Prader-Willi Syndrome : Genotype and Phenotype at Adult Age
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WELLBUTRIN SR Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION psychosis, hallucinations, paranoia, delusions, homicidal ideation, These highlights do not include all the information needed to use aggression, hostility, agitation, anxiety, and panic, as well as suicidal WELLBUTRIN SR safely and effectively. See full prescribing ideation, suicide attempt, and completed suicide. Observe patients information for WELLBUTRIN SR. attempting to quit smoking with bupropion for the occurrence of such symptoms and instruct them to discontinue bupropion and contact a WELLBUTRIN SR (bupropion hydrochloride) sustained-release tablets, healthcare provider if they experience such adverse events. (5.2) for oral use • Initial U.S. Approval: 1985 Seizure risk: The risk is dose-related. Can minimize risk by gradually increasing the dose and limiting daily dose to 400 mg. Discontinue if WARNING: SUICIDAL THOUGHTS AND BEHAVIORS seizure occurs. (4, 5.3, 7.3) See full prescribing information for complete boxed warning. • Hypertension: WELLBUTRIN SR can increase blood pressure. Monitor blood pressure before initiating treatment and periodically during • Increased risk of suicidal thinking and behavior in children, treatment. (5.4) adolescents and young adults taking antidepressants. (5.1) • Activation of mania/hypomania: Screen patients for bipolar disorder and • Monitor for worsening and emergence of suicidal thoughts and monitor for these symptoms. (5.5) behaviors. (5.1) • Psychosis and other neuropsychiatric reactions: Instruct patients to contact a healthcare professional if such reactions occur. (5.6) --------------------------- INDICATIONS AND USAGE ---------------------------- • Angle-closure glaucoma: Angle-closure glaucoma has occurred in WELLBUTRIN SR is an aminoketone antidepressant, indicated for the patients with untreated anatomically narrow angles treated with treatment of major depressive disorder (MDD). (1) antidepressants. -

Clarifying the Ghrelin System's Ability to Regulate Feeding Behaviours
International Journal of Molecular Sciences Review Clarifying the Ghrelin System’s Ability to Regulate Feeding Behaviours Despite Enigmatic Spatial Separation of the GHSR and Its Endogenous Ligand Alexander Edwards and Alfonso Abizaid * Department of Neuroscience, Carleton University, 1125 Colonel By Drive, Ottawa, ON K1S 5B6, Canada; [email protected] * Correspondence: [email protected]; Tel.: +1-613-520-2600 (ext. 1544) Academic Editor: Suzanne L. Dickson Received: 27 February 2017; Accepted: 11 April 2017; Published: 19 April 2017 Abstract: Ghrelin is a hormone predominantly produced in and secreted from the stomach. Ghrelin is involved in many physiological processes including feeding, the stress response, and in modulating learning, memory and motivational processes. Ghrelin does this by binding to its receptor, the growth hormone secretagogue receptor (GHSR), a receptor found in relatively high concentrations in hypothalamic and mesolimbic brain regions. While the feeding and metabolic effects of ghrelin can be explained by the effects of this hormone on regions of the brain that have a more permeable blood brain barrier (BBB), ghrelin produced within the periphery demonstrates a limited ability to reach extrahypothalamic regions where GHSRs are expressed. Therefore, one of the most pressing unanswered questions plaguing ghrelin research is how GHSRs, distributed in brain regions protected by the BBB, are activated despite ghrelin’s predominant peripheral production and poor ability to transverse the BBB. This manuscript will describe how peripheral ghrelin activates central GHSRs to encourage feeding, and how central ghrelin synthesis and ghrelin independent activation of GHSRs may also contribute to the modulation of feeding behaviours. Keywords: feeding; ghrelin; GHSR; blood brain barrier; vagal afferents; circumventricular organs; central ghrelin synthesis; GHSR heterodimerization; GHSR constitutive activity 1. -

