Blockade of Phospholipid Scramblase 1 with Its N-Terminal Domain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Role and Regulation of Snon/Skil and PLSCR1 Located at 3Q26.2
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 9-18-2014 Role and Regulation of SnoN/SkiL and PLSCR1 Located at 3q26.2 and 3q23, Respectively, in Ovarian Cancer Pathophysiology Madhav Karthik Kodigepalli University of South Florida, [email protected] Follow this and additional works at: https://scholarcommons.usf.edu/etd Part of the Cell Biology Commons, Microbiology Commons, and the Molecular Biology Commons Scholar Commons Citation Kodigepalli, Madhav Karthik, "Role and Regulation of SnoN/SkiL and PLSCR1 Located at 3q26.2 and 3q23, Respectively, in Ovarian Cancer Pathophysiology" (2014). Graduate Theses and Dissertations. https://scholarcommons.usf.edu/etd/5426 This Dissertation is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. Role and Regulation of SnoN/SkiL and PLSCR1 Located at 3q26.2 and 3q23, Respectively, in Ovarian Cancer Pathophysiology by Madhav Karthik Kodigepalli A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Cell and Molecular Biology Department of Cell Biology, Microbiology and Molecular Biology College of Arts and Sciences University of South Florida Major Professor: Meera Nanjundan, Ph.D. Richard Pollenz, Ph.D. Patrick Bradshaw, Ph.D. Sandy Westerheide, Ph.D. Date of Approval: September 18, 2014 Keywords: Chemotherapeutics, phospholipid scramblase, toll-like receptor, interferon, dsDNA Copyright © 2014, Madhav Karthik Kodigepalli Dedication I dedicate this research at the lotus feet of Bhagwan Sri Sathya Sai Baba and all the Masters for I am what I am due to their divine grace. -

Molecular Signatures Differentiate Immune States in Type 1 Diabetes Families
Page 1 of 65 Diabetes Molecular signatures differentiate immune states in Type 1 diabetes families Yi-Guang Chen1, Susanne M. Cabrera1, Shuang Jia1, Mary L. Kaldunski1, Joanna Kramer1, Sami Cheong2, Rhonda Geoffrey1, Mark F. Roethle1, Jeffrey E. Woodliff3, Carla J. Greenbaum4, Xujing Wang5, and Martin J. Hessner1 1The Max McGee National Research Center for Juvenile Diabetes, Children's Research Institute of Children's Hospital of Wisconsin, and Department of Pediatrics at the Medical College of Wisconsin Milwaukee, WI 53226, USA. 2The Department of Mathematical Sciences, University of Wisconsin-Milwaukee, Milwaukee, WI 53211, USA. 3Flow Cytometry & Cell Separation Facility, Bindley Bioscience Center, Purdue University, West Lafayette, IN 47907, USA. 4Diabetes Research Program, Benaroya Research Institute, Seattle, WA, 98101, USA. 5Systems Biology Center, the National Heart, Lung, and Blood Institute, the National Institutes of Health, Bethesda, MD 20824, USA. Corresponding author: Martin J. Hessner, Ph.D., The Department of Pediatrics, The Medical College of Wisconsin, Milwaukee, WI 53226, USA Tel: 011-1-414-955-4496; Fax: 011-1-414-955-6663; E-mail: [email protected]. Running title: Innate Inflammation in T1D Families Word count: 3999 Number of Tables: 1 Number of Figures: 7 1 For Peer Review Only Diabetes Publish Ahead of Print, published online April 23, 2014 Diabetes Page 2 of 65 ABSTRACT Mechanisms associated with Type 1 diabetes (T1D) development remain incompletely defined. Employing a sensitive array-based bioassay where patient plasma is used to induce transcriptional responses in healthy leukocytes, we previously reported disease-specific, partially IL-1 dependent, signatures associated with pre and recent onset (RO) T1D relative to unrelated healthy controls (uHC). -

Anergic and Regulatory T Lymphocytes Functional and Molecular Comparison Of
Functional and Molecular Comparison of Anergic and Regulatory T Lymphocytes Birgit Knoechel, Jens Lohr, Shirley Zhu, Lisa Wong, Donglei Hu, Lara Ausubel and Abul K. Abbas This information is current as of September 29, 2021. J Immunol 2006; 176:6473-6483; ; doi: 10.4049/jimmunol.176.11.6473 http://www.jimmunol.org/content/176/11/6473 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2006/05/18/176.11.6473.DC1 Material References This article cites 54 articles, 28 of which you can access for free at: http://www.jimmunol.org/content/176/11/6473.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 29, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2006 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Functional and Molecular Comparison of Anergic and Regulatory T Lymphocytes1 Birgit Knoechel,2* Jens Lohr,2* Shirley Zhu,† Lisa Wong,† Donglei Hu,† Lara Ausubel,3* and Abul K. -

