Ketamine for Pain Management Memory, and Synapticreceptor Plasticity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
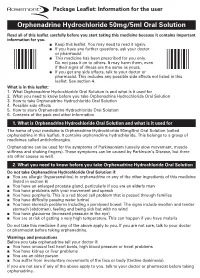
Orphenadrine Hydrochloride 50Mg/5Ml Oral Solution Rare (Affect More Than 1 in 10,000 People) N Forgetting Things More Than Usual
Uncommon (affect more than 1 in 1000 people) n Constipation Package Leaflet: Information for the user n Greater sensitivity to things around you or feeling nervous n Feeling light-headed and an unusual feeling of excitement (elation) n Difficulty sleeping or feeling tired. Orphenadrine Hydrochloride 50mg/5ml Oral Solution Rare (affect more than 1 in 10,000 people) n Forgetting things more than usual. Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Reporting of side effects n Keep this leaflet. You may need to read it again. If you get any side effects, talk to your doctor, n If you have any further questions, ask your doctor pharmacist or nurse. This includes any possible side or pharmacist. effects not listed in this leaflet. You can also report n This medicine has been prescribed for you only. side effects directly (see details below). By reporting Do not pass it on to others. It may harm them, even side effects you can help provide more information on if their signs of illness are the same as yours. the safety of this medicine. n If you get any side effects, talk to your doctor or United Kingdom pharmacist. This includes any possible side effects not listed in this Yellow Card Scheme leaflet. See section 4. Website: www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or What is in this leaflet: Apple App Store. 1. What Orphenadrine Hydrochloride Oral Solution is and what is it used for 2. -

Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

Prescription Regulations Summary Chart Who Hold an Approval to Prescribe Methadone from Their
Products included in the Triplicate Prescription Program* This is a reference list provided for convenience. While all generic medication names appear, only sample brand names are provided and it should not be viewed as an all-inclusive listing of all trade names of drugs included in the Triplicate Prescription Program. BUPRENORPHINE METHADONE BuTrans, Suboxone** Metadol, Methadose - May only be prescribed by physicians Prescription regulations summary chart who hold an approval to prescribe methadone from their BUTALBITAL PREPARATIONS provincial regulatory body*** Summary of federal and provincial laws governing prescription drug ordering, Fiorinal, Fiorinal C ¼ & C ½, Pronal, Ratio-Tecnal, records, prescription requirements, and refills Ratio-Tecnal C ¼ & C ½, Trianal, Trianal C ½ METHYLPHENIDATE Biphentin®, Foquest®, and Concerta® brands are excluded Revised 2019 BUTORPHANOL from TPP prescr ip t i o n p a d req u ir e m e n t s (generic versions Butorphanol NS, PMS-Butorphanol, Torbutrol (Vet), of these products require a triplicate presc ription) Torbugesic (Vet) Apo-Methyphenidate, PHL-Methylphenidate, PMS- Prescription regulations DEXTROPROPOXYPHENE Methylphenidate, PMS-Methylphenidate ER, Ratio- None identified Methylphenidate, Ritalin, Ritalin SR, Sandoz- According to the Standards of Practice for Pharmacists and Pharmacy Technicians: Methylphenidate SR, Teva-Methylphenidate ER-C FENTANYL/SUFENTANIL/ALFENTANIL 6.4 Neither a pharmacist nor a pharmacy technician may dispense a drug or blood product under a Alfentanil Injection, -