WHO Drug Information Vol. 12, No. 3, 1998
WHO DRUG INFORMATION VOLUME 12 NUMBER 3 • 1998 RECOMMENDED INN LIST 40 INTERNATIONAL NONPROPRIETARY NAMES FOR PHARMACEUTICAL SUBSTANCES WORLD HEALTH ORGANIZATION • GENEVA Volume 12, Number 3, 1998 World Health Organization, Geneva WHO Drug Information Contents Seratrodast and hepatic dysfunction 146 Meloxicam safety similar to other NSAIDs 147 Proxibarbal withdrawn from the market 147 General Policy Issues Cholestin an unapproved drug 147 Vigabatrin and visual defects 147 Starting materials for pharmaceutical products: safety concerns 129 Glycerol contaminated with diethylene glycol 129 ATC/DDD Classification (final) 148 Pharmaceutical excipients: certificates of analysis and vendor qualification 130 ATC/DDD Classification Quality assurance and supply of starting (temporary) 150 materials 132 Implementation of vendor certification 134 Control and safe trade in starting materials Essential Drugs for pharmaceuticals: recommendations 134 WHO Model Formulary: Immunosuppressives, antineoplastics and drugs used in palliative care Reports on Individual Drugs Immunosuppresive drugs 153 Tamoxifen in the prevention and treatment Azathioprine 153 of breast cancer 136 Ciclosporin 154 Selective serotonin re-uptake inhibitors and Cytotoxic drugs 154 withdrawal reactions 136 Asparaginase 157 Triclabendazole and fascioliasis 138 Bleomycin 157 Calcium folinate 157 Chlormethine 158 Current Topics Cisplatin 158 Reverse transcriptase activity in vaccines 140 Cyclophosphamide 158 Consumer protection and herbal remedies 141 Cytarabine 159 Indiscriminate antibiotic -

FSI-D-16-00226R1 Title
Elsevier Editorial System(tm) for Forensic Science International Manuscript Draft Manuscript Number: FSI-D-16-00226R1 Title: An overview of Emerging and New Psychoactive Substances in the United Kingdom Article Type: Review Article Keywords: New Psychoactive Substances Psychostimulants Lefetamine Hallucinogens LSD Derivatives Benzodiazepines Corresponding Author: Prof. Simon Gibbons, Corresponding Author's Institution: UCL School of Pharmacy First Author: Simon Gibbons Order of Authors: Simon Gibbons; Shruti Beharry Abstract: The purpose of this review is to identify emerging or new psychoactive substances (NPS) by undertaking an online survey of the UK NPS market and to gather any data from online drug fora and published literature. Drugs from four main classes of NPS were identified: psychostimulants, dissociative anaesthetics, hallucinogens (phenylalkylamine-based and lysergamide-based materials) and finally benzodiazepines. For inclusion in the review the 'user reviews' on drugs fora were selected based on whether or not the particular NPS of interest was used alone or in combination. NPS that were use alone were considered. Each of the classes contained drugs that are modelled on existing illegal materials and are now covered by the UK New Psychoactive Substances Bill in 2016. Suggested Reviewers: Title Page (with authors and addresses) An overview of Emerging and New Psychoactive Substances in the United Kingdom Shruti Beharry and Simon Gibbons1 Research Department of Pharmaceutical and Biological Chemistry UCL School of Pharmacy -
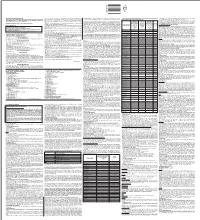
Full Prescribing Information Warning: Suicidal Thoughts
tablets (SR) BUPROPION hydrochloride extended-release HIGHLIGHTS OF PRESCRIBING INFORMATION anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe hydrochloride extended-release tablets (SR) was reported. However, the symptoms persisted in some Table 3. Adverse Reactions Reported by at Least 1% of Subjects on Active Treatment and at a tablets (SR) may be necessary when coadministered with ritonavir, lopinavir, or efavirenz [see Clinical These highlights do not include all the information needed to use bupropion hydrochloride patients attempting to quit smoking with Bupropion hydrochloride extended-release tablets, USP cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve. Greater Frequency than Placebo in the Comparator Trial Pharmacology (12.3)] but should not exceed the maximum recommended dose. extended-release tablets (SR) safely and effectively. See full prescribing information for (SR) for the occurrence of such symptoms and instruct them to discontinue Bupropion hydrochloride Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs extended-release tablets, USP (SR) and contact a healthcare provider if they experience such adverse The neuropsychiatric safety of Bupropion hydrochloride extended-release tablets (SR) was evaluated in Bupropion Bupropion may induce the metabolism of bupropion and may decrease bupropion exposure [see Clinical bupropion hydrochloride extended-release tablets (SR). Nicotine events. (5.2) a randomized, double-blind, active-and placebo-controlled study that included patients without a history Hydrochloride Hydrochloride Pharmacology (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary Transdermal BUPROPION hydrochloride extended-release tablets (SR), for oral use • Seizure risk: The risk is dose-related. -

