington1,2, PhD; Sandy Lam1,2, RRT, MSc; Maxime Lê5, BHSc, MA; Laurie Proulx5, BA; Meghan Britton6, BScN; Julie Kenna6, BScN; Antoine Przybylak-Brouillard1,2, MA; Jeremy Grimshaw2, MBChB, PhD; Teodor Grantcharov7,8, MD, PhD; Sukhbir Singh9, MD 1Department of Anesthesiology and Pain Medicine, University of Ottawa, Ottawa, ON, Canada 2Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON, Canada 3Department of Innovation in Medical Education, University of Ottawa, Ottawa, ON, Canada 4Francophone Affairs, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada 5Patient and Family Advisory Council, The Ottawa Hospital, Ottawa, ON, Canada 6Main Operating Room, The Ottawa Hospital, Ottawa, ON, Canada 7Department of General Surgery, University of Toronto, Toronto, ON, Canada 8Li Ka Shing Knowledge Institute, St. Michael©s Hospital, Toronto, ON, Canada 9Department of Obstetrics, Gynecology, and Newborn Care, University of Ottawa, Ottawa, ON, Canada Corresponding Author: Sylvain Boet, MD, PhD Department of Anesthesiology and Pain Medicine University of Ottawa 501 Smyth Road Ottawa, ON, K1H 8L6 Canada Phone: 1 613 798 5555 ext 78187 Email: [email protected] Abstract Background: A large proportion of surgical patient harm is preventable; yet, our ability to systematically learn from these incidents and improve clinical practice remains limited. The Operating Room Black Box was developed to address the need for comprehensive assessments of clinical performance in the operating room. It captures synchronized audio, video, patient, and environmental clinical data in real time, which are subsequently analyzed by a combination of expert raters and software-based algorithms. -

City of Ottawa Transportation Committee
City of Ottawa Transportation Committee Councillor Keith Egli Pictures Left: Main Street Renewal The $39 million Main Street Renewal Project began construction in 2015 after extensive consultations with the area’s businesses, residents, and community organizations. The project involved a renewal of the street’s infrastructure following the City’s complete street guidelines, aiming to link the street together as a unified corridor and create memorable places along it while recognizing and supporting the character of its communities. The infrastructure of Main Street has been renewed and revitalized, and now provides better options for walking, cycling, and transit use. Middle: Rideau Canal Crossing: The construction has started! 2 years of planned construction. Multi-use pedestrian and cyclist bridge over the Rideau Canal and Colonel By Drive Reduces distances between mid-town neighbourhoods Improves access to the City’s extensive network of pedestrian multi-use pathways and to Lansdowne Right: Mackenzie Cycle Track Officially opened on Friday May 19 2017. The track is bi-directional, similar to the cycle track along O’Connor Street, and runs along the east side of Mackenzie Avenue, from Rideau Street to Murray Street. Mackenzie Avenue remains a one-way, two-lane roadway, expanding to three lanes at the Rideau Street intersection. The cycle track is separated from road traffic on Mackenzie Avenue by a combination of curbs, a buffer area, and bollards in front of the U.S. Embassy.The cycle track was opened during Bike to Work Month and is part of a larger project that involved the resurfacing of Mackenzie Avenue and installation of security bollards in front of the U.S. -
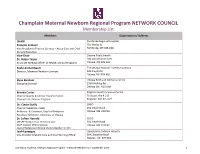
Champlain Maternal Newborn Regional Program NETWORK
Champlain Maternal Newborn Regional Program NETWORK COUNCIL Membership List Members Organization / Address CHAIR Pembroke Regional Hospital François Lemaire 705 McKay St. Vice President of Patient Services – Acute Care and Chief Pembroke, ON K8A 1G8 Nursing Executive Vice-Chair Ottawa Public Health Dr. Robin Taylor 100 Constellation Cres. Associate Medical Officer of Health, Clinical Programs Ottawa, ON K2G 6J8 Paula Archambault The Ottawa Hospital – General Campus Director, Maternal Newborn Services 501 Smyth Rd. Ottawa ON K1H 8L6 Elyse Banham Ottawa Birth and Wellness Centre Executive Director 2260 Walkley Rd. Ottawa ON K1G 6A8 Brenda Carter Kingston Health Sciences Centre Chief of Quality & Clinical Transformation 76 Stuart, Rm 4-217 Women’s & Children Program Kingston ON K7L 2V7 Dr. Ciaràn Duffy CHEO Chief of Pediatrics, CHEO 401 Smyth Road Professor & Chairman, Dep’t of Pediatrics Ottawa ON K1H 8L1 Faculty of Medicine, University of Ottawa Dr. JoAnn Harrold CHEO CMNRP Medical Lead - Newborn Care 401 Smyth Road Chief, Division of Neonatology Ottawa ON K1H 8L1 Dept of Pediatrics (CHEO) & Ob-Gyn-Newborn (TOH) Leah Levesque Queensway Carleton Hospital Vice President Patient Care and Chief Nursing Officer 3045 Baseline Road Nepean ON K2H 8P4 Champlain Maternal Newborn Regional Program - Network Membership – September 2019 1 Members Organization / Address Ann Lynch CHEO Vice President, Acute Care & Chief Nursing Executive 401 Smyth Road Ottawa ON K1H 8L1 Suzanne Robichaud Hôpital Montfort Vice President Clinical Services and Chief Nursing Officer 713 chemin Montreal Ottawa ON K1K 0T2 Nancy Shaw Perth and Smiths Falls District Hospital Vice President Clinical Services 60 Cornelia St. W. Smiths Falls, ON K7A 2H9 Mari Teitelbaum CHEO Vice President Technology & Chief Information Officer; 401 Smyth Rd. -

