Laboratory Testing for COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

China Confronts Covid-19
CHINA CONFRONTS COVID-19 By DAKE KANG and COLLEAGUES Associated Press STORY TK | ASSOCIATED PRESS 1 of 2 CRACKDOWN IN CHINA 1. CHINA DIDN’T WARN PUBLIC OF LIKELY PANDEMIC FOR 6 KEY DAYS April 15, 2020: Top Chinese ofcials secretly determined they were likely facing a pandemic from a new coronavirus in mid-January, ordering preparations even as they downplayed it in public. https://apnews.com/article/68a9e1b91de4fc166acd6012d82c2f9 2. CHINA DELAYED RELEASING CORONAVIRUS INFO, FRUSTRATING WHO June 3, 2020: Even as the World Health Organization publicly praised China, it privately complained about the lack of information it was getting on the new coronavirus. https://apnews.com/article/3c061794970661042b18d5aeaaed9fae 3. CHINA TESTING BLUNDERS STEMMED FROM SECRET DEALS WITH FIRMS Dec. 3, 2020: Secrecy and cronyism crippled China’s testing capacity in the early days of the outbreak, an Associated Press investigation has found. https://apnews.com/article/china-virus-testing-secret-deals-frms- 312f4a953e0264a3645219a08c62a0ad TABLE OF CONTENTS | ASSOCIATED PRESS https://apnews.com/article/68a9e1b91de4fc166acd6012d82c2f9 1 Xie Huanchi/Xinhua via AP Chinese President Xi Jinping talks by video with patients and medical workers at the Huoshenshan Hospital in Wuhan in central China’s Hubei Province in a video released March 10, 2020. April 15, 2020 China didn’t warn public of likely pandemic for 6 key days By ASSOCIATED PRESS Associated Press In the six days after top Chinese ofcials secretly determined they likely were facing a pandemic from a new coronavirus, the city of Wuhan at the epicenter of the disease hosted a mass banquet for tens of thousands of people; millions began traveling through for Lunar New Year celebrations. -

Transmittal 3771, Claims Processing
Department of Health & CMS Manual System Human Services (DHHS) Pub 100-04 Medicare Claims Processing Centers for Medicare & Medicaid Services (CMS) Transmittal 3771 Date: May 12, 2017 Change Request 10055 SUBJECT: New Waived Tests I. SUMMARY OF CHANGES: This Change Request (CR) will inform contractors of new Clinical Laboratory Improvement Amendments of 1988 (CLIA) waived tests approved by the Food and Drug Administration. Since these tests are marketed immediately after approval, the Centers for Medicare & Medicaid Services (CMS) must notify its contractors of the new tests so that the contractors can accurately process claims. There are 12 newly added waived complexity tests. The initial release of this Recurring Update Notification applies to Chapter 16, section 70.8 of the IOM. EFFECTIVE DATE: January 1, 2017 *Unless otherwise specified, the effective date is the date of service. IMPLEMENTATION DATE: July 3, 2017 Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated) R=REVISED, N=NEW, D=DELETED-Only One Per Row. R/N/D CHAPTER / SECTION / SUBSECTION / TITLE N/A N/A III. FUNDING: For Medicare Administrative Contractors (MACs): The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. -