Cross-Sectional Study of the Dispensation of Synthetic Anorectic Drugs in Community Pharmacies in the City of Cruz Alta – State of Rio Grande Do Sul
Brazilian Journal of Pharmaceutical Sciences vol. 50, n. 4, oct./dec., 2014 Article http://dx.doi.org/10.1590/S1984-82502014000400008 Cross-sectional study of the dispensation of synthetic anorectic drugs in community pharmacies in the city of Cruz Alta – State of Rio Grande do Sul Marcieli Maria Navarini1, Viviane Cecilia Kessler Nunes Deuschle2,*, Regis Augusto Norbert Deuschle3 1Faculty of Pharmacy, University of Cruz Alta, Rio Grande do Sul, Brazil,2,3Postgraduate Program in Pharmaceutical Sciences, Federal University of Santa Maria, Brazil Obesity is defined as the excess adipose tissue in the body. Drugs responsible for inhibiting the appetite are called anorectics or appetite suppressants. Sibutramine, fenproporex and amfepramone belongs to this class, and are capable of causing physical or psychological dependence. The aim of this study was to evaluate the frequency of prescriptions for appetite suppressants in community pharmacies at Cruz Alta, State of Rio Grande do Sul, Brazil. The sales of fenproporex, amfepramone and sibutramine in the months of September, October and November 2010 and April, May and June 2011 were compared. It was observed that the most commonly dispensed anorectic in the three community pharmacies analyzed was sibutramine. In the months of September, October and November 2010, consumption was higher, with sibutramine achieving 40.3% of overall sales, amfepramone 21% and, finally, fenproporex, 7.9%. The consumption of appetite suppressants was more prevalent in females, who represented 82% of total. The results suggested the existence of high consumption of anorectics, possibly related to the current concern with aesthetic standards, which emphasizes the importance of strict control over the marketing of these substances. -

PRODUCT MONOGRAPH Pr WELLBUTRIN XL Bupropion
PRODUCT MONOGRAPH Pr WELLBUTRIN XL Bupropion Hydrochloride Extended-Release Tablets, USP 150 mg and 300 mg Antidepressant Name: Date of Revision: Valeant Canada LP March 20, 2017 Address: 2150 St-Elzear Blvd. West Laval, QC, H7L 4A8 Control Number: 200959 Table of Contents Page PART I: HEALTH PROFESSIONAL INFORMATION .............................................................. 2 SUMMARY PRODUCT INFORMATION ................................................................................. 2 INDICATIONS AND CLINICAL USE ....................................................................................... 2 CONTRAINDICATIONS ............................................................................................................ 3 WARNINGS AND PRECAUTIONS ........................................................................................... 3 ADVERSE REACTIONS ............................................................................................................. 9 DRUG INTERACTIONS ........................................................................................................... 19 DOSAGE AND ADMINISTRATION ....................................................................................... 22 OVERDOSAGE ......................................................................................................................... 24 ACTION AND CLINICAL PHARMACOLOGY ..................................................................... 25 STORAGE AND STABILITY .................................................................................................. -