A Qualitative Investigation of How EHR Use Obstructs a Vital Clinical Activity
International Journal of Medical Informatics 84 (2015) 1019–1028 Contents lists available at ScienceDirect International Journal of Medical Informatics j ournal homepage: www.ijmijournal.com The EHR and building the patient’s story: A qualitative investigation of how EHR use obstructs a vital clinical activity a,b,∗ c,d e f g Lara Varpio , Judy Rashotte , Kathy Day , James King , Craig Kuziemsky , h Avi Parush a Department of Medicine, Uniformed Services University for the Health Sciences, 4301 Jones Bridge Road, Bethesda, MD, USA b Academy for Innovation in Medical Education, Faculty of Medicine, University of Ottawa, 451 Smyth Road, Ottawa, Ontario, Canada c Nursing Research, Children’s Hospital of Eastern Ontario, 401 Smyth Road, Ottawa, Ontario, Canada d School of Nursing, Faculty of Health Sciences, University of Ottawa, 451 Smyth Road, Ottawa, Ontario, Canada e Academy for Innovation in Medical Education, Faculty of Medicine, University of Ottawa, 451 Smyth Road, Ottawa, Ontario, Canada f Children’s Hospital of Eastern Ontario, 401 Smyth Road, Ottawa, Ontario, Canada g Telfer School of Management, University of Ottawa, 55 Laurier Avenue East, Ottawa, Ontario, Canada h Department of Psychology, Carleton University, Loeb B550, 1125 Colonel By Drive, Ottawa, Ontario, Canada a r t i c l e i n f o a b s t r a c t Article history: Background: Recent research has suggested that using electronic health records (EHRs) can negatively Received 2 June 2015 impact clinical reasoning (CR) and interprofessional collaborative practices (ICPs). Understanding the Received in revised form 19 August 2015 benefits and obstacles that EHR use introduces into clinical activities is essential for improving medical Accepted 11 September 2015 documentation, while also supporting CR and ICP. -

