The Role of Mesolimbic Reward Neurocircuitry in Prevention and Rescue of the Activity-Based Anorexia (ABA) Phenotype in Rats
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

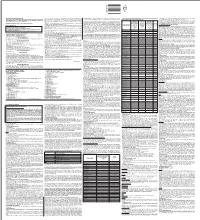
WELLBUTRIN SR Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION psychosis, hallucinations, paranoia, delusions, homicidal ideation, These highlights do not include all the information needed to use aggression, hostility, agitation, anxiety, and panic, as well as suicidal WELLBUTRIN SR safely and effectively. See full prescribing ideation, suicide attempt, and completed suicide. Observe patients information for WELLBUTRIN SR. attempting to quit smoking with bupropion for the occurrence of such symptoms and instruct them to discontinue bupropion and contact a WELLBUTRIN SR (bupropion hydrochloride) sustained-release tablets, healthcare provider if they experience such adverse events. (5.2) for oral use • Initial U.S. Approval: 1985 Seizure risk: The risk is dose-related. Can minimize risk by gradually increasing the dose and limiting daily dose to 400 mg. Discontinue if WARNING: SUICIDAL THOUGHTS AND BEHAVIORS seizure occurs. (4, 5.3, 7.3) See full prescribing information for complete boxed warning. • Hypertension: WELLBUTRIN SR can increase blood pressure. Monitor blood pressure before initiating treatment and periodically during • Increased risk of suicidal thinking and behavior in children, treatment. (5.4) adolescents and young adults taking antidepressants. (5.1) • Activation of mania/hypomania: Screen patients for bipolar disorder and • Monitor for worsening and emergence of suicidal thoughts and monitor for these symptoms. (5.5) behaviors. (5.1) • Psychosis and other neuropsychiatric reactions: Instruct patients to contact a healthcare professional if such reactions occur. (5.6) --------------------------- INDICATIONS AND USAGE ---------------------------- • Angle-closure glaucoma: Angle-closure glaucoma has occurred in WELLBUTRIN SR is an aminoketone antidepressant, indicated for the patients with untreated anatomically narrow angles treated with treatment of major depressive disorder (MDD). (1) antidepressants. -

Clarifying the Ghrelin System's Ability to Regulate Feeding Behaviours
International Journal of Molecular Sciences Review Clarifying the Ghrelin System’s Ability to Regulate Feeding Behaviours Despite Enigmatic Spatial Separation of the GHSR and Its Endogenous Ligand Alexander Edwards and Alfonso Abizaid * Department of Neuroscience, Carleton University, 1125 Colonel By Drive, Ottawa, ON K1S 5B6, Canada; [email protected] * Correspondence: [email protected]; Tel.: +1-613-520-2600 (ext. 1544) Academic Editor: Suzanne L. Dickson Received: 27 February 2017; Accepted: 11 April 2017; Published: 19 April 2017 Abstract: Ghrelin is a hormone predominantly produced in and secreted from the stomach. Ghrelin is involved in many physiological processes including feeding, the stress response, and in modulating learning, memory and motivational processes. Ghrelin does this by binding to its receptor, the growth hormone secretagogue receptor (GHSR), a receptor found in relatively high concentrations in hypothalamic and mesolimbic brain regions. While the feeding and metabolic effects of ghrelin can be explained by the effects of this hormone on regions of the brain that have a more permeable blood brain barrier (BBB), ghrelin produced within the periphery demonstrates a limited ability to reach extrahypothalamic regions where GHSRs are expressed. Therefore, one of the most pressing unanswered questions plaguing ghrelin research is how GHSRs, distributed in brain regions protected by the BBB, are activated despite ghrelin’s predominant peripheral production and poor ability to transverse the BBB. This manuscript will describe how peripheral ghrelin activates central GHSRs to encourage feeding, and how central ghrelin synthesis and ghrelin independent activation of GHSRs may also contribute to the modulation of feeding behaviours. Keywords: feeding; ghrelin; GHSR; blood brain barrier; vagal afferents; circumventricular organs; central ghrelin synthesis; GHSR heterodimerization; GHSR constitutive activity 1. -