The Phospholipid Scramblases 1 and 4 Are Cellular Receptors for the Secretory Leukocyte Protease Inhibitor and Interact with CD4 at the Plasma Membrane
The Phospholipid Scramblases 1 and 4 Are Cellular Receptors for the Secretory Leukocyte Protease Inhibitor and Interact with CD4 at the Plasma Membrane Be´ne´dicte Py1,2., Ste´phane Basmaciogullari1,2.,Je´roˆ me Bouchet1,2, Marion Zarka1,2, Ivan C. Moura3,4, Marc Benhamou3,4, Renato C. Monteiro3,4, Hakim Hocini5, Ricardo Madrid1,2, Serge Benichou1,2* 1 Institut Cochin, Universite´ Paris-Descartes, CNRS, UMR 8104, Paris, France, 2 INSERM, U567, Paris, France, 3 INSERM U699, Paris, France, 4 Universite´ Paris 7-Denis Diderot, site Bichat, Paris, France, 5 INSERM U743, Paris, France Abstract Secretory leukocyte protease inhibitor (SLPI) is secreted by epithelial cells in all the mucosal fluids such as saliva, cervical mucus, as well in the seminal liquid. At the physiological concentrations found in saliva, SLPI has a specific antiviral activity against HIV-1 that is related to the perturbation of the virus entry process at a stage posterior to the interaction of the viral surface glycoprotein with the CD4 receptor. Here, we confirm that recombinant SLPI is able to inhibit HIV-1 infection of primary T lymphocytes, and show that SLPI can also inhibit the transfer of HIV-1 virions from primary monocyte-derived dendritic cells to autologous T lymphocytes. At the molecular level, we show that SLPI is a ligand for the phospholipid scramblase 1 (PLSCR1) and PLSCR4, membrane proteins that are involved in the regulation of the movements of phospholipids between the inner and outer leaflets of the plasma membrane. Interestingly, we reveal that PLSCR1 and PLSCR4 also interact directly with the CD4 receptor at the cell surface of T lymphocytes. -
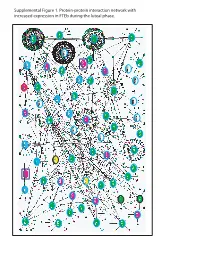
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

Discerning the Role of Foxa1 in Mammary Gland
DISCERNING THE ROLE OF FOXA1 IN MAMMARY GLAND DEVELOPMENT AND BREAST CANCER by GINA MARIE BERNARDO Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Dissertation Adviser: Dr. Ruth A. Keri Department of Pharmacology CASE WESTERN RESERVE UNIVERSITY January, 2012 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of Gina M. Bernardo ______________________________________________________ Ph.D. candidate for the ________________________________degree *. Monica Montano, Ph.D. (signed)_______________________________________________ (chair of the committee) Richard Hanson, Ph.D. ________________________________________________ Mark Jackson, Ph.D. ________________________________________________ Noa Noy, Ph.D. ________________________________________________ Ruth Keri, Ph.D. ________________________________________________ ________________________________________________ July 29, 2011 (date) _______________________ *We also certify that written approval has been obtained for any proprietary material contained therein. DEDICATION To my parents, I will forever be indebted. iii TABLE OF CONTENTS Signature Page ii Dedication iii Table of Contents iv List of Tables vii List of Figures ix Acknowledgements xi List of Abbreviations xiii Abstract 1 Chapter 1 Introduction 3 1.1 The FOXA family of transcription factors 3 1.2 The nuclear receptor superfamily 6 1.2.1 The androgen receptor 1.2.2 The estrogen receptor 1.3 FOXA1 in development 13 1.3.1 Pancreas and Kidney -