EURO SKO NORGE AS - Leverandørliste Denne Listen Omfatter Leverandører Som Euro Sko Norge AS Bruker Til Produksjon Av Egne Merkevarer
EURO SKO NORGE AS - Leverandørliste Denne listen omfatter leverandører som Euro Sko Norge AS bruker til produksjon av egne merkevarer. Siden leverandørkjeden endres fra tid til annen, for å gjenspeile virksomhetens behov, kan avvik forekomme. Leverandørlisten blir oppdatert årlig. Euro Sko Norge AS har bygget sterke, strategiske bånd med våre leverandører, slik at vi kan offentliggjøre navnene deres, samt plassering uten bekymring for konkurranse i vår bransje. Vi håper offentliggjøringen av listen fremmer deling, samarbeid og bærekraftig produksjon på en måte som kan forbedre arbeidsforholdene og ytterligere beskytte rettighetene for arbeiderene på fabrikkene. Publisert: Juni 2020 Land Garveri navn City/province Albania Fital shpk Kamza/Tirane Bangladesh Apex Dhaka Kina Yangzhou OuHao Handicraft Co., Yangzhou/Jiangsu Zhenjiang Infiniti Shoes Co. Ltd. Zhenjiang/Jiangsu Hengshui Guanyi Leather Products Co Ltd Hengshui/Hebei Yangzhou Duofulai Footwear Co., Ltd. Yangzhou/Jiangsu TM SHOES Zhenjiang/Jiangsu Jinjiang DEVO Shoes & Garments Co., Ltd JinJiang/Fujian Jinbu handicraft Co. Ltd Tianchang/Anhui FuDeLai Zhejiang Dongguan Jiale Shoes Co Ltd. Dongguan/Guangdong Changzhou Qifa Shoes Changzhou/Jiangsu Jolly/JinXi Dongguan/Guangdong LETA FuNan/Anhui Yazhouren Wenzhou/Zhejiang Hangzhou Luke Shoe Co., Ltd. Hangzhou/Zhejiang Shuangha Shuang Ha/Zhejiang Shicheng County Changan Sun Shoes and GarmentGanzhou/JiangxXi Co., Ltd. JinJiang Xinnanxing Shoes and plastic manufacturingChendai/Jinjiang Co Jinjiang Peike Shoes Co., Ltd Chendai/Jinjiang JinJiang Zuta JinJiang/Fujian Fujian Jinjiang Qiaobu Shoes Co.Ltd JinJiang/Fujian Funtag JinJiang/Fujian Huidong Taizifa Shoes Factory HuiZhou/Guangdong Xinyan Shoes Factory HuiZhou/Guangdong Hui Zhou Wei Ming Shoes Co.,Ltd Huangbu Town/Guangdong Shangyuanxin Shoes Factory Huangbu/Guangdong Soon Seng Footwear Company Huiyang City/Guangdong Jinshun Company Dongguan/Guangdong Jin Jiang Xinya Sports Goods Co., Ltd Jwuli/Jinjiang Tengda Sport Products Co Ltd Chidian/Jinjiang Taizhoushi Chiye Shoes Branches Co., Ltd. -

A Chinese Feminist's Reflections on the Pandemic: Gender, Surveillance
1 gender, surveillance& rights onthepandemic: reflections A Chinesefeminist’s CAI YIPING CAI YIPING - JUNE 2020 - TALKS ON COVID - 19 TALKS DAWN DAWN On January 20, 2020 83-year-old Dr Zhong Nanshan solemnly announced on CCTV—on behalf of the National Commission of Health—that the new coronavirus pneumonia (discovered in Wuhan) is transmittable amongst people. After a month had passed, Cai Yiping took a train from Beijing to Tianjin to visit her parents for Chinese New Year—the Spring Festival. She noticed the few passengers travelling on public transport wearing masks and the lack of vehicles and pedestrians in the two cities. The exception, were the patrons queued up to buy festival food at the popular bakeries in preparation for the Spring Festival. Two days before the Chinese New Year, Wuhan was locked down. Movement of people was stopped and confinement measures were soon nationally imposed and it was as if the virus pressed a magic button putting into hibernation 1.4 billion people. Soon after, doctors and nurses across the country were deployed 2 to Wuhan and Hubei provinces as the health workers were on the verge of collapse—a result of the flooding in of patients seeking diagnosis and treatment. By mid-April, it was reported that a total of 42, 600 medical personnel supported Hubei, two-thirds of which were women. 100 days have passed since the lockdown of Wuhan and a glimpse CAI YIPING - JUNE 2020 of hope emerges. Children are now playing in parks, major cities now - witness traffic jams, people are dining out at their favourite restaurants and it seems that life has returned to normal. -

Presentation: IPPR Co-Chairs
World Health Organization Executive Board Special Session October 6, 2020 Update from the Co-Chairs of The Independent Panel for Pandemic Preparedness and Response The Right Honourable Helen Clark, Co-Chair Her Excellency Ellen Johnson Sirleaf, Co-Chair Progress to Date – Key Milestones Resolution 73.1 WHO Director Secretariat Terms of Reference Executive Board adopted by World General appointed established. finalized. Special Session Health Assembly Co-Chairs for the Panelist Independent Panel nominations and Independent Panel for Pandemic comments on draft assembled and held st Preparedness & Terms of Reference. its 1 meeting. Response. Panelists selected May 2020 July 2020 August 2020 September 2020 October 2020 Terms of Reference • The Panel will review experience gained and lessons learned from the international health response to COVID-19 as coordinated by WHO and assess: • (i) the overall relevance and effectiveness of the international health response to the COVID-19 pandemic; WHO IHR Review • (ii) the functioning of the International Health Regulations (2005) and the status of Committee implementation of the relevant recommendations of previous IHR Review Committees; • (iii) the effectiveness of the mechanisms at WHO’s disposal and the actions of WHO and their timelines pertaining to the COVID-19 pandemic; • (iv) WHO’s contribution to United Nations-wide efforts. • In reviewing the experience gained and lessons learned from the WHO-coordinated international health response to COVID-19 as stated in the resolution the Panel will also: • (v) examine global health security threats and provide an analysis of past and future challenges and lessons learned; • (vi) include in its work analysis of the broader impacts of pandemics, including economic and social ones, and make recommendations to the extent that they have a direct bearing on future threats to global health security. -