Choice of Drugs in the Treatment of Rheumatoid Arthritis
RHEUMATOLOGY IN GENERAL PRACTICE 7 Those with predominant but never exclusive involvement of the terminal finger joint, usually associated with changes in the nail of the same finger; they are serologically negative. There may be a swollen finger with loss of the skin markings-a sort of dactylitis, again serologically negative. (2) Those with a much more severe process which produces loss of movement in the spine and changes in the sacroiliac joints much the same as those in ankylosing spondylitis; unlike ankylosing spondylitis, it produces severe deformity often with ankylosis in peripheral joints. Many of the finger joints become deformed and ankylosed. (3) Those cases indistinguishable from rheumatoid arthritis although the majority are sero-negative. The Stevens Johnson syndrome produces acute effusions, particularly in large joints. It is sometimes associated with the rash of erythema multiforme, always with ulceration in the mouth and genital tract; the mouth ulcers are accompanied by sloughing, unlike those of Beh9et's syndrome which we come to next. BehCet's syndrome, originally described as a combination of orogenital ulceration with relapsing iritis, is now expanded to include skin lesions, other eye lesions, lesions of the central nervous system, thrombophlebitis migrans, and arthropathy (occurring in 64 per cent). The onset is acute, often affecting only a single joint and settling without residual trouble. Choice of drugs in the treatment of rheumatoid arthritis Dr Dudley Hart, M.D., F.R.C.P. (Consultant physician, Westminster Hospital and Medical School) There are many potential drugs for the treatment of rheumatoid disease, but what are we treating in this disorder? Pain in rheumatoid arthritis is but one of the symp- toms. -

Literature Review of Prescription Analgesics in the Causal Path to Pain
Literature Review: Opioids and Death compiled by Bill Stockdale ([email protected]) This review is the result of searches for the terms opioid/opioid-related-disorders and death/ADE done in the PubMed database. This bibliography includes selected articles from the 1,075 found by searching during May, 2008, which represent key findings in the study of opioids. Articles for which there is no abstract are excluded. Also case reports and initial clinical trial reports are excluded. This is a compendium of all articles and do not lead to a specific target. There are three major topics developed in the literature as shown in this table of contents; • Topic One: Opioids in Causal Path to Death (page 1) o Prescription Drug Deaths (page 1) o Illicit Drug Deaths (page 30) o Neonatal Deaths (page 49) • Topic Two: Deaths in Palliative Care and Pain Treatment (page 57) • Topic Three: Pharmacology, Psychology, Origins of Abuse Relating to Death (page 72) • Bibliography (page 77) The three topics are presented below; each is followed in chronological order. Topic One: Opioids in Causal Path to Death Prescription Drug Deaths Karlson et al. describe differences in treatment of acute myocardial infarction, including different opioid use among men and women. The question whether women and men with acute myocardial infarction (AMI) are treated differently is currently debated. In this analysis we compared pharmacological treatments and revascularization procedures during hospitalization and during 1 year of follow-up in 300 women and 621 men who suffered an AMI in 1986 or 1987 at our hospital. During hospitalization, the mean dose of morphine (+/- SD) during the first 3 days was higher in men compared to women (14.5 +/- 15.7 vs. -

PCF4 Revised Monographs (Since Publication September 2011 to July 2014)
www.palliativedrugs.com PCF4 revised monographs (since publication September 2011 to July 2014) Monograph Chapter number Date updated 5HT3 antagonists Chapter 04 Correction Apr-13 5HT3 antagonists Chapter 04 Jun-14 Adjuvant analgesics Chapter 05 Jun-14 Alfentanil Chapter 05 May-14 Amitriptyline Chapter 04 Oct-13 Anaemia Chapter 09 Apr-14 Analgesic drugs and fitness to drive Chapter 19 Jun-14 Anaphylaxis Chapter 27 May-13 Anaphylaxis Chapter 27 Correction Oct-13 Anaphylaxis Chapter 27 Jul-14 Antacids Chapter 01 Sep-12 Antacids Chapter 01 Minor update Jun-14 Antibacterials in palliative care Chapter 06 Sep-12 Antibacterials in palliative care Chapter 06 Minor update Apr-14 Anticoagulants Chapter 02 Minor update Aug-13 Anticoagulants (new) Chapter 02 New May-13 Antidepressants Chapter 04 Oct-13 Anti-emetics Chapter 04 Jun-14 Anti-epileptics pre-synaptic calcium channel blockers Chapter 04 Discontinued May-14 Anti-epileptics sodium channel blockers Chapter 04 Discontinued May-14 Anti-epileptics Chapter 04 Merged monograph May-14 Antifibrinolytics Chapter 02 Aug-13 Antihistaminic antimuscarinic anti-emetics Chapter 04 Jun-14 Antimuscarinics Chapter 01 Correction Apr-13 Antimuscarinics Chapter 01 Apr-14 Antipsychotics Chapter 04 Jun-14 Antitussives Chapter 03 Mar-14 Artificial saliva Chapter 11 Jun-14 Ascorbic acid Chapter 09 Nov-12 Baclofen Chapter 10 Jun-14 Barrier products Chapter 12 Apr-14 Benzodiazepines Chapter 04 Jun-14 Bisphosphonates Chapter 07 Merged monograph Jun-14 Buprenorphine Chapter 05 Jun-13 Buprenorphine Chapter 05 Jun-14 -