Phospholipid Scramblase 1 Potentiates the Antiviral Activity of Interferon
Cleveland State University EngagedScholarship@CSU Chemistry Faculty Publications Chemistry Department 9-1-2004 Phospholipid Scramblase 1 Potentiates The Antiviral Activity of Interferon Beihua Dong Lerner Research Institute Quansheng Zhou The Scripps Research Institute Ji Zhao The Scripps Research Institute Aimin Zhou Cleveland State University, [email protected] Ronald N. Harty University of Pennsylvania See next page for additional authors Follow this and additional works at: https://engagedscholarship.csuohio.edu/scichem_facpub Part of the Chemistry Commons How does access to this work benefit ou?y Let us know! Recommended Citation Dong, Beihua; Zhou, Quansheng; Zhao, Ji; Zhou, Aimin; Harty, Ronald N.; Bose, Santanu; Banerjee, Amiya; Slee, Roger; Guenther, Jeanna; Williams, Bryan R.G.; Wiedmer, Therese; Sims, Peter J.; and Silverman, Robert H., "Phospholipid Scramblase 1 Potentiates The Antiviral Activity of Interferon" (2004). Chemistry Faculty Publications. 403. https://engagedscholarship.csuohio.edu/scichem_facpub/403 This Article is brought to you for free and open access by the Chemistry Department at EngagedScholarship@CSU. It has been accepted for inclusion in Chemistry Faculty Publications by an authorized administrator of EngagedScholarship@CSU. For more information, please contact [email protected]. Authors Beihua Dong, Quansheng Zhou, Ji Zhao, Aimin Zhou, Ronald N. Harty, Santanu Bose, Amiya Banerjee, Roger Slee, Jeanna Guenther, Bryan R.G. Williams, Therese Wiedmer, Peter J. Sims, and Robert H. Silverman This article is available at EngagedScholarship@CSU: https://engagedscholarship.csuohio.edu/scichem_facpub/403 8983 Phospholipid Scramblase 1 Potentiates the Antiviral Activity of Interferon Beihua Dong, Quansheng Zhou, Ji Zhao, Aimin Zhou, Ronald N. Harty, Santanu Bose, Amiya Banerjee, Roger Slee, Jeanna Guenther, Bryan R. -

Phenotype Informatics
Freie Universit¨atBerlin Department of Mathematics and Computer Science Phenotype informatics: Network approaches towards understanding the diseasome Sebastian Kohler¨ Submitted on: 12th September 2012 Dissertation zur Erlangung des Grades eines Doktors der Naturwissenschaften (Dr. rer. nat.) am Fachbereich Mathematik und Informatik der Freien Universitat¨ Berlin ii 1. Gutachter Prof. Dr. Martin Vingron 2. Gutachter: Prof. Dr. Peter N. Robinson 3. Gutachter: Christopher J. Mungall, Ph.D. Tag der Disputation: 16.05.2013 Preface This thesis presents research work on novel computational approaches to investigate and characterise the association between genes and pheno- typic abnormalities. It demonstrates methods for organisation, integra- tion, and mining of phenotype data in the field of genetics, with special application to human genetics. Here I will describe the parts of this the- sis that have been published in peer-reviewed journals. Often in modern science different people from different institutions contribute to research projects. The same is true for this thesis, and thus I will itemise who was responsible for specific sub-projects. In chapter 2, a new method for associating genes to phenotypes by means of protein-protein-interaction networks is described. I present a strategy to organise disease data and show how this can be used to link diseases to the corresponding genes. I show that global network distance measure in interaction networks of proteins is well suited for investigat- ing genotype-phenotype associations. This work has been published in 2008 in the American Journal of Human Genetics. My contribution here was to plan the project, implement the software, and finally test and evaluate the method on human genetics data; the implementation part was done in close collaboration with Sebastian Bauer. -

Autocrine IFN Signaling Inducing Profibrotic Fibroblast Responses By
Downloaded from http://www.jimmunol.org/ by guest on September 23, 2021 Inducing is online at: average * The Journal of Immunology , 11 of which you can access for free at: 2013; 191:2956-2966; Prepublished online 16 from submission to initial decision 4 weeks from acceptance to publication August 2013; doi: 10.4049/jimmunol.1300376 http://www.jimmunol.org/content/191/6/2956 A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Autocrine IFN Signaling Feng Fang, Kohtaro Ooka, Xiaoyong Sun, Ruchi Shah, Swati Bhattacharyya, Jun Wei and John Varga J Immunol cites 49 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2013/08/20/jimmunol.130037 6.DC1 This article http://www.jimmunol.org/content/191/6/2956.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 23, 2021. The Journal of Immunology A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Inducing Autocrine IFN Signaling Feng Fang,* Kohtaro Ooka,* Xiaoyong Sun,† Ruchi Shah,* Swati Bhattacharyya,* Jun Wei,* and John Varga* Activation of TLR3 by exogenous microbial ligands or endogenous injury-associated ligands leads to production of type I IFN. -