The Role of Mesolimbic Reward Neurocircuitry in Prevention and Rescue of the Activity-Based Anorexia (ABA) Phenotype in Rats
Neuropsychopharmacology (2017) 42, 2292–2300 © 2017 American College of Neuropsychopharmacology. All rights reserved 0893-133X/17 www.neuropsychopharmacology.org The Role of Mesolimbic Reward Neurocircuitry in Prevention and Rescue of the Activity-Based Anorexia (ABA) Phenotype in Rats 1 1 ,1 Claire J Foldi , Laura K Milton and Brian J Oldfield* 1 Department of Physiology, Monash University, Clayton, VIC, Australia Patients suffering from anorexia nervosa (AN) become anhedonic; unable or unwilling to derive normal pleasures and avoid rewarding outcomes, most profoundly in food intake. The activity-based anorexia (ABA) model recapitulates many of the characteristics of the human condition, including anhedonia, and allows investigation of the underlying neurobiology of AN. The potential for increased neuronal activity in reward/hedonic circuits to prevent and rescue weight loss is investigated in this model. The mesolimbic pathway extending from the ventral tegmental area (VTA) to the nucleus accumbens (NAc) was activated using a dual viral strategy, involving retrograde transport of Cre (CAV-2-Cre) to the VTA and coincident injection of DREADD receptors (AAV-hSyn-DIO-hM3D(Gq)-mCherry). Systemic clozapine-n-oxide (CNO; 0.3 mg/kg) successfully recruited a large proportion of the VTA-NAc dopaminergic projections, with activity evidenced by colocalization with elevated levels of Fos protein. The effects of reward circuit activation on energy balance and predicted survival was investigated in female Sprague-Dawley rats, where free access to running wheels was paired with time-limited (90 min) access to food, a paradigm (ABA) which will cause anorexia and death if unchecked. Excitation of the reward pathway substantially increased food intake and food anticipatory activity (FAA) to prevent ABA-associated weight loss, while overall locomotor activity was unchanged. -

5-Hydroxy-L-Tryptophan Suppresses Food Intake in Food-Deprived and Stressed Rats
Pharmacology, Biochemistry and Behavior 77 (2004) 137–143 www.elsevier.com/locate/pharmbiochembeh 5-Hydroxy-L-tryptophan suppresses food intake in food-deprived and stressed rats Ahmed Amera, Jeff Breub, Janine McDermottb, Richard J. Wurtmanb,c, Timothy J. Mahera,c,* aDepartment of Pharmaceutical Sciences, Massachusetts College of Pharmacy and Health Sciences, Boston, MA, USA bGeneral Clinical Research Center, Massachusetts Institute of Technology, Cambridge, MA, USA cDepartment of Brain and Cognitive Sciences, Massachusetts Institute of Technology, Cambridge, MA, USA Received 22 January 2003; received in revised form 15 June 2003; accepted 10 October 2003 Abstract Giving L-tryptophan, serotonin’s circulating precursor, or a serotonin-releasing drug can decrease food intake and body weight. Giving 5- hydroxy-L-tryptophan (5-HTP), serotonin’s immediate intracellular precursor, has been thought to be ineffective in enhancing brain serotonin synthesis unless it is coadministered with a dopa decarboxylase inhibitor to protect 5-HTP from destruction outside the brain. We have examined the effect of 5-HTP on food consumption and tissue 5-HTP levels among rats subjected to two different hyperphagic stimuli, food deprivation and a standardized stress (tail pinch), and on plasma 5-HTP levels in humans. In rats, 5-HTP (3–200 mg/kg ip) suppressed food intake in a dose-dependent manner in both models, but was at least eight times more effective in our stress–hyperphagia model. (Differences in the two procedures might have contributed to the observed differences in potencies.) This suppression was blocked by coadministration of 2 another large neutral amino acid (LNAA), L-valine. Brain 5-HTP levels correlated significantly with peak plasma 5-HTP (r =.69) or 5-HTP/ LNAA (r2=.81) levels. -