Risk Factors for Carbapenem-Resistant Pseudomonas Aeruginosa, Zhejiang Province, China
Article DOI: https://doi.org/10.3201/eid2510.181699 Risk Factors for Carbapenem-Resistant Pseudomonas aeruginosa, Zhejiang Province, China Appendix Appendix Table. Surveillance for carbapenem-resistant Pseudomonas aeruginosa in hospitals, Zhejiang Province, China, 2015– 2017* Years Hospitals by city Level† Strain identification method‡ excluded§ Hangzhou First 17 People's Liberation Army Hospital 3A VITEK 2 Compact Hangzhou Red Cross Hospital 3A VITEK 2 Compact Hangzhou First People’s Hospital 3A MALDI-TOF MS Hangzhou Children's Hospital 3A VITEK 2 Compact Hangzhou Hospital of Chinese Traditional Hospital 3A Phoenix 100, VITEK 2 Compact Hangzhou Cancer Hospital 3A VITEK 2 Compact Xixi Hospital of Hangzhou 3A VITEK 2 Compact Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University 3A MALDI-TOF MS The Children's Hospital of Zhejiang University School of Medicine 3A MALDI-TOF MS Women's Hospital, School of Medicine, Zhejiang University 3A VITEK 2 Compact The First Affiliated Hospital of Medical School of Zhejiang University 3A MALDI-TOF MS The Second Affiliated Hospital of Zhejiang University School of 3A MALDI-TOF MS Medicine Hangzhou Second People’s Hospital 3A MALDI-TOF MS Zhejiang People's Armed Police Corps Hospital, Hangzhou 3A Phoenix 100 Xinhua Hospital of Zhejiang Province 3A VITEK 2 Compact Zhejiang Provincial People's Hospital 3A MALDI-TOF MS Zhejiang Provincial Hospital of Traditional Chinese Medicine 3A MALDI-TOF MS Tongde Hospital of Zhejiang Province 3A VITEK 2 Compact Zhejiang Hospital 3A MALDI-TOF MS Zhejiang Cancer -

Potential Factors Influencing Repeated SARS Outbreaks in China
International Journal of Environmental Research and Public Health Review Potential Factors Influencing Repeated SARS Outbreaks in China Zhong Sun 1 , Karuppiah Thilakavathy 1,2 , S. Suresh Kumar 2,3, Guozhong He 4,* and Shi V. Liu 5,* 1 Department of Biomedical Sciences, Faculty of Medicine & Health Sciences, University Putra Malaysia, UPM Serdang 43400, Selangor, Malaysia; [email protected] (Z.S.); [email protected] (K.T.) 2 Genetics and Regenerative Medicine Research Group, Faculty of Medicine & Health Sciences, University Putra Malaysia, UPM Serdang 43400, Selangor, Malaysia; [email protected] 3 Department of Medical Microbiology and Parasitology, University Putra Malaysia, UPM Serdang 43400, Selangor, Malaysia 4 Institute of Health, Kunming Medical University, Kunming 650500, China 5 Eagle Institute of Molecular Medicine, Apex, NC 27523, USA * Correspondence: [email protected] (G.H.); [email protected] (S.V.L.) Received: 28 January 2020; Accepted: 29 February 2020; Published: 3 March 2020 Abstract: Within last 17 years two widespread epidemics of severe acute respiratory syndrome (SARS) occurred in China, which were caused by related coronaviruses (CoVs): SARS-CoV and SARS-CoV-2. Although the origin(s) of these viruses are still unknown and their occurrences in nature are mysterious, some general patterns of their pathogenesis and epidemics are noticeable. Both viruses utilize the same receptor—angiotensin-converting enzyme 2 (ACE2)—for invading human bodies. Both epidemics occurred in cold dry winter seasons celebrated with major holidays, and started in regions where dietary consumption of wildlife is a fashion. Thus, if bats were the natural hosts of SARS-CoVs, cold temperature and low humidity in these times might provide conducive environmental conditions for prolonged viral survival in these regions concentrated with bats. -