Chapter 151 – Antidepressants
Crack Cast Show Notes – Skin and Soft Tissue Infections www.canadiem.org Chapter 151 – Antidepressants Key Concepts ❏ Although rarely used for depression, MAOIs are used in the treatment of Parkinson’s disease ❏ Because serious symptoms can occur after a lengthy latent period, patients with reported MAOI overdose should be admitted for 24 hours, regardless of symptoms. Symptoms are characterized by tachycardia, hypertension, and CNS changes, and later cardiovascular collapse. ❏ The primary manifestations of TCA toxicity are seizures, tachycardia, and intraventricular conduction delay. IV sodium bicarbonate should be administered for QRS prolongation. ❏ DO NOT USE PHYSOSTIGMINE IN TCA OVERDOSE ❏ SSRIs are comparatively benign in overdose. ❏ SNRI ingestions can result in seizures, tachycardia, and occasionally intraventricular conduction delay. ❏ The hallmark feature of serotonin syndrome is lower extremity rigidity (spasticity) with spontaneous or inducible clonus, especially at the ankles. ❏ Serotonin syndrome is primarily treated with supportive care, including discontinuation of the offending agent, and benzodiazepines. Sign Post 1) List 7 pharmacodynamic effects of cyclic antidepressants and describe the physiologic result 2) What are the ECG findings associated with TCA toxicity and what are their implications 3) Describe the management of TCA toxicity 4) What are the diagnostic criteria for Serotonin Syndrome? 5) How can you discern between NMS and Serotonin Syndrome? 6) What are the common meds causing Serotonin Syndrome? 7) Describe the management of Serotonin Syndrome 8) What is the primary risk of toxicity in Bupropion? 9) What are the 3 mechanisms by which MAOI toxicity can occur? And what is the clinical syndrome? 10) List 5 foods and 5 classes of meds that can interact to cause MAOI toxicity 11) Describe the management of MAOI toxicity. -