Non-Pharmacological Factors That Determine Drug Use and Addiction Aldo Badiani, Klaus Miczek, Christian Müller, Serge Ahmed H
Non-pharmacological factors that determine drug use and addiction Aldo Badiani, Klaus Miczek, Christian Müller, Serge Ahmed H. To cite this version: Aldo Badiani, Klaus Miczek, Christian Müller, Serge Ahmed H.. Non-pharmacological factors that determine drug use and addiction. Neuroscience & Biobehavioral Reviews, Oxford: Elsevier Ltd., 2020, 110, pp.3-27. 10.1016/j.neubiorev.2018.08.015. hal-03005497 HAL Id: hal-03005497 https://hal.archives-ouvertes.fr/hal-03005497 Submitted on 25 Nov 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Special Issue – IBNS Non-pharmacological factors that determine drug use and addiction Serge Ahmed 1*, Aldo Badiani 2,3*, Klaus A. Miczek 4,5*, Christian P. Müller 6* 1 Université de Bordeaux, Institut des Maladies Neurodégénératives, UMR 5293, 146 rue Léo-Saignat, F-33000 Bordeaux, France; CNRS, Institut des Maladies Neurodégénératives, UMR 5293, 146 rue Léo-Saignat, F-33000 Bordeaux, France. 2 Department of Physiology and Pharmacology, Sapienza University of Rome, Piazzale Aldo Moro 5, 00185 Rome, Italy. 3 Sussex Addiction Research and Intervention Centre (SARIC), School of Psychology, University of Sussex, BN1 9RH, Brighton, UK. 4 Psychology Department, Tufts University, Bacon Hall, 530 Boston Avenue, Medford, MA, 02155, USA. -

A Clinical Perspective on the Therapeutic Role of Venlafaxine, A
Panic and depression: not all SSRI's are the same 2538 serotonin-norepinephrine reuptake inhibitor, will examine venlafax ine's usefulnessin a broadrangeof depressedpatientsand character Smithkline, Beecham ize features that distinguish venlafaxine from other antidepressants. Double-blind, parallel-group studies are planned to compare ven lafaxinewith other antidepressants including fluoxet ine, paroxetine, ST5. Panic and depression: not all SSRl's sertraline, citalopram, and moclobemide, A series of studies is in are the same progress to provide clinical confirmation for in vitro findings which suggest that venlafaxine has a low potential for producing drug Chairmen: J Ballanger, J Mendlewicz interactions, because it does not significantly inhibit any of the majorcytochrome P450 enzymes. Specificstudiesare in progressor planned to further elucidate venlafaxine's mechanismof action and onset of action. A once daily formulation of venlafaxine is under Abstractsnot received, development to provide additional simplicity of dosage administra tion. Although depression will continue to be the major focus for venlafaxine clinical investigations, there is growing interest among researchers and clinicians in a variety of other clinical applications for antidepressants. Possible new applications include generalized Pfizer Limited anxiety disorder. panic disorder. obsessive-compulsive disorder, so cial phobia, neuropathic pain syndromes. premenstrual dysphoric ST6. The role of 5HT central synaptic disorder, obesity. Alzheimer's disease.and attention deficitdisorder. transmission in the regulation of the extra pyramidal system A CLINICALPERSPECTIVEONTHE THERAPEUTIC ROLEOF VENLAFAXINE. ASNRI,IN DEPRESSION Chairman: T Dinan E. Salinas. Director, Clinical Science CRDEurope. Wyeth-Lederle CRD.80Avedu President Wilson. 92031 Paris la Defense Cedex; France DOPAMINE ANDTHE USEOF SSRls FOR CONDITIONS Venlafaxine, a new serotonin-norepinephrine reuptake inhibitor OTHERTHANDEPRESSION (SNRI). -

Wellbutrin (Bupropion Hydrochloride) Tablets Label
PRESCRIBING INFORMATION ® WELLBUTRIN (bupropion hydrochloride) Tablets WARNING Suicidality and Antidepressant Drugs Use in Treating Psychiatric Disorders: Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of WELLBUTRIN or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. WELLBUTRIN is not approved for use in pediatric patients. (See WARNINGS: Clinical Worsening and Suicide Risk in Treating Psychiatric Disorders, PRECAUTIONS: Information for Patients, and PRECAUTIONS: Pediatric Use.) Use in Smoking Cessation Treatment: WELLBUTRIN®, WELLBUTRIN SR®, and WELLBUTRIN XL® are not approved for smoking cessation treatment, but bupropion under the name ZYBAN® is approved for this use. Serious neuropsychiatric events, including but not limited to depression, suicidal ideation, suicide attempt, and completed suicide have been reported in patients taking bupropion for smoking cessation. Some cases may have been complicated by the symptoms of nicotine withdrawal in patients who stopped smoking.