Focus on Scientists Who Tamed Virus
CHINA DAILY | HONG KONG EDITION Monday, December 7, 2020 | 7 CHINA From left: Cao Bin, deputy director of the National Center for Respiratory Medicine, and vice-president of the China-Japan Friendship Hospital in Beijing; Han Qide, academician of the Chinese Academy of Sciences, pathophysiologist and honorary president of the China Association for Science and Technology; Cheng Jing, academician of the Chinese Academy of Engineering and medical biophysicist; Wu Yiling, CAE academician, doctor of traditional Chinese medicine and founder of Shijiazhuang Yiling Pharmaceutical. PHOTOS BY ZHU XINGXIN / CHINA DAILY Zhong Nanshan (left), a prominent respiratory disease expert and CAE academician, chats with Wang Chen, CAE vice- president and president of the Chinese Academy of Medical Sciences , at the opening ceremony of the 2020 Annual Con- gress of the Chinese Thoracic Society in Shenzhen, Guangdong province, on Oct 23. Focus on scientists who tamed virus In this year’s battle to contain COVID19, Chinese medical scientists have always been on the front line and made important contributions. China Daily photographer Zhu Xingxin zooms in on some of the scientists at the forefront of the struggle. Clockwise from left: Huang Jiefu (center), hepatobiliary surgery specialist and director of the China National Organ Donation and Transplantation Committee, at a public event promoting organ donation in Beijing in June. Zeng Yixin, CAS academician, oncologist and deputy director of the National Health Commission; Yang Weizhong, vice-president of the Chinese Preventive Medicine Association and executive president of the School of Population Medicine and Public Health at Peking Union Medical College.. -