EMBASSY of the UNITED STATES of AMERICA 490 Sussex Drive Ottawa, Ontario K1N 1G8
EMBASSY OF THE UNITED STATES OF AMERICA 490 Sussex Drive Ottawa, Ontario K1N 1G8 LIST OF PHYSICIANS 2018 DISCLAIMER: The U.S. Embassy Ottawa, Canada assumes no responsibility or liability for the professional ability or reputation of, or the quality of services provided by, the medical professionals, medical facilities or air ambulance services whose names appear on the following lists. Inclusion on this list is in no way an endorsement by the Department of State or the U.S. Embassy/Consulate. Names are listed alphabetically, and the order in which they appear has no other significance. The information in the list on professional credentials and areas of expertise are provided directly by the medical professional, medical facility or air ambulance service; the Embassy/Consulate is not in a position to vouch for such information. You may receive additional information about the individuals and facilities on the list by contacting local medical boards and associations (or its equivalent) or local licensing authorities. GENERAL MEDICAL INFORMATION IN THE EVENT OF AN EMERGENCY, DIAL 911 This is a universal number and will bring emergency service, i.e. ambulance, police, fire department, to any locale in Ottawa or its environs. Tell the operator where you are and what the emergency is. The operator will connect you to the service you need. If you are at a pay phone, just dial 911 – no money is required. The quickest way to obtain emergency medical service in non-threatening instances is to go directly to the Emergency Room at the nearest hospital (listed below). Medical care is provided throughout the province by the Ontario Health Insurance Plan (OHIP). -
APPENDIX a Transportation Reference Materials
LRT TRANSIT ORIENTED DEVELOPMENT STUDY AREAS SERVICING OVERVIEW Final Report, November 2013 APPENDIX A Transportation Reference Materials LRT TRANSIT ORIENTED DEVELOPMENT STUDY AREAS SERVICING OVERVIEW Final Report, November 2013 Existing Conditions 370000 375000 ± 5035000 5035000 Blair Rd. Montreal Rd. Macdonald Cartier Br. St. Laurent Blvd. ^_ Blair A Cyrville v i a 4 t 7 i 1 o d. n R P al k n w io y eg . R Train ^_ Lees ^_Hwy. 417 ^_Hwy. 417 ^_ St. Laurent Hw y. 417 ^_ Innes Rd. Main St. 5030000 Hurdman 5030000 Cycling Capture Area and Cycling Routes Smyth Rd. ^_ Future LRT Platform Bike Lane Multi-use Pathway Servicing Overview Study - Transportation Analysis Boundary Cycling Capture Area 0 500 1,000 Study Area Boundary m 1:50,000 V:\01225\active\other_pc\163401180\GIS\MXD\Powerpoint_Figures_08022013\163401180_PP_LRT_Cycling.mxdRevised: 2013-11-27 By: ncruikshank 370000 375000 370000 375000 74 . 1 Rd al ion eg ± R 5035000 5035000 ! ! ! ! Blair Rd. Montreal Rd. Macdonald Cartier Br. 4 17 d. l R St. Laurent Blvd. ! na io eg ! ! R ! ! ! Blair ^_ ! A Cyrville v i a !t io ! n P ! k w ! y ! !! . ! Train ! ^_ ! ! ! ! wy. 417 ! Lees ^_ H ! ! ! ! ! Hwy. 417 ! ^_ ! ^_ ! ! St. Laurent Hw ! y. 417 !! ^_ !! ! Innes Rd. Main St. ! 5030000 Hurdman 5030000 LRT Intersections ! Smyth Rd. ^_ Future LRT Platform ! ! TOD Study 1 Intersections ! TOD Study 2 Intersections Future LRT Cycling Capture Area Servicing Overview Study - Transportation Analysis Boundary Study Area Boundary 0 500 1,000 Approved TOD Area m 1:50,000 V:\01225\active\other_pc\163401180\GIS\MXD\Powerpoint_Figures_08022013\163401180_PP_LRT_Intersections.mxd Revised: By:2013-11-01 ncruikshank 370000 375000 City of Ottawa LOS A = 0.00 – 0.60 LOS B = 0.61 – 0.70 LOS C = 0.71 – 0.80 LOS D = 0.81 – 0.90 LOS E = 0.91 – 1.00 LOS F = > 1.00 All Intersections signalized unless otherwise noted. -

Services for Italian Speaking Seniors in Ottawa Contents
SERVICES FOR ITALIAN SPEAKING SENIORS IN OTTAWA Contents INFOline for Seniors .................................................................. 2 Telehealth Ontario ....................................................................... 2 How to Find a Doctor in Ontario ................................................. 3 Community Care Access Centre (CCAC) .................................... 4 Long Term Care Homes ............................................................... 4 Hospitals ...................................................................................... 5 Doctors Who Speak Italian .......................................................... 6 Dentists Who Speak Italian .......................................................... 8 Denturists Who Speak Italian ...................................................... 8 Drug Stores Where Italian is Spoken ........................................... 9 Counselling Services Where Italian is Spoken ............................ 9 Dieticians Who Speak Italian ..................................................... 10 Hair Care in the Home ............................................................... 10 Recreation Programs with Italian Seniors .................................. 10 Assistance with Italian/European Pensions ............................... 12 Legal Services ............................................................................ 12 Lawyers ...................................................................................... 12 Churches ................................................................................... -