Addiction, Opioids, and Beyond
Addiction, Opioids and Beyond Chronic Pain Mental Illness Substance Dep Medical Illness Genetics/Env Objectives Understanding Definitions in Substance Dependency and Addiction. Review of Basic Epidemiology in Opioids Understanding Basic Addiction Physiology and how it relates to Schizophrenia Knowledge the General Overview of SUD Treatment Knowledge of non-pharmacological treatments of SUD. Understanding of Prescription Opioids, Side Effects and Dangers Understanding Prescription Opioids in the setting of Chronic Pain Understand MAT for Opioids (Tip43) with Naltrexone, Methadone and Buprenorphine Naloxone WHAT DOES ADDICTION MEAN? In 2016 11.5 million people 12 years and older misused opioid pain medications 1.8 million had substance use disorder involving prescription pain medications Between 2000 to 2015, more then 500,000 person died from opioid overdoses Opioid and 2012 clinicians wrote 259 million prescription for opioids Overdose 2.5 million people with Opioid Addiction (JAMA) US deaths from drug overdoses hit record high in 2014, propelled by abuse of prescription painkillers and heroin. (CDC) Heroin related deaths tripled since 2010. Only 2.2% of US Physician have waiver to prescribe Buprenorphine (JAMA) Statistically, nonmedical use of drugs from individuals obtained a majority of their drugs from friends and relatives, however 80% of those “friends and family” obtained from ONE DOCTOR. Addiction Poorly Understood • Regard Addiction as a moral problem • Fail to adequately screen • 1% of medical school curriculum • Believe interventions are ineffective JAMA,2003,290, 1299 Defining the Word "Addiction" The American Society of Addiction Medicine (ASAM), American Pain Society (APS), and American Academy of Pain Medicine (AAPM) define addiction as a primary, chronic, neurobiological disease with genetic, psychosocial, and environmental factors influencing its development and manifestations characterized by one or more of the behaviors listed above (ASAM, 2001). -

WHO Drug Information Vol. 12, No. 3, 1998
WHO DRUG INFORMATION VOLUME 12 NUMBER 3 • 1998 RECOMMENDED INN LIST 40 INTERNATIONAL NONPROPRIETARY NAMES FOR PHARMACEUTICAL SUBSTANCES WORLD HEALTH ORGANIZATION • GENEVA Volume 12, Number 3, 1998 World Health Organization, Geneva WHO Drug Information Contents Seratrodast and hepatic dysfunction 146 Meloxicam safety similar to other NSAIDs 147 Proxibarbal withdrawn from the market 147 General Policy Issues Cholestin an unapproved drug 147 Vigabatrin and visual defects 147 Starting materials for pharmaceutical products: safety concerns 129 Glycerol contaminated with diethylene glycol 129 ATC/DDD Classification (final) 148 Pharmaceutical excipients: certificates of analysis and vendor qualification 130 ATC/DDD Classification Quality assurance and supply of starting (temporary) 150 materials 132 Implementation of vendor certification 134 Control and safe trade in starting materials Essential Drugs for pharmaceuticals: recommendations 134 WHO Model Formulary: Immunosuppressives, antineoplastics and drugs used in palliative care Reports on Individual Drugs Immunosuppresive drugs 153 Tamoxifen in the prevention and treatment Azathioprine 153 of breast cancer 136 Ciclosporin 154 Selective serotonin re-uptake inhibitors and Cytotoxic drugs 154 withdrawal reactions 136 Asparaginase 157 Triclabendazole and fascioliasis 138 Bleomycin 157 Calcium folinate 157 Chlormethine 158 Current Topics Cisplatin 158 Reverse transcriptase activity in vaccines 140 Cyclophosphamide 158 Consumer protection and herbal remedies 141 Cytarabine 159 Indiscriminate antibiotic -

