Cobas SARS-Cov-2 Instructions For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transmittal 3771, Claims Processing
Department of Health & CMS Manual System Human Services (DHHS) Pub 100-04 Medicare Claims Processing Centers for Medicare & Medicaid Services (CMS) Transmittal 3771 Date: May 12, 2017 Change Request 10055 SUBJECT: New Waived Tests I. SUMMARY OF CHANGES: This Change Request (CR) will inform contractors of new Clinical Laboratory Improvement Amendments of 1988 (CLIA) waived tests approved by the Food and Drug Administration. Since these tests are marketed immediately after approval, the Centers for Medicare & Medicaid Services (CMS) must notify its contractors of the new tests so that the contractors can accurately process claims. There are 12 newly added waived complexity tests. The initial release of this Recurring Update Notification applies to Chapter 16, section 70.8 of the IOM. EFFECTIVE DATE: January 1, 2017 *Unless otherwise specified, the effective date is the date of service. IMPLEMENTATION DATE: July 3, 2017 Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated) R=REVISED, N=NEW, D=DELETED-Only One Per Row. R/N/D CHAPTER / SECTION / SUBSECTION / TITLE N/A N/A III. FUNDING: For Medicare Administrative Contractors (MACs): The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. -

COVID-19 and Neonatal Respiratory Care: Current Evidence and Practical Approach
Published online: 2020-05-02 780 Review Article COVID-19 and Neonatal Respiratory Care: Current Evidence and Practical Approach Wissam Shalish, MD1 Satyanarayana Lakshminrusimha, MD2 Paolo Manzoni, MD3 Martin Keszler, MD4 Guilherme M. Sant’Anna, MD, PhD, FRCPC1 1 Neonatal Division, Department of Pediatrics, McGill University Address for correspondence Guilherme M. Sant’Anna, MD, PhD, Health Center, Montreal, Quebec, Canada FRCPC, Neonatal Division, Department of Pediatrics, McGill University 2 Department of Pediatrics, UC Davis, Sacramento, California Health Center, 1001 Décarie Boulevard, Room 05.2711, 3 Department of Pediatrics and Neonatology, University Hospital Montreal H4A 3J1, Canada (e-mail: [email protected]). Degli Infermi, Biella, Italy 4 Department of Pediatrics, Women and Infants Hospital, Brown University, Providence, Rhode Island Am J Perinatol 2020;37:780–791. Abstract The novel coronavirus disease 2019 (COVID-19) pandemic has urged the development and implementation of guidelines and protocols on diagnosis, management, infection control strategies, and discharge planning. However, very little is currently known about neonatal COVID-19 and severe acute respiratory syndrome–coronavirus-2 (SARS-CoV-2) infections. Thus, many questions arise with regard to respiratory care after birth, necessary protection to health care workers (HCW) in the delivery room and neonatal intensive care unit (NICU), and safety of bag and mask ventilation, noninvasive respiratory support, deep suctioning, endotracheal intubation, and mechanical ventilation. Indeed, these questions have created tremendous confusion amongst neonatal HCW. In this manuscript, we comprehensively reviewed the current evidence regarding COVID-19 perinatal transmission, respiratory outcomes of neonates born to mothers with COVID-19 and infants with documented SARS- CoV-2 infection, and the evidence for using different respiratory support modalities and aerosol-generating procedures in this specific population. -

COVID-19 and Total Laryngectomy—A Report of Two Cases
AORXXX10.1177/0003489420935500Annals of Otology, Rhinology & LaryngologyPaderno et al 935500case-report2020 Case Report Annals of Otology, Rhinology & Laryngology 1 –4 COVID-19 and Total Laryngectomy © The Author(s) 2020 Article reuse guidelines: sagepub.com/journals-permissions —A Report of Two Cases DOI:https://doi.org/10.1177/0003489420935500 10.1177/0003489420935500 journals.sagepub.com/home/aor Alberto Paderno, MD1 , Milena Fior, MD1, Giulia Berretti, MD1, Francesca Del Bon, MD1, Alberto Schreiber, MD, PhD1, Alberto Grammatica, MD1, Davide Mattavelli, MD1, and Alberto Deganello, MD, PhD1 Abstract Objective: To date, no cases have been reported on the effects of COVID-19 in laryngectomees. Case Presentation: We herein presented two clinical cases of laryngectomized patients affected by COVID-19, detailing their clinical course and complications. Discussion: In our experience, permanent tracheostomy did not significantly affect the choice of treatment. However, dedicated devices and repeated tracheal toilettes may be needed to deal with oxygen-therapy-related tracheal crusting. Conclusion: In conclusion, laryngectomees should be considered a vulnerable population that may be at risk for worse outcomes of COVID-19 due to anatomical changes in their airways. The role of the ENT specialist is to guide airway management and inform the support-staff regarding specific needs of these patients. Keywords COVID-19, coronavirus, SARS-CoV-2, laryngectomy, management Introduction At admission (March 9, 2020), the most relevant clinical findings included severe oxygen desaturation (76%), tachy- To date, the effects of COVID-19 on laryngectomized pnea, cyanosis, lymphocytopenia, and C reactive protein patients is unknown, with no cases reported so far. After (CRP; 185 mg/L). -
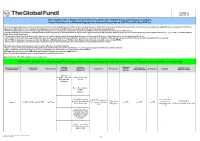
List of SARS-Cov-2 Diagnostic Test Kits and Equipments Eligible For
Version 33 2021-09-24 List of SARS-CoV-2 Diagnostic test kits and equipments eligible for procurement according to Board Decision on Additional Support for Country Responses to COVID-19 (GF/B42/EDP11) The following emergency procedures established by WHO and the Regulatory Authorities of the Founding Members of the GHTF have been identified by the QA Team and will be used to determine eligibility for procurement of COVID-19 diagnostics. The product, to be considered as eligible for procurement with GF resources, shall be listed in one of the below mentioned lists: - WHO Prequalification decisions made as per the Emergency Use Listing (EUL) procedure opened to candidate in vitro diagnostics (IVDs) to detect SARS-CoV-2; - The United States Food and Drug Administration’s (USFDA) general recommendations and procedures applicable to the authorization of the emergency use of certain medical products under sections 564, 564A, and 564B of the Federal Food, Drug, and Cosmetic Act; - The decisions taken based on the Canada’s Minister of Health interim order (IO) to expedite the review of these medical devices, including test kits used to diagnose COVID-19; - The COVID-19 diagnostic tests approved by the Therapeutic Goods Administration (TGA) for inclusion on the Australian Register of Therapeutic Goods (ARTG) on the basis of the Expedited TGA assessment - The COVID-19 diagnostic tests approved by the Ministry of Health, Labour and Welfare after March 2020 with prior scientific review by the PMDA - The COVID-19 diagnostic tests listed on the French -

Recommended Laboratory HIV Testing Algorithm for Serum Or Impact of HIV/AIDS
Journal of HIV for Clinical and Scientific Research eertechz Uğur Tüzüner*, Begüm Saran Gülcen Review article and Mehmet Özdemir Necmettin Erbakan University, Meram Medical Faculty, Medical Microbiology Department, Medical Virology Laboratory Algorithm in HIV Division. Konya, Turkey Dates: Received: 02 April, 2016; Accepted: 18 April, Infection Diagnosis 2016; Published: 19 April, 2016 *Corresponding author: Dr. Uğur Tüzüner, Abstract Necmettin Erbakan University, Meram Medical Faculty, Medical Microbiology Department, AIDS caused by HIV is an infection disease which was defined firstly in the USA in 1981. Since Konya, Turkey, Tel:+90 332 223 7029; E-mail: then, number of AIDS patients has increased continuously. About 36.9 million people are living with HIV around the world. Approximately 15 million people living with HIV were receiving antiretroviral therapy. Early detection is important due to the high risk of transmission that precedes seroconversion www.peertechz.com and also because it provides an opportunity to improve health outcomes with an early antiretroviral therapy. HIV testing is the key part of diagnosis and prevention efforts. Many tests have been used ISSN: 2455-3786 in the diagnosis of HIV over years and with developing testing methods, accuracy of the laboratory Keywords: HIV; Laboratory diagnosis; Algorithm diagnosis of HIV infection has been improved. Detecting p24 antigens, HIV 1-2 antibodies and HIV nucleic acid demonstrated that antibody testing alone might miss a considerable percentage of HIV infections detectable by these tests. This review provides updated recommendations and algorithm for HIV testing that are necessary for diagnosing HIV and offers approaches for accurate assessment of test results. Introduction HIV infection (asymptomatic HIV infection or clinical latency), and progression to AIDS (the late stage of HIV infection). -