EMERGENCY ACTION PLAN 2019-20 Nepean Ravens Tween AA (Coach)
EMERGENCY ACTION PLAN 2019-20 Nepean Ravens Tween AA (Coach) Emergency: 9-1-1 for all emergencies Manager: Name 613-xxx-xxxx Coach: Name 613-xxx-xxxx Manager: Name 613-xxx-xxxx A/Coach: Name 613-xxx-xxxx Trainer/AC: Name 613-xxx-xxxx A/Coach: Name 613-xxx-xxxx Home Facilities Nearest Hospital Directions Carleton University Ice House CHEO From Arena: Raven Road 401 Smyth Road Turn RIGHT onto University Drive (travel 750 m). Ottawa, ON K1S Ottawa, ON K1H 8L1 Turn RIGHT onto Bronson Ave. (travel 1 km). 613.247.2061 613.737.7600 Take RAMP onto Riverside Drive EAST (travel 2.4 km). 613.520.2600 ext 4655 Take RAMP onto Smythe Road EAST (travel 1.2 km). Turn LEFT at South Haven Place (follow signs to the Emergency Entrance). Merivale (Darwin) Arena Queensway Carleton From Arena: 1765 Merivale Road 3054 Baseline Road Turn LEFT onto Merivale Road (travel 750 m). Ottawa, ON K2G 1E1 Ottawa, ON K2H 8P4 Turn RIGHT onto West Hunt Club Road (travel 4.4 km). 613.224.3168 613.721.2000 Turn RIGHT onto Greenbank Road (travel 2.2 km). Turn LEFT onto Baseline Road (travel 1.5 km). Turn RIGHT onto John Sutherland Drive (follow signs to the Emergency Entrance). Nepean Sportsplex Queensway Carleton From Arena: 1701 Woodroffe Avenue 3054 Baseline Road Turn RIGHT onto Woodroffe (travel 200 m). Ottawa, ON K2G 1W2 Ottawa, ON K2H 8P4 Turn LEFT onto West Hunt Club Road (travel 2.3 km). 613.580.2828 613.721.2000 Turn RIGHT onto Greenbank Road (travel 2.2 km). -

Land Investment Opportunity
1867 Alta Vista Drive, Ottawa ON Land Investment Opportunity Michael Pyman Jordan Lovett Vice President Senior Sales Representative +1 613 683 2202 +1 613 683 2239 [email protected] [email protected] Accelerating success. Property Overview • Centrally positioned in the well- established neighbourhood, appealing to a broad base of Hurdman Station users • A large footprint and favorable zoning, permitting a wide variety of uses Smyth Station • Situated on the corner of Alta Vista Drive and Smyth Road and is minutes away from Alta Vista Shopping Centre and the Ottawa Train Yards • Within walking distance to public transportation and is nearby LRT Tremblay Station and the Ottawa VIA Rail Train Station • Property is free from contaminants with a recent, clean phase 1 report on file that is available upon request Alta Vista Drive with a signed Confidentiality Bus Transit Line Smyth Road Agreement (CA) Alta Vista/Smyth Bus Stop (1 minute walk) Highway 417 (3 minute drive) LRT (6 mintue drive to Hurdman Station) Property Salient Facts Highlights Civic Address 1867 Alta Vista Drive Legal Address PT LT 15, CON JG , AS IN N561626 ; OTTAWA/GLOUCESTER Site Area 2.99 Acres Frontage 472 Feet Current Zoning IP12 (F1.5) - Business Park Industrial Zone Total Buildable Area 195,000 SF Smyth Road Alta Vista Drive 8 Nearby 11 Tremblay Station Amenities VIA Rail Train Station 6 5 Hurdman Station 7 4 3 9 1867 Alta Vista Drive 1 Billings Bridge Shopping Centre 2 10 2 The Ottawa Hospital 3 CHEO 4 Alta Vista Shopping Centre 5 Ottawa Train Yards 6 Walmart 7 Farmboy 1 8 St. -