FSI-D-16-00226R1 Title
Elsevier Editorial System(tm) for Forensic Science International Manuscript Draft Manuscript Number: FSI-D-16-00226R1 Title: An overview of Emerging and New Psychoactive Substances in the United Kingdom Article Type: Review Article Keywords: New Psychoactive Substances Psychostimulants Lefetamine Hallucinogens LSD Derivatives Benzodiazepines Corresponding Author: Prof. Simon Gibbons, Corresponding Author's Institution: UCL School of Pharmacy First Author: Simon Gibbons Order of Authors: Simon Gibbons; Shruti Beharry Abstract: The purpose of this review is to identify emerging or new psychoactive substances (NPS) by undertaking an online survey of the UK NPS market and to gather any data from online drug fora and published literature. Drugs from four main classes of NPS were identified: psychostimulants, dissociative anaesthetics, hallucinogens (phenylalkylamine-based and lysergamide-based materials) and finally benzodiazepines. For inclusion in the review the 'user reviews' on drugs fora were selected based on whether or not the particular NPS of interest was used alone or in combination. NPS that were use alone were considered. Each of the classes contained drugs that are modelled on existing illegal materials and are now covered by the UK New Psychoactive Substances Bill in 2016. Suggested Reviewers: Title Page (with authors and addresses) An overview of Emerging and New Psychoactive Substances in the United Kingdom Shruti Beharry and Simon Gibbons1 Research Department of Pharmaceutical and Biological Chemistry UCL School of Pharmacy -

Neuroplasticity in the Mesolimbic System Induced by Sexual Experience and Subsequent Reward Abstinence
Western University Scholarship@Western Electronic Thesis and Dissertation Repository 6-21-2012 12:00 AM Neuroplasticity in the Mesolimbic System Induced by Sexual Experience and Subsequent Reward Abstinence Kyle Pitchers The University of Western Ontario Supervisor Lique M. Coolen The University of Western Ontario Graduate Program in Anatomy and Cell Biology A thesis submitted in partial fulfillment of the equirr ements for the degree in Doctor of Philosophy © Kyle Pitchers 2012 Follow this and additional works at: https://ir.lib.uwo.ca/etd Recommended Citation Pitchers, Kyle, "Neuroplasticity in the Mesolimbic System Induced by Sexual Experience and Subsequent Reward Abstinence" (2012). Electronic Thesis and Dissertation Repository. 592. https://ir.lib.uwo.ca/etd/592 This Dissertation/Thesis is brought to you for free and open access by Scholarship@Western. It has been accepted for inclusion in Electronic Thesis and Dissertation Repository by an authorized administrator of Scholarship@Western. For more information, please contact [email protected]. NEUROPLASTICITY IN THE MESOLIMBIC SYSTEM INDUCED BY SEXUAL EXPERIENCE AND SUBSEQUENT REWARD ABSTINENCE (Spine Title: Sex, Drugs and Neuroplasticity) (Thesis Format: Integrated Article) By Kyle Kevin Pitchers Graduate Program in Anatomy and Cell Biology A thesis submitted in partial fulfillment of the requirements for degree of Doctor of Philosophy The School of Graduate and Postdoctoral Studies The University of Western Ontario London, Ontario, Canada © Kyle K. Pitchers, 2012 THE UNIVERSITY -
Full Prescribing Information Warning: Suicidal Thoughts
tablets (SR) BUPROPION hydrochloride extended-release HIGHLIGHTS OF PRESCRIBING INFORMATION anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe hydrochloride extended-release tablets (SR) was reported. However, the symptoms persisted in some Table 3. Adverse Reactions Reported by at Least 1% of Subjects on Active Treatment and at a tablets (SR) may be necessary when coadministered with ritonavir, lopinavir, or efavirenz [see Clinical These highlights do not include all the information needed to use bupropion hydrochloride patients attempting to quit smoking with Bupropion hydrochloride extended-release tablets, USP cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve. Greater Frequency than Placebo in the Comparator Trial Pharmacology (12.3)] but should not exceed the maximum recommended dose. extended-release tablets (SR) safely and effectively. See full prescribing information for (SR) for the occurrence of such symptoms and instruct them to discontinue Bupropion hydrochloride Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs extended-release tablets, USP (SR) and contact a healthcare provider if they experience such adverse The neuropsychiatric safety of Bupropion hydrochloride extended-release tablets (SR) was evaluated in Bupropion Bupropion may induce the metabolism of bupropion and may decrease bupropion exposure [see Clinical bupropion hydrochloride extended-release tablets (SR). Nicotine events. (5.2) a randomized, double-blind, active-and placebo-controlled study that included patients without a history Hydrochloride Hydrochloride Pharmacology (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary Transdermal BUPROPION hydrochloride extended-release tablets (SR), for oral use • Seizure risk: The risk is dose-related. -