COVID 19 Inpatient Testing Guidelines
COVID-19 Inpatient COVID-19 Testing Protocol, Version 7, 20210714 Owners: T. Bouton, J. Hudspeth Inpatient COVID-19 Testing Protocol A. Who to test? BMC tests all patients being admitted to the hospital, with the exception of COVID- recovered patients who are within 9 months of their initial positive COVID test and remain asymptomatic (for outpatient testing algorithms, please refer to the outpatient testing protocol). o Refer to COVID-Flu Testing Winter 2020 for guidance on testing patients admitted with flu-like febrile respiratory illness and sepsis-like syndrome requiring hospitalization. If a patient who is already admitted develops symptoms potentially attributable to COVID- 19 and warrants testing per your clinical opinion, they should be retested (even if their admission test was negative). Note: For COVID-recovered patients who have new symptoms of COVID-19 within 9 months of initial positive test AND for whom an alternate etiology cannot be identified, also consider retesting. o Promptly alert the nurse of your concern so precautions are instituted o There are a wide range of symptoms and presentations potentially compatible with COVID including: Fever, cough, shortness of breath, new anosmia, unexplained hypoxia, diarrhea (more than 3 watery bowel movements per day), nausea or vomiting, dizziness, headache, muscle aches, throat pain, rhinorrhea, fatigue and others. o In accordance with guidelines, testing should be conducted for patients with: . ST elevation MI . Unprovoked venous thromboembolism . Multifocal PNA or ground glass opacities on CT without clear alternative diagnosis o Diagnoses for which one should consider testing for COVID: . New seizure . New stroke . Myocarditis, stress cardiomyopathy, coronary spasm, right heart failure Direct admissions to BMC should be assessed for symptoms of COVID (or results of prior COVID testing) by the accepting physician prior to accepting the patient. -

Disparate Nasopharyngeal and Tracheal COVID-19 Diagnostic Test
Revised complete Manuscript Click here to access/download;Complete Manuscript;laryngectomy Testing manuscript plaintext.docx This manuscript has been accepted for publication in Otolaryngology-Head and Neck Surgery. 1 1 Disparate Nasopharyngeal and Tracheal COVID-19 Diagnostic Test 2 Results in a Patient with Total Laryngectomy 3 Running Title: “COVID-19 Testing with Total Laryngectomy” 4 5 Tirth R. Patel, MD1; Joshua E. Teitcher, CCC-SLP2; Bobby A. Tajudeen, MD1; Peter C. 6 Revenaugh, MD1 7 8 1. Department of Otolaryngology—Head and Neck Surgery, Rush University Medical 9 Center, Chicago, Illinois 10 2. Department of Hematology/Oncology, Rush University Medical Center, Chicago, Illinois 11 12 Corresponding Author: 13 Tirth R. Patel, MD 14 Department of Otolaryngology—Head and Neck Surgery 15 Rush University Medical Center 16 1650 West Harrison Street, Suite 550 17 Chicago, Illinois 60612 18 Phone: 312-942-6100 19 Email: [email protected] 20 21 22 Keywords: COVID-19, coronavirus, laryngectomy 23 Sponsor or Funding Source: None 24 Conflicts of Interest: None 25 26 Author Contributions: 27 T.R.P.: Conception and design; data acquisition; drafting, revision, final approval of article 28 J.E.T.: Conception and design; data acquisition; drafting, revision, final approval of article 29 B.A.T.: Conception and design; drafting, revision, final approval of article 30 P.C.R.: Conception and design; drafting, revision, final approval of article 31 32 This manuscript has been accepted for publication in Otolaryngology-Head and Neck Surgery. This manuscript has been accepted for publication in Otolaryngology-Head and Neck Surgery. 2 33 Introduction 34 Coronavirus disease 2019 (COVID-19), caused by SARS-CoV-2 virus, has been declared 35 a pandemic by the World Health Organization1. -

Microbiology Specimen Collection