An En Masse Phenotype and Function Prediction System for Mus Musculus
Open Access Research2008TaetVolume al.s¸an 9, Suppl 1, Article S8 An en masse phenotype and function prediction system for Mus musculus Murat Taşan¤*, Weidong Tian¤*, David P Hill†, Francis D Gibbons‡, Judith A Blake† and Frederick P Roth* Addresses: *Department of Biological Chemistry and Molecular Pharmacology, Harvard Medical School, Longwood Avenue, Boston, Massachusetts 02115, USA. †Computational Biology and Bioinformatics, The Jackson Laboratory, Main Street, Bar Harbor, Maine 04609, USA. ‡Merrimack Pharmaceuticals, Kendall Square, Cambridge, Massachusetts 02139, USA. ¤ These authors contributed equally to this work. Correspondence: Frederick P Roth. Email: [email protected] Published: 27 June 2008 Genome Biology 2008, 9:S8 The electronic version of this article is the complete one and can be found online at http://genomebiology.com/2008/9/S1/S8 © 2008 Tas¸an et al; licensee BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Individual researchers are struggling to keep up with the accelerating emergence of high-throughput biological data, and to extract information that relates to their specific questions. Integration of accumulated evidence should permit researchers to form fewer - and more accurate - hypotheses for further study through experimentation. Results: Here a method previously used to predict Gene Ontology (GO) terms for Saccharomyces cerevisiae (Tian et al.: Combining guilt-by-association and guilt-by-profiling to predict Saccharomyces cerevisiae gene function. Genome Biol 2008, 9(Suppl 1):S7) is applied to predict GO terms and phenotypes for 21,603 Mus musculus genes, using a diverse collection of integrated data sources (including expression, interaction, and sequence-based data). -

Epitope Stealing As Mechanism of Dominant Protection
Page 1 of 49 Diabetes EPITOPE STEALING AS MECHANISM OF DOMINANT PROTECTION BY HLA-DQ6 IN TYPE 1 DIABETES Menno van Lummel1, David T. P. Buis1, Cherish Ringeling1, Arnoud H. de Ru1, Jos Pool1, George K. Papadopoulos2, Peter A. van Veelen1, Helena Reijonen3, Jan W. Drijfhout1 and Bart O. Roep1, 3 1Department of Immunohematology and Blood Transfusion, Leiden University Medical Center, the Netherlands, The Netherlands; 2Laboratory of Biochemistry and Biophysics, Faculty of Agricultural Technology, Epirus Institute of Technology, Arta, Greece 3Department of Diabetes Immunology, Diabetes & Metabolism Research Institute at the Beckman Research Institute, City of Hope, Duarte, USA; *Running title: islet epitope stealing by protective HLA-DQ6 Corresponding author: Prof. Bart O Roep, PhD Department of Immunohematology and Blood Transfusion, LUMC, E3-Q, PO Box 9600, 2300 RC Leiden, the Netherlands Tel: +31.71.5266673; Fax: +31.71.5266801; Email: [email protected] Keywords: type 1 diabetes, HLA-DQ6, HLA-DQ8, protection, immunotherapy 1 Diabetes Publish Ahead of Print, published online January 9, 2019 Diabetes Page 2 of 49 ABSTRACT The heterozygous DQ2/8 (DQA1*05:01-DQB1*02:01/DQA1*03:01-DQB1*03:02) genotype confers the highest risk in T1D, whereas the DQ6/8 (DQA1*02:01-DQB1*06:02/ DQA1*03:01-DQB1*03:02) genotype is protective. The mechanism of dominant protection by DQ6 (DQB1*06:02) is unknown. We tested the hypothesis that DQ6 interferes with peptide- binding to DQ8 by competition for islet epitope (‘epitope stealing’) by analysis of the islet ligandome presented by HLA-DQ6/8 and -DQ8/8 on dendritic cells pulsed with islet autoantigens preproinsulin (PPI), GAD65 and IA2, followed by competition assays employing a newly established ‘epitope stealing’ HLA/peptide binding assay.