The Effects of Alcohol and Nicotine Pretreatment During Adolescence on Adulthood Responsivity to Alcohol Antoniette M
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 2007 The effects of alcohol and nicotine pretreatment during adolescence on adulthood responsivity to alcohol Antoniette M. Maldonado University of South Florida Follow this and additional works at: http://scholarcommons.usf.edu/etd Part of the American Studies Commons Scholar Commons Citation Maldonado, Antoniette M., "The effects of alcohol and nicotine pretreatment during adolescence on adulthood responsivity to alcohol" (2007). Graduate Theses and Dissertations. http://scholarcommons.usf.edu/etd/2272 This Thesis is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. The Effects of Alcohol and Nicotine Pretreatment During Adolescence on Adulthood Responsivity to Alcohol by Antoniette M. Maldonado A thesis submitted in partial fulfillment of the requirements for the degree of Masters of Arts Department of Psychology College of Arts and Sciences University of South Florida Major Professor: Cheryl L. Kirstein, Ph.D. Mark Goldman, Ph.D. Toru Shimizu, Ph.D. David J. Drobes, Ph.D. Date of Approval: 18 October, 2007 Keywords: addiction, adolescent, alcohol-nicotine interactions, conditioned place preference, novelty preference © Copyright 2007, Antoniette M. Maldonado Dedication To my mom, Sylvia Ann Valdez. Mom, you are my very best friend and I do not know what I would have done without all of the support you gave me through every single step of this journey. You make such a difference in my life and I cannot even begin to describe how grateful I am to have you still here with me. -

New Persistent Opioid Abuse and the Brain Reward Circuit
Zhang L, Boysen PG. New Persistent Opioid Abuse and the Brain Reward Circuit. J Anesthesiol & Pain Therapy. 2020;1(1):11-13 Letter to the Editor Open Access New Persistent Opioid Abuse and the Brain Reward Circuit Ly Zhang*, Philip G. Boysen Department of Anesthesiology, University of Mississippi Medical Center, The Mississippi Critical Care Organization, USA Article Info New persistent opioid abuse in peri-operative and peri- procedural patients is reported to be ~6% in two large population- Article Notes 1 Received: December 06, 2019 based studies . In addressing the opioid crisis the CDC has developed Accepted: April 08, 2020 2 *Correspondence: approved opioids are prescribed by licensed professionals . The *Dr. Ly Zhang, Department of Anesthesiology, University of three categories. The first is prescription drugs, when legal and Mississippi Medical Center, The Mississippi Critical Care and fentanyl . Over time CDC data indicates a sharp uptick in opioid Organization, USA; Email: [email protected]. second and third3,4 categories involve illicit drugs, specifically heroin ©2020 Zhang L. This article is distributed under the terms of the prescription drugs5. Understanding the neurobiology of addiction Creative Commons Attribution 4.0 International License. deaths for heroin and fentanyl, but a flat incidence of overdose with and public health issues are integral to the understanding of how adds insight to the problem and treatment. In addition, the social the brain reward circuit is activated in the first place. human primates 50 years ago. Rats taught to push a lever to self – The brain reward circuit was described in rodents, then in non- aspectsadminister of addictive addictive behavior. -