Martin Health System Stuart, Florida Laboratory Services Microbiology Specimen Collection The recovery of pathogenic organisms responsible for an infectious process is dependent on proper collection and transportation of a specimen. An improperly collected or transported specimen may lead to failure to isolate the causative organism(s) of an infectious disease or may result in the recovery and subsequent treatment of contaminating organisms. Improper handling of specimens may also lead to accidental exposure to infectious material. GENERAL GUIDELINES FOR COLLECTION: 1. Follow universal precaution guidelines, treating all specimens as potentially hazardous. 2. Whenever possible, collect specimen before antibiotics are administered. 3. Collect the specimen from the actual site of infection, avoiding contamination from adjacent tissues or secretions. 4. Collect the specimen at optimal time i.e. Early morning sputum for AFB First voided specimen for urine culture Specimens ordered x 3 should be 24 hours apart (exception: Blood cultures which are collected as indicated by the physician) 5. Collect sufficient quantity of material for tests requested. 6. Use appropriate collection and transport container. Refer to the Microbiology Quick Reference Chart or to the specific source guidelines. Containers should always be tightly sealed and leak-proof 7. Label the specimen with the Patient’s First and Last Name Date of Birth Collection Date and Time Collector’s First and Last Name Source 8. Submit specimen in the sealed portion of a Biohazard specimen bag. 9. Place signed laboratory order in the outside pocket of the specimen bag. 10. Include any pertinent information i.e. recent travel or relocation, previous antibiotic therapy, unusual suspected organisms, method or environment of wound infliction 11. -
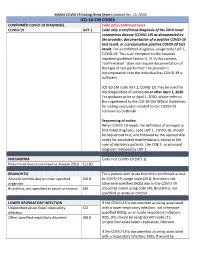
Icd-10-Cm Codes
MGMA COVID-19 Coding Cheat Sheet (Updated Dec. 23, 2020) ICD-10-CM CODES CONFIRMED COVID-19 DIAGNOSIS Code only confirmed cases COVID-19 U07.1 Code only a confirmed diagnosis of the 2019 novel coronavirus disease (COVID-19) as documented by the provider, documentation of a positive COVID-19 test result, or a presumptive positive COVID-19 test result. For a confirmed diagnosis, assign code U07.1, COVID-19. This is an exception to the hospital inpatient guideline Section II, H. In this context, “confirmation” does not require documentation of the type of test performed; the provider’s documentation that the individual has COVID-19 is sufficient. ICD-10-CM code U07.1, COVID-19, may be used for discharges/date of service on or after April 1, 2020. For guidance prior to April 1, 2020, please refer to the supplement to the ICD-10-CM Official Guidelines for coding encounters related to the COVID-19 coronavirus outbreak. Sequencing of codes: When COVID-19 meets the definition of principal or first-listed diagnosis, code U07.1, COVID-19, should be sequenced first, and followed by the appropriate codes for associated manifestations, except in the case of obstetrics patients. Use O98.5- as principal diagnosis followed by U07.1. PNEUMONIA Code first COVID-19 (U07.1) Pneumonia due to coronavirus disease 2019 J12.82 BRONCHITIS For a patient with acute bronchitis confirmed as due Acute bronchitis due to other specified J20.8 to COVID-19, assign code J20.8. Bronchitis not organism otherwise specified (NOS) due to the COVID-19 Bronchitis, not specified as acute or chronic J40 should be coded using code J40, Bronchitis, not specified as acute or chronic. -

Rapid Review: Performance and Feasibility of Rapid COVID-19 Tests
COVID-19 Scientific Advisory Group Rapid Evidence Report Do the rapid COVID-19 tests on the market represent a feasible opportunity for Alberta? 1. What are the reported performance characteristics of the rapid COVID-19 tests that have been approved for commercial (diagnostic) use in Canada? 2. What are the optimal strategies for deployment of rapid testing, to improve either clinical care or outbreak control in health care and community settings? Context • It is unclear how the rapid (point-of-care) molecular and antigen tests for COVID-19 tests compare to each other. • Five point-of-care testing devices/systems have been approved for diagnostic use by Health Canada: 1) BD Veritor System for Rapid Detection of SARS-CoV-2 (Becton Dickinson and Company) 2) BKit Virus Finder COVID-19 (Hyris Ltd.) 3) ID NOW COVID-19 (Abbott Diagnostics Scarborough Inc.) 4) Panbio COVID-19 Ag Rapid Test Device (Abbott Rapid Diagnostics) 5) Xpert Xpress SARS-CoV-2 (Cepheid). • The federal government