COVID-19: Make It the Last Pandemic
COVID-19: Make it the Last Pandemic Disclaimer: The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Independent Panel for Pandemic Preparedness and Response concerning the legal status of any country, territory, city of area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Report Design: Michelle Hopgood, Toronto, Canada Icon Illustrator: Janet McLeod Wortel Maps: Taylor Blake COVID-19: Make it the Last Pandemic by The Independent Panel for Pandemic Preparedness & Response 2 of 86 Contents Preface 4 Abbreviations 6 1. Introduction 8 2. The devastating reality of the COVID-19 pandemic 10 3. The Panel’s call for immediate actions to stop the COVID-19 pandemic 12 4. What happened, what we’ve learned and what needs to change 15 4.1 Before the pandemic — the failure to take preparation seriously 15 4.2 A virus moving faster than the surveillance and alert system 21 4.2.1 The first reported cases 22 4.2.2 The declaration of a public health emergency of international concern 24 4.2.3 Two worlds at different speeds 26 4.3 Early responses lacked urgency and effectiveness 28 4.3.1 Successful countries were proactive, unsuccessful ones denied and delayed 31 4.3.2 The crisis in supplies 33 4.3.3 Lessons to be learnt from the early response 36 4.4 The failure to sustain the response in the face of the crisis 38 4.4.1 National health systems under enormous stress 38 4.4.2 Jobs at risk 38 4.4.3 Vaccine nationalism 41 5. -
CONNECTION the Official Newsletter of Zhejiang University Issue 16 Feb.2020
CONNECTION The Official Newsletter of Zhejiang University Issue 16 Feb.2020 COVID-19 Special Issue Stand Strong Message from Editor-in-Chief CONNECTION Welcome to the special COVID-19 issue of Issue 16 CONNECTION, which highlights the efforts and contributions of ZJU community in face of the epidemic. As a group, they are heroes in harm's way, givers and doers who respond swiftly to the need of our city, our country and the world. When you read their stories, you'll recognize the strength and solidarity that define all ZJUers. ZJU community has demonstrated its courage and resilience in the battle against the novel coronavirus. At this time, let us all come together to protect ourselves and our loved ones, keep all those who are at the front lines in our prayers and pass on our gratitude to those who have joined and contributed to the fight against the virus. Together, we will weather this crisis. LI Min, Editor-in-Chief Director, Office of Global Engagement Editorial office : Global Communications Office of Global Engagement, Zhejiang University 866 Yuhangtang Road, Hangzhou, P.R. China 310058 Phone: +86 571 88981259 Fax: +86 571 87951315 Email: [email protected] Edited by : CHEN Weiying, AI Ni Designed by : HUANG Zhaoyi Material from Connection may be reproduced accompanied with appropriate acknowledgement. CONTENTS Faculty One of the heroes in harm’s way: LI Lanjuan 03 ZJU medics answered the call from Wuhan 04 Insights from ZJU experts 05 Alumni Fund for Prevention and Control of Viral Infectious Diseases set up 10 Alumni community mobilized in the battle against COVID-19 11 Education Classes start online during the epidemic 15 What ZJUers feel about online learning 15 Efforts to address concerns, avoid misinformation 17 International World standing with us 18 International students lending a hand against the epidemic 20 What our fans say 21 FacultyFaculty ZJU community has taken on the responsibility to join the concertedZJU community efforts has takenagainst on thethe responsibility spreadto join the of concerted the virus. -
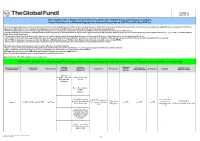
List of SARS-Cov-2 Diagnostic Test Kits and Equipments Eligible For
Version 33 2021-09-24 List of SARS-CoV-2 Diagnostic test kits and equipments eligible for procurement according to Board Decision on Additional Support for Country Responses to COVID-19 (GF/B42/EDP11) The following emergency procedures established by WHO and the Regulatory Authorities of the Founding Members of the GHTF have been identified by the QA Team and will be used to determine eligibility for procurement of COVID-19 diagnostics. The product, to be considered as eligible for procurement with GF resources, shall be listed in one of the below mentioned lists: - WHO Prequalification decisions made as per the Emergency Use Listing (EUL) procedure opened to candidate in vitro diagnostics (IVDs) to detect SARS-CoV-2; - The United States Food and Drug Administration’s (USFDA) general recommendations and procedures applicable to the authorization of the emergency use of certain medical products under sections 564, 564A, and 564B of the Federal Food, Drug, and Cosmetic Act; - The decisions taken based on the Canada’s Minister of Health interim order (IO) to expedite the review of these medical devices, including test kits used to diagnose COVID-19; - The COVID-19 diagnostic tests approved by the Therapeutic Goods Administration (TGA) for inclusion on the Australian Register of Therapeutic Goods (ARTG) on the basis of the Expedited TGA assessment - The COVID-19 diagnostic tests approved by the Ministry of Health, Labour and Welfare after March 2020 with prior scientific review by the PMDA - The COVID-19 diagnostic tests listed on the French -

Recommended Laboratory HIV Testing Algorithm for Serum Or Impact of HIV/AIDS
Journal of HIV for Clinical and Scientific Research eertechz Uğur Tüzüner*, Begüm Saran Gülcen Review article and Mehmet Özdemir Necmettin Erbakan University, Meram Medical Faculty, Medical Microbiology Department, Medical Virology Laboratory Algorithm in HIV Division. Konya, Turkey Dates: Received: 02 April, 2016; Accepted: 18 April, Infection Diagnosis 2016; Published: 19 April, 2016 *Corresponding author: Dr. Uğur Tüzüner, Abstract Necmettin Erbakan University, Meram Medical Faculty, Medical Microbiology Department, AIDS caused by HIV is an infection disease which was defined firstly in the USA in 1981. Since Konya, Turkey, Tel:+90 332 223 7029; E-mail: then, number of AIDS patients has increased continuously. About 36.9 million people are living with HIV around the world. Approximately 15 million people living with HIV were receiving antiretroviral therapy. Early detection is important due to the high risk of transmission that precedes seroconversion www.peertechz.com and also because it provides an opportunity to improve health outcomes with an early antiretroviral therapy. HIV testing is the key part of diagnosis and prevention efforts. Many tests have been used ISSN: 2455-3786 in the diagnosis of HIV over years and with developing testing methods, accuracy of the laboratory Keywords: HIV; Laboratory diagnosis; Algorithm diagnosis of HIV infection has been improved. Detecting p24 antigens, HIV 1-2 antibodies and HIV nucleic acid demonstrated that antibody testing alone might miss a considerable percentage of HIV infections detectable by these tests. This review provides updated recommendations and algorithm for HIV testing that are necessary for diagnosing HIV and offers approaches for accurate assessment of test results. Introduction HIV infection (asymptomatic HIV infection or clinical latency), and progression to AIDS (the late stage of HIV infection).