NORFLEX™ Orphenadrine Citrate 100Mg Tablets
NORFLEX™ Orphenadrine citrate 100mg tablets Consumer Medicine Information What is in this leaflet Ask your doctor if you have any Before you start to take it questions about why this medicine Tell your doctor or pharmacist if This leaflet answers some common has been prescribed for you. • you have allergies to any other questions about NORFLEX tablets. medicines, foods, preservatives However it does not contain all the or dyes. available information. Your doctor and pharmacist have more Before you take • you have any heart problems. information about this medicine. NORFLEX • you have any liver or kidney If you have any questions about problems. NORFLEX that are not answered When you must not take it Tell your doctor if you are by this leaflet, please ask your Do not take NORFLEX if: pregnant or intend to become doctor or pharmacist. pregnant or you are breast-feeding • you have had an allergic or plan to breast-feed. All medicines have risks and reaction to orphenadrine citrate benefits. Your doctor has weighed or other similar medicines, or Your doctor or pharmacist can the risks of your taking NORFLEX to any of the ingredients listed discuss the risks and benefits against the benefits before at the end of this leaflet. involved. prescribing it for you. • you have any of the following: If you are not sure whether to start If you are worried about taking taking this medicine, talk to your - glaucoma this medicine please talk to your doctor. doctor or pharmacist. (high pressure in the eye); Keep this leaflet with your - intestinal blockage, stomach Taking other medicines medicine as you may want to read ulcer or oesophageal disease; Tell your doctor or pharmacist if it again. -
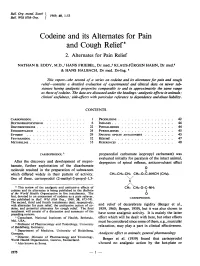
Codeine and Its Alternates for Pain and Cough Relief* 2
Bull. Org. mond. Sante Bull. Wid Hith Org. J 1969, 40. 1-53 Codeine and its Alternates for Pain and Cough Relief* 2. Alternates for Pain Relief NATHAN B. EDDY, M.D.,1 HANS FRIEBEL, Dr med.,2 KLAUS-J)RGEN HAHN, Dr med.3 & HANS HALBACH, Dr med. Dr-Ing. 4 This report-the second of a series on codeine and its alternates for pain and cough relief-contains a detailed evaluation of experimental and clinical data on newer sub- stances having analgesic properties comparable to and in approximately the same range as those ofcodeine. The data are discussed under the headings: analgesic effects in animals; clinical usefulness; side-effects with particular reference to dependence andabuse liability. CONTENTS CARISOPRODOL ............... 1 PRODILIDINE ........... ... .. 42 DEXTROPROPOXYPHENE ........... 6 INDANES .................. 44 DHYDROCODEINE ............... 22 PHTHALIMIDES ............... 44 ETHOHEPTAZINE ............... 24 PYRROLIDINES .......... .... 45 ETYMIDE.. .............. 29 SPECIFIC OPIATE ANTAGONISTS .... 45 FENYRAMIDOL ............... 32 Risum .................... 47 METOFOLINE. .............. 33 REFERENCES ............. ... 48 CARISOPRODOL 5 propanediol carbamate isopropyl carbamate) was evaluated initially for paralysis of the intact animal, After the discovery and development of mepro- depression of spinal reflexes, anticonvulsant effect bamate, further exploitation of the dicarbamate molecule resulted in the preparation of substances 0 which differed widely in their pattern of activity. CH3-CH2-CH2 CH2-O-C-NHCH (CH3)2 One of these, carisoprodol (2-methyl-2-propyl-1,3- \I/ c * This review of the analgesic and antitussive effects of CH3 CH2-0-C-NH2 codeine and its alternates is being published in the Bulletin of the World Health Organization in five instalments. The first, devoted to an assessment of codeine as a pain reliever, was published in Bull. -

Ensuring Adequate Access for Medical and Scientific Purposes
INTERNATIONAL NARCOTICS CONTROL BOARD Availability of Internationally Controlled Drugs Controlled Internationally of Availability Availability of Internationally Controlled Drugs: Ensuring Adequate Access for Medical and Scientific Purposes Indispensable, adequately available and not unduly restricted UNITED NATIONS Reports published by the International Narcotics Control Board in 2015 TheReport of the International Narcotics Control Board for 2015 (E/INCB/2015/1) is supple- mented by the following reports: Availability of Internationally Controlled Drugs: Ensuring Adequate Access for Medical and Scientific Purposes. Indispensable, adequately available and not unduly restricted (E/INCB/2015/1/Supp.1) Narcotic Drugs: Estimated World Requirements for 2016—Statistics for 2014 (E/INCB/2015/2) Psychotropic Substances: Statistics for 2014—Assessments of Annual Medical and Scientific Requirements for Substances in Schedules II, III and IV of the Convention on Psychotropic Substances of 1971 (E/INCB/2015/3) Precursors and Chemicals Frequently Used in the Illicit Manufacture of Narcotic Drugs and Psychotropic Substances: Report of the International Narcotics Control Board for 2014 on the Implementation of Article 12 of the United Nations Convention against Illicit Traffic in Narcotic Drugs and Psychotropic Substances of 1988 (E/INCB/2015/4) The updated lists of substances under international control, comprising narcotic drugs, psychotropic substances and substances frequently used in the illicit manufacture of narcotic drugs and psychotropic substances, are contained in the latest editions of the annexes to the statistical forms (“Yellow List”, “Green List” and “Red List”), which are also issued by the Board. Contacting the International Narcotics Control Board The secretariat of the Board may be reached at the following address: Vienna International Centre Room E-1339 P.O. -

