Risk Based Requirements for Medicines Handling
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of Status Epilepticus
Published online: 2019-11-21 THIEME Review Article 267 Management of Status Epilepticus Ritesh Lamsal1 Navindra R. Bista1 1Department of Anaesthesiology, Tribhuvan University Teaching Address for correspondence Ritesh Lamsal, MD, DM, Department Hospital, Institute of Medicine, Tribhuvan University, Nepal of Anaesthesiology, Tribhuvan University Teaching Hospital, Institute of Medicine, Tribhuvan University,Kathmandu, Nepal (e-mail: [email protected]). J Neuroanaesthesiol Crit Care 2019;6:267–274 Abstract Status epilepticus (SE) is a life-threatening neurologic condition that requires imme- diate assessment and intervention. Over the past few decades, the duration of seizure Keywords required to define status epilepticus has shortened, reflecting the need to start thera- ► convulsive status py without the slightest delay. The focus of this review is on the management of con- epilepticus vulsive and nonconvulsive status epilepticus in critically ill patients. Initial treatment ► neurocritical care of both forms of status epilepticus includes immediate assessment and stabilization, ► nonconvulsive status and administration of rapidly acting benzodiazepine therapy followed by nonbenzodi- epilepticus azepine antiepileptic drug. Refractory and super-refractory status epilepticus (RSE and ► refractory status SRSE) pose a lot of therapeutic problems, necessitating the administration of contin- epilepticus uous infusion of high doses of anesthetic agents, and carry a high risk of debilitating ► status epilepticus morbidity as well as mortality. ► super-refractory sta- tus epilepticus Introduction occur after 30 minutes of seizure activity. However, this working definition did not indicate the need to immediately Status epilepticus (SE) is a medical and neurologic emergency commence treatment and that permanent neuronal injury that requires immediate evaluation and treatment. It is associat- could occur by the time a clinical diagnosis of SE was made. -
Orphenadrine Hydrochloride 50Mg/5Ml Oral Solution Rare (Affect More Than 1 in 10,000 People) N Forgetting Things More Than Usual
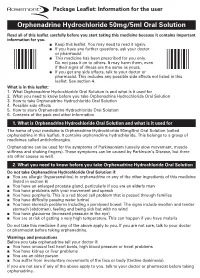
Uncommon (affect more than 1 in 1000 people) n Constipation Package Leaflet: Information for the user n Greater sensitivity to things around you or feeling nervous n Feeling light-headed and an unusual feeling of excitement (elation) n Difficulty sleeping or feeling tired. Orphenadrine Hydrochloride 50mg/5ml Oral Solution Rare (affect more than 1 in 10,000 people) n Forgetting things more than usual. Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Reporting of side effects n Keep this leaflet. You may need to read it again. If you get any side effects, talk to your doctor, n If you have any further questions, ask your doctor pharmacist or nurse. This includes any possible side or pharmacist. effects not listed in this leaflet. You can also report n This medicine has been prescribed for you only. side effects directly (see details below). By reporting Do not pass it on to others. It may harm them, even side effects you can help provide more information on if their signs of illness are the same as yours. the safety of this medicine. n If you get any side effects, talk to your doctor or United Kingdom pharmacist. This includes any possible side effects not listed in this Yellow Card Scheme leaflet. See section 4. Website: www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or What is in this leaflet: Apple App Store. 1. What Orphenadrine Hydrochloride Oral Solution is and what is it used for 2. -

Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW
Guideline Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW Summary To provide the most up-to-date knowledge and current level of best practice for the treatment of withdrawal from alcohol and other drugs such as heroin, and other opioids, benzodiazepines, cannabis and psychostimulants. Document type Guideline Document number GL2008_011 Publication date 04 July 2008 Author branch Centre for Alcohol and Other Drugs Branch contact (02) 9424 5938 Review date 18 April 2018 Policy manual Not applicable File number 04/2766 Previous reference N/A Status Active Functional group Clinical/Patient Services - Pharmaceutical, Medical Treatment Population Health - Pharmaceutical Applies to Area Health Services/Chief Executive Governed Statutory Health Corporation, Board Governed Statutory Health Corporations, Affiliated Health Organisations, Affiliated Health Organisations - Declared Distributed to Public Health System, Ministry of Health, Public Hospitals Audience All groups of health care workers;particularly prescribers of opioid treatments Secretary, NSW Health Guideline Ministry of Health, NSW 73 Miller Street North Sydney NSW 2060 Locked Mail Bag 961 North Sydney NSW 2059 Telephone (02) 9391 9000 Fax (02) 9391 9101 http://www.health.nsw.gov.au/policies/ space space Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW space Document Number GL2008_011 Publication date 04-Jul-2008 Functional Sub group Clinical/ Patient Services - Pharmaceutical Clinical/ Patient Services - Medical Treatment Population Health - Pharmaceutical -

Understanding Benzodiazephine Use, Abuse, and Detection
Siemens Healthcare Diagnostics, the leading clinical diagnostics company, is committed to providing clinicians with the vital information they need for the accurate diagnosis, treatment and monitoring of patients. Our comprehensive portfolio of performance-driven systems, unmatched menu offering and IT solutions, in conjunction with highly responsive service, is designed to streamline workflow, enhance operational efficiency and support improved patient care. Syva, EMIT, EMIT II, EMIT d.a.u., and all associated marks are trademarks of General Siemens Healthcare Diagnostics Inc. All Drugs other trademarks and brands are the Global Division property of their respective owners. of Abuse Siemens Healthcare Product availability may vary from Diagnostics Inc. country to country and is subject 1717 Deerfield Road to varying regulatory requirements. Deerfield, IL 60015-0778 Please contact your local USA representative for availability. www.siemens.com/diagnostics Siemens Global Headquarters Global Siemens Healthcare Headquarters Siemens AG Understanding Wittelsbacherplatz 2 Siemens AG 80333 Muenchen Healthcare Sector Germany Henkestrasse 127 Benzodiazephine Use, 91052 Erlangen Germany Abuse, and Detection Telephone: +49 9131 84 - 0 www.siemens.com/healthcare www.usa.siemens.com/diagnostics Answers for life. Order No. A91DX-0701526-UC1-4A00 | Printed in USA | © 2009 Siemens Healthcare Diagnostics Inc. Syva has been R1 R2 a leading developer N and manufacturer of AB R3 X N drugs-of-abuse tests R4 for more than 30 years. R2 C Now part of Siemens Healthcare ® Diagnostics, Syva boasts a long and Benzodiazepines have as their basic chemical structure successful track record in drugs-of-abuse a benzene ring fused to a seven-membered diazepine ring. testing, and leads the industry in the All important benzodiazepines contain a 5-aryl substituent ring (ring C) and a 1,4–diazepine ring. -

Retention Behaviour of Some Benzodiazepines in Solid-Phase Extraction Using Modified Silica Adsorbents Having Various Hydrophobicities
ACADEMIA ROMÂNĂ Rev. Roum. Chim., Revue Roumaine de Chimie 2015, 60(9), 891-898 http://web.icf.ro/rrch/ RETENTION BEHAVIOUR OF SOME BENZODIAZEPINES IN SOLID-PHASE EXTRACTION USING MODIFIED SILICA ADSORBENTS HAVING VARIOUS HYDROPHOBICITIES Elena BACALUM,a Mihaela CHEREGIb,* and Victor DAVIDb,* a Research Institute from University of Bucharest – ICUB, 36-46 M. Kogalniceanu Blvd., Bucharest, 050107, Roumania b University of Bucharest, Faculty of Chemistry, Department of Analytical Chemistry, 90 Panduri Ave, Bucharest – 050663, Roumania Received April 6, 2015 The retention properties of six benzodiazepines (alprazolam, bromazepam, diazepam, flunitrazepam, medazepam, and nitrazepam) on four different solid phase extraction silica 1.0 adsorbents with various hydrophobicities (octadecylsilica, octylsilica, phenylsilica, and cyanopropylsilica) were 0.8 H O investigated. The breakthrough curves showed a significant N retention of these compounds on octadecylsilica, octylsilica, 0.6 Br N phenylsilica, excepting alprazolam that has a poor retention on 0 C/C N octadecylsilica. These results can be explained by the 0.4 PHENYL CN hydrophobic character of studied benzodiazepines (octanol- C18 0.2 C8 Bromazepam water partition constant, log Kow, being situated within the interval 1.90-4.45). A poor retention on cyanopropylsilica was 0.0 observed for all studied compounds indicating that π-π and 0 102030405060708090100 Volume (mL) polar intermolecular interactions have a less significant role in their retention on this adsorbent. Generally, the breakthrough -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Benzodiazepines
Benzodiazepines Using benzodiazepines in Children and Adolescents Overview Benzodiazepines are group of medications used to treat several different conditions. Some examples of these medications include: lorazepam (Ativan®); clonazepam (Rivotril®); alprazolam (Xanax®) and oxazepam (Serax®). Other benzodiazepine medications are available, but are less commonly used in children and adolescents. What are benzodiazepines used for? Benzodiazepines may be used for the following conditions: • anxiety disorders: generalized anxiety disorder; social anxiety disorder; post-traumatic stress disorder (PTSD); panic attacks/disorder; excessive anxiety prior to surgery • sleep disorders: trouble sleeping (insomnia); waking up suddenly with great fear (night terrors); sleepwalking • seizure disorders (epilepsy) • alcohol withdrawal • treatment of periods of extreme slowing or excessive purposeless motor activity (catatonia) Your doctor may be using this medication for another reason. If you are unclear why this medication is being prescribed, please ask your doctor. How do benzodiazepines work? Benzodiazepines works by affecting the activity of the brain chemical (neurotransmitter) called GABA. By enhancing the action of GABA, benzodiazepines have a calming effect on parts of the brain that are too excitable. This in turn helps to manage anxiety, insomnia, and seizure disorders. How well do benzodiazepines work in children and adolescents? When used to treat anxiety disorders, benzodiazepines decrease symptoms such as nervousness, fear, and excessive worrying. Benzodiazepines may also help with the physical symptoms of anxiety, including fast or strong heart beat, trouble breathing, dizziness, shakiness, sweating, and restlessness. Typically, benzodiazepines are prescribed to manage anxiety symptoms that are uncomfortable, frightening or interfere with daily activities for a short period of time before conventional anti-anxiety treatments like cognitive-behavioural therapy or anti-anxiety takes effect. -

Neonatal Clonazepam Administration Induced Long-Lasting Changes in GABAA and GABAB Receptors
International Journal of Molecular Sciences Article Neonatal Clonazepam Administration Induced Long-Lasting Changes in GABAA and GABAB Receptors Hana Kubová 1,* , Zde ˇnkaBendová 2,3 , Simona Moravcová 2,3 , Dominika Paˇcesová 2,3, Luisa Rocha 4 and Pavel Mareš 1 1 Institute of Physiology, Academy of Sciences of the Czech Republic, 14220 Prague, Czech Republic; [email protected] 2 Faculty of Science, Charles University, 12800 Prague, Czech Republic; [email protected] (Z.B.); [email protected] (S.M.); [email protected] (D.P.) 3 National Institute of Mental Health, 25067 Klecany, Czech Republic 4 Pharmacobiology Department, Center of Research and Advanced Studies, Mexico City 14330, Mexico; [email protected] * Correspondence: [email protected]; Tel.: +420-2-4106-2565 Received: 31 March 2020; Accepted: 28 April 2020; Published: 30 April 2020 Abstract: Benzodiazepines (BZDs) are widely