has committed to distributing the consumables for the Abbott ID NOW and PanBio testing kits to each Canadian jurisdiction, however, the strategy for deploying the rapid test kits will be the responsibility of the public health leaders in the provincial/territorial governments. • The implementation of rapid testing in other jurisdictions offers an opportunity to learn from their experiences in deploying rapid COVID-19 tests and avoid potential missteps. These implementation activities have included mass assessments, population-level testing to determine prevalence, returned traveler assessment, staff screening at long-term care facilities, and school testing. Key Messages from the Evidence Summary • The body of evidence for rapid testing platforms is poor – many of the studies are at high risk of bias. -
Lower Respiratory SARS-Cov-2 Testing for Lung Donors
Notice of OPTN Emergency Policy Change Lower Respiratory SARS-CoV-2 Testing for Lung Donors Sponsoring Committee: Ad Hoc Disease Transmission Advisory Policies Affected: Policy 1.2: Definitions Policy 2.9: Required Deceased Donor Infectious Disease Testing Public Comment: August 3, 2021-September 30, 2021 Board Approved: April 26, 2021 Effective Date: May 27, 2021 Summary of Changes The policy change defines what a lower respiratory specimen is and requires that all lung donors receive lower respiratory specimen testing by nucleic acid test (NAT). The policy specifies that testing results must be available pre-transplant of lungs. Purpose of Policy Change There has been accumulating evidence of a patient safety risk to lung recipients in four recent cases of deceased lung donors testing negative for SARS-CoV-2 by upper respiratory specimen and retrospectively testing positive by lower respiratory specimen. Three cases resulted in donor-derived transmission to lung recipients while the fourth resulted in lung discard. One lung recipient has died as a result of the donor-derived transmission. As of March 2021, only 60% of lung donors were tested by lower respiratory specimen.1 Policy is needed to ensure organ procurement organizations (OPOs) perform and obtain results from lower respiratory specimen testing for all potential deceased lung donors to avoid SARS-CoV-2 (COVID-19) transmission to lung recipients. The policy change is emergent because of the significant patient safety implications of donor-derived COVID-19 and the subsequent risk of patient mortality. The policy change requires nucleic acid testing (NAT) for COVID-19 by lower respiratory specimen for all potential deceased lung donors, with results being available prior to lung transplantation. -

Respiratory Specimens
1.1. Department Of Pathology MIC.20650.04 Collection Guidelines - Respiratory Cultures Version#4 Department POLICY NO. PAGE NO. Microbiology 1408 1 OF 8 Printed copies are for reference only. Please refer to the electronic copy for the latest version. 1. Purpose 1.1. To provide accurate specimen collection information to the units as part of our on-line collection manual 2. Principles 2.1. Proper selection, collection, and handling of specimens for microbiology is necessary to ensure quality results that have the greatest impact on patient care. 3. Procedure The following page(s) have been posted on the on-line collection manual. • Note that much of the collection information was taken from the Clinical Microbiology Procedures Handbook. The authors have written the following in their manual for collection procedures “the following can be coped for preparation of a specimen collection instruction manual for physicians and other caregivers” 4. References 4.1. Clinical and Laboratory Standards institute. 2008. Viral Culture; Approved Guideline; M41-A. Clinical and Laboratory Standards Institute, Wayne, PA. 4.2. York, Mary K, et al. (2004). Guidelines for Performance of Respiratory Tract. In Clinical Microbiology Procedures Handbook, Volume 2, (Isenberg, H. D., Ed.), pp. 3.11.1.1. American Society for Microbiology, Washington, DC. 4.3. York, Mary K, et al. (2004). Lower Respiratory Tract Cultures. In Clinical Microbiology Procedures Handbook, Volume 2, (Isenberg, H. D., Ed.), pp. 3.11.2.1–10. American Society for Microbiology, Washington, DC. 4.4. York, Mary K, et al. (2004). Body Fluid Cultures (Excluding Blood, Cerebral Spinal Fluid, and Urine).