NCT02523690 IRB00072940 Evaluating Muscle
NCT02523690 IRB00072940 Evaluating Muscle Weakness Improvement With Lorcaserin in ICU (EMILI) Protocol Version: February 10, 2017 (Date in header of protocol, 8/1/2016 was inadvertently not updated) Date: 1 August 2016 Principal Investigator: Dale Needham, MD PhD Application Number: IRB00072940 JHM IRB - eForm A – Protocol Use the section headings to write the JHM IRB eForm A, inserting the appropriate material in each. If a section is not applicable, leave heading in and insert N/A. When submitting JHM IRB eForm A (new or revised), enter the date submitted to the field at the top of JHM IRB eForm A. *************************************************************************************************** 1) Abstract (Provide no more than a one page research abstract briefly stating the problem, the research hypothesis, and the importance of the research.) It was recently discovery that patients recovering from sepsis/critical illness have great difficulty recruiting motor units to generate muscle force. Prior to this discovery, the primary etiology of muscle weakness in these patients was thought to be muscle disease (myopathy) and degeneration of peripheral nerve (neuropathy). However, since motor units are composed of a group of muscle fibers contacted by a single motor neuron arising from the spinal cord, these new findings suggested a problem within the spinal cord as the primary cause of weakness in affected patients. Consistent with these clinical findings in critically ill patients, there is a profound deficit in the excitability of motor neurons in the spinal cord of septic rats. Studies characterizing the impaired excitability in rat motor neurons point to a specific deficit in a slowly inactivating type of sodium current (i.e., the persistent sodium current). -

ESTIMATED WORLD REQUIREMENTS of NARCOTIC DRUGS in GRAMS for 2013 (January Update)
ESTIMATED WORLD REQUIREMENTS OF NARCOTIC DRUGS IN GRAMS FOR 2013 (January update) Afghanistan Oxycodone 43 000 Codeine 50 000 Oxymorphone 300 Dextropropoxyphene 2 000 000 Pethidine 65 000 Diphenoxylate 20 000 Remifentanil 9 100 Fentanyl 6 Sufentanil 1 Methadone 6 000 Thebaine 45 000 Morphine 4 000 Armenia Pethidine 80 000 Codeine 3 000 Pholcodine 100 000 Fentanyl 21 Albania Methadone 10 000 Codeine 35 000 Morphine 4 500 Fentanyl 40 Thebaine 10 Methadone 9 000 Trimeperidine 650 Morphine 3 000 Aruba* Pethidine 2 500 Alfentanil 3 Pholcodine 1 000 Bezitramide 1 Remifentanil 8 Cocaine 70 Sufentanil 1 Codeine 85 Algeria Dextromoramide 1 Alfentanil 500 Dextropropoxyphene 85 Codeine 1 000 000 Fentanyl 130 Etorphine 1 Hydrocodone 2 Fentanyl 1 000 Methadone 150 Morphine 11 000 Morphine 340 Pethidine 3 000 Opium 450 Pholcodine 2 500 000 Oxycodone 26 Sufentanil 30 Pethidine 404 Andorra Piritramide 20 Fentanyl 80 Remifentanil 19 Methadone 1 000 Ascension Island Morphine 500 Alfentanil 1 Oxycodone 1 500 Fentanyl 1 Pethidine 500 Morphine 2 Remifentanil 4 Pethidine 9 Angola* Australia Alfentanil 2 Alfentanil 400 Codeine 30 000 Cannabis 21 500 Dextromoramide 375 Cocaine 20 000 Dihydrocodeine 375 Codeine 9 800 000 Fentanyl 45 Conc. of poppy straw Morphine 11 000 AOA 4 000 000 Pethidine 13 000 ATA 85 000 000 Sufentanil 2 Dextromoramide 10 Anguilla Dextropropoxyphene 1 925 000 Fentanyl 1 Difenoxin 7 Morphine 20 Dihydrocodeine 285 000 Pethidine 300 Diphenoxylate 80 000 Antigua and Barbuda* Ethylmorphine 10 Cocaine 9 Etorphine 2 Codeine 169 Fentanyl 40 000