used in patients of all ages. Unlike adults, neonatal animals treated with BZDs exhibit a variety of behavioral deficits later in life; however, the mechanisms underlying these deficits are poorly understood. This study aims to examine whether administration of clonazepam (CZP; 1 mg/kg/day) in 7–11-day-old rats affects Gama aminobutyric acid (GABA)ergic receptors in both the short and long terms. Using RT-PCR and quantitative autoradiography, we examined the expression of the selected GABAA receptor subunits (α1, α2, α4, γ2, and δ) and the GABAB B2 subunit, and GABAA, benzodiazepine, and GABAB receptor binding 48 h, 1 week, and 2 months after treatment discontinuation. Within one week after CZP cessation, the expression of the α2 subunit was upregulated, whereas that of the δ subunit was downregulated in both the hippocampus and cortex. -

Prescription Regulations Summary Chart Who Hold an Approval to Prescribe Methadone from Their
Products included in the Triplicate Prescription Program* This is a reference list provided for convenience. While all generic medication names appear, only sample brand names are provided and it should not be viewed as an all-inclusive listing of all trade names of drugs included in the Triplicate Prescription Program. BUPRENORPHINE METHADONE BuTrans, Suboxone** Metadol, Methadose - May only be prescribed by physicians Prescription regulations summary chart who hold an approval to prescribe methadone from their BUTALBITAL PREPARATIONS provincial regulatory body*** Summary of federal and provincial laws governing prescription drug ordering, Fiorinal, Fiorinal C ¼ & C ½, Pronal, Ratio-Tecnal, records, prescription requirements, and refills Ratio-Tecnal C ¼ & C ½, Trianal, Trianal C ½ METHYLPHENIDATE Biphentin®, Foquest®, and Concerta® brands are excluded Revised 2019 BUTORPHANOL from TPP prescr ip t i o n p a d req u ir e m e n t s (generic versions Butorphanol NS, PMS-Butorphanol, Torbutrol (Vet), of these products require a triplicate presc ription) Torbugesic (Vet) Apo-Methyphenidate, PHL-Methylphenidate, PMS- Prescription regulations DEXTROPROPOXYPHENE Methylphenidate, PMS-Methylphenidate ER, Ratio- None identified Methylphenidate, Ritalin, Ritalin SR, Sandoz- According to the Standards of Practice for Pharmacists and Pharmacy Technicians: Methylphenidate SR, Teva-Methylphenidate ER-C FENTANYL/SUFENTANIL/ALFENTANIL 6.4 Neither a pharmacist nor a pharmacy technician may dispense a drug or blood product under a Alfentanil Injection, -

Pentameric Ligand-Gated Ion Channel ELIC Is Activated by GABA And
Pentameric ligand-gated ion channel ELIC is activated PNAS PLUS by GABA and modulated by benzodiazepines Radovan Spurnya, Joachim Ramerstorferb, Kerry Pricec, Marijke Bramsa, Margot Ernstb, Hugues Nuryd, Mark Verheije, Pierre Legrandf, Daniel Bertrandg, Sonia Bertrandg, Dennis A. Doughertyh, Iwan J. P. de Esche, Pierre-Jean Corringerd, Werner Sieghartb, Sarah C. R. Lummisc, and Chris Ulensa,1 aDepartment of Cellular and Molecular Medicine, Laboratory of Structural Neurobiology, Catholic University of Leuven, 3000 Leuven, Belgium; bDepartment of Biochemistry and Molecular Biology of the Nervous System, Medical University of Vienna, A-1090 Vienna, Austria; cDepartment of Biochemistry, University of Cambridge, Cambridge CB2 1QW, United Kingdom; dPasteur Institute, G5 Group of Channel-Receptor, Centre National de la Recherche Scientifique, 75724 Paris, France; eDepartment of Medicinal Chemistry, VU University Amsterdam, 1081 HV, Amsterdam, The Netherlands; fSOLEIL Synchrotron, 91192 Gif sur Yvette, France; gHiQScreen, CH-1211 Geneva, Switzerland; and hCalifornia Institute of Technology, Pasadena, CA 91125 Edited* by Jean-Pierre Changeux, Institut Pasteur, Paris Cedex 15, France, and approved September 10, 2012 (received for review May 24, 2012) GABAA receptors are pentameric ligand-gated ion channels in- marized in SI Appendix, Table S1). In addition, it has been volved in fast inhibitory neurotransmission and are allosterically suggested that the GABA carboxylate group is stabilized through modulated by the anxiolytic, anticonvulsant, and sedative-hypnotic electrostatic interactions with Arg residues on the principal and benzodiazepines. Here we show that the prokaryotic homolog ELIC complementary faces of the binding site (4, 7–9). For benzo- also is activated by GABA and is modulated by benzodiazepines diazepines, the individual contributions of residues in loops A–F with effects comparable to those at GABAA receptors. -

Choice of Drugs in the Treatment of Rheumatoid Arthritis
RHEUMATOLOGY IN GENERAL PRACTICE 7 Those with predominant but never exclusive involvement of the terminal finger joint, usually associated with changes in the nail of the same finger; they are serologically negative. There may be a swollen finger with loss of the skin markings-a sort of dactylitis, again serologically negative. (2) Those with a much more severe process which produces loss of movement in the spine and changes in the sacroiliac joints much the same as those in ankylosing spondylitis; unlike ankylosing spondylitis, it produces severe deformity often with ankylosis in peripheral joints. Many of the finger joints become deformed and ankylosed. (3) Those cases indistinguishable from rheumatoid arthritis although the majority are sero-negative. The Stevens Johnson syndrome produces acute effusions, particularly in large joints. It is sometimes associated with the rash of erythema multiforme, always with ulceration in the mouth and genital tract; the mouth ulcers are accompanied by sloughing, unlike those of Beh9et's syndrome which we come to next. BehCet's syndrome, originally described as a combination of orogenital ulceration with relapsing iritis, is now expanded to include skin lesions, other eye lesions, lesions of the central nervous system, thrombophlebitis migrans, and arthropathy (occurring in 64 per cent). The onset is acute, often affecting only a single joint and settling without residual trouble. Choice of drugs in the treatment of rheumatoid arthritis Dr Dudley Hart, M.D., F.R.C.P. (Consultant physician, Westminster Hospital and Medical School) There are many potential drugs for the treatment of rheumatoid disease, but what are we treating in this disorder? Pain in rheumatoid arthritis is but one of the symp- toms. -

KLONOPIN(R) Tablets (1.0 Mg)
Safety Data Sheet KLONOPIN(R) Tablets (1.0 mg) SECTION 1: Identification of the substance/mixture and of the company/undertaking 1.1. Product identifier Product name KLONOPIN(R) Tablets (1.0 mg) Product code SAP-10065806 1.2. Relevant identified uses of the substance or mixture and uses advised against Use - pharmaceutical active substance (anti-epileptic drug) *1 1.3. Details of the supplier of the safety data sheet Company information Enquiries: Local representation: Genentech, Inc. 1 DNA Way South San Francisco USA-CA 94080 United States of America Phone 001-(650) 225-1000 E-Mail [email protected] US Chemtrec phone: (800)-424-9300 1.4. Emergency telephone number Emergency telephone number US Chemtrec phone: (800)-424-9300 *1 referring to: Clonazepam SECTION 2: Hazards identification Classification of the substance or mixture / Label elements GHS Classification no classification and labelling according to GHS Other hazards Note - Benzodiazepines induce central nervous system depression and drowsiness. In addition, longer use may be habit forming. Hence, these compounds are also misused by addicts. *1 *1 referring to: Clonazepam Date: 30.4.15/LS (SEISMO) Replacing edition of: -- Page: 1/8 KLONOPIN(R) Tablets (1.0 mg) SECTION 3: Composition/information on ingredients Characterization mixture of 0.6% Clonazepam with excipients Ingredients Concentration Clonazepam - Combustible dust (No category), USH003 1622-61-3 0.6 % Corn starch 9005-25-8 11.8 % Microcrystalline cellulose 9004-34-6 14.7 % For the full text of the H-phrases mentioned in this Section, see Section 16. SECTION 4: First aid measures 4.1. Description of