Cross-Sectional Study of the Dispensation of Synthetic Anorectic Drugs in Community Pharmacies in the City of Cruz Alta – State of Rio Grande Do Sul
Brazilian Journal of Pharmaceutical Sciences vol. 50, n. 4, oct./dec., 2014 Article http://dx.doi.org/10.1590/S1984-82502014000400008 Cross-sectional study of the dispensation of synthetic anorectic drugs in community pharmacies in the city of Cruz Alta – State of Rio Grande do Sul Marcieli Maria Navarini1, Viviane Cecilia Kessler Nunes Deuschle2,*, Regis Augusto Norbert Deuschle3 1Faculty of Pharmacy, University of Cruz Alta, Rio Grande do Sul, Brazil,2,3Postgraduate Program in Pharmaceutical Sciences, Federal University of Santa Maria, Brazil Obesity is defined as the excess adipose tissue in the body. Drugs responsible for inhibiting the appetite are called anorectics or appetite suppressants. Sibutramine, fenproporex and amfepramone belongs to this class, and are capable of causing physical or psychological dependence. The aim of this study was to evaluate the frequency of prescriptions for appetite suppressants in community pharmacies at Cruz Alta, State of Rio Grande do Sul, Brazil. The sales of fenproporex, amfepramone and sibutramine in the months of September, October and November 2010 and April, May and June 2011 were compared. It was observed that the most commonly dispensed anorectic in the three community pharmacies analyzed was sibutramine. In the months of September, October and November 2010, consumption was higher, with sibutramine achieving 40.3% of overall sales, amfepramone 21% and, finally, fenproporex, 7.9%. The consumption of appetite suppressants was more prevalent in females, who represented 82% of total. The results suggested the existence of high consumption of anorectics, possibly related to the current concern with aesthetic standards, which emphasizes the importance of strict control over the marketing of these substances. -

Nicotine and Neurotransmitters
Module 2 —Legal Doesn’t Mean Harmless Overview Overview Summary This module focuses on how two drugs, nicotine and alcohol, change the functioning of the brain and body. Both drugs are widely used in the community, and for adults, using them is legal. Nonetheless, both alcohol and nicotine can have a strong impact on the functioning of the brain. Each can cause a number of negative effects on the body and brain, ranging from mild symptoms to addiction. The goal of this module is to help students understand that, although nicotine and alcohol are legal for adults, they are not harmless substances. Students will learn about how nicotine and alcohol change or disrupt the process of neurotransmission. Students will explore information on the short- and long- term effects of these two drugs, and also learn why these drugs are illegal for children and teens. Through the media, students are exposed to a great deal of information about alcohol and tobacco, much of which is misleading or scientifically inaccurate. This module will provide information on what researchers have learned about how nicotine and alcohol change the brain, and the resulting implications for safety and health. Learning Objectives At the end of this module: • Students can explain how nicotine disrupts neurotransmission. • Students can explain how alcohol use may harm the brain and the body. • Students understand how alcohol can intensify the effect of other drugs. • Students can define addiction and understand its basis in the brain. • Students draw conclusions about why our society regulates the use of nicotine and alcohol for young people. -

The Effects of Nicotine Administration on Behavior and Markers of Brain Plasticity in a Rodent Model of Psychosis" (2012)
East Tennessee State University Digital Commons @ East Tennessee State University Electronic Theses and Dissertations Student Works 5-2012 The ffecE ts of Nicotine Administration on Behavior and Markers of Brain Plasticity in a Rodent Model of Psychosis Marla K. Perna East Tennessee State University Follow this and additional works at: https://dc.etsu.edu/etd Part of the Chemical Actions and Uses Commons Recommended Citation Perna, Marla K., "The Effects of Nicotine Administration on Behavior and Markers of Brain Plasticity in a Rodent Model of Psychosis" (2012). Electronic Theses and Dissertations. Paper 1432. https://dc.etsu.edu/etd/1432 This Dissertation - Open Access is brought to you for free and open access by the Student Works at Digital Commons @ East Tennessee State University. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Digital Commons @ East Tennessee State University. For more information, please contact [email protected]. The Effects of Nicotine Administration on Behavior and Markers of Brain Plasticity in a Rodent Model of Psychosis ________________________ A dissertation presented to the faculty of the Department of Anatomy and Cell Biology East Tennessee State University In partial fulfillment of the requirements for the degree Doctor of Philosophy in Biomedical Sciences ________________________ by Marla Perna May 2012 ________________________ Russell W. Brown, Chair Ronald H. Baisden Theresa A. Harrison Gregory A. Ordway Brooks B. Pond David S. Roane Keywords: psychosis, adolescence, nicotine, dopamine, synaptic plasticity ABSTRACT The Effects of Nicotine Administration on Behavior and Markers of Brain Plasticity in a Rodent Model of Psychosis by Marla Perna Schizophrenia affects about 1% of the population.