Health Care Partnership Pharmacy List (2018)
The Health Care Partnership (HCP)—between your employer and area pharmacies—helps you find discounted dispensing fees, competitive drug ingredient prices, and preferred service levels. By using an HCP pharmacy, you are partnering with your employer to manage costs and help sustain your Pharmacy list comprehensive coverage. Emergency Dispensing Area HCP pharmacy Address Telephone # Extended hours Delivery* services fee** Gloucester Blackburn Pharmacy 2559 Innes Road 613 830-1212 no yes no $8.83 Loblaws 1980 Ogilvie Road 613 746-9553 yes no no $8.83 The Medicine Shoppe 19-5303 Canoteck Road 613 745-5905 no no yes $8.83 Your Independent Grocer 1619 Orleans Boulevard 613 830-9914 yes no no $8.83 Your Independent Grocer 685 River Road 613 822-9878 yes no no $8.83 Wal-Mart Pharmacy 1980 Ogilvie Road 613 747-7384 no no no $8.83 Kanata Loblaws 200 Earl Grey Drive 613 599-4046 yes no no $8.83 Real Canadian Superstore 760 Eagleson Road 613 254-5334 yes no no $8.83 Wal-Mart Pharmacy 500 Earl Grey Drive 613 599-1343 yes no no $8.83 Nepean Canada Chemists Pharmacy 1 Centrepointe Drive 613 225-5070 no yes no $8.83 Cedarview Guardian 4100 Strandherd Drive 613 823-1700 no yes no $8.83 Pharmacy Centrepointe Gabriel Drugs 117 Centrepointe Drive 613 723-2366 no yes no $8.83 Food Basics Pharmacy 1465 Merivale Road 613 723-8887 no yes no $8.83 Loblaws 59A Robertson Road 613 829-4680 yes no no $8.83 Loblaws 3201 Greenbank Road 613 825-3748 yes no no $8.83 Loblaws 1980 Baseline Road 613 723-3100 yes no no $8.83 Wal-Mart Pharmacy 3651 Strandherd Drive 613 823-8717 -

Deligated Authority Doc 1
Document 1 Delegation of Authority - Acquisition of Land and Property - 1 April 2015 to 30 June 2015 Approved Approved Report Report Title Total Transaction By Number Expended 16-Jun-15 Program DEL2015- Temporary Easements - Hazeldean Pumping Station $ 3,385.00 Acquisition Manager REPDO-0049 Improvements - Arthur and Mary Van Gaal - 5331 Fernbank Road 15-Apr-15 Program DEL2015- Acquisition of Permanent Easement and Temporary $ 25,280.00 Acquisition Manager REPDO-0064 Occupancy of Land for Renewal of a Culvert Crossing Hiawatha Park Road - Sisters of Charity of Ottawa - Soeurs de la charité d'Ottawa, 879 Hiawatha Park Road, Ottawa 13-May-15 Manager DEL2015- Property Acquisition - Main Street Renewal Project - $ 132,450.00 Acquisition REPDO-0066 English Oblates of Eastern Canada, 100 Main Street, Ottawa 28-Apr-15 Program DEL2015- 249 Main Street - Public Art Loan Agreement - Université $ 1.00 Acquisition Manager REPDO-0068 Saint-Paul/Saint-Paul University 20-May-15 Director DEL2015- Land Acquisition - Taylor Creek Business Park - 1161 $ 74,235.00 Acquisition REPDO-0070 Vimont Court - Owner 6892639 Canada Inc. 28-Apr-15 Program DEL2015- Acquisition of a Permanent Easement for Replacement of $ 1.00 Acquisition Manager REPDO-0072 a Storm Sewer Over a Parcel of Land on Riverwood Drive, Ottawa from the Estate of Wilfred Barnet MacLaren 07-May-15 Program DEL2015- Interest Payment, Tenth Line Road Widening and $ 8,530.68 Acquisition Manager REPDO-0075 Urbanization Project, Richard Des Rivières and Estelle Des Rivières 20-May-15 Program DEL2015- -

Information Booklet: Patient Privacy: Ours to Protect
Patient Privacy. Ours to Protect. Information Booklet Patient Privacy: Ours to Protect Disclaimer This is general information developed by The Ottawa Hospital. It is not intended to replace the advice of a qualified health-care provider. Please consult your health-care provider who will be able to determine the appropriateness of the information for your specific situation. P1043 (10/2012) Printed at The Ottawa Hospital What is Personal Health Information (PHI)? Personal health information includes any identifying information about your health or health care history, such as your medical history, details of visits to your doctor, test results or your health number. What is the Personal Health Information Protection Act (PHIPA) 2004, and how does it relate to me? PHIPA is the Ontario law that protects the personal health information of individuals by regulating its use, collection and disclosure. PHIPA gives you the right to access or correct your Personal Health Information and to have related complaints reviewed by the Offi ce of the Information and Privacy Commissioner/Ontario. Why does The Ottawa Hospital collect my Personal Health Information? In order to provide you with the most appropriate health care, we need to accurately identify you as a patient and maintain a complete medical record. How is my Personal Health Information used and disclosed? • To provide you with care; • To monitor and evaluate the quality of care we provide you; • To administer and manage the operations of the hospital; • To do research, educate and collect statistics; • To comply with legal and regulatory requirements. 1 As well, we disclose your contact information to our Foundation, so that they may conduct fundraising to improve our healthcare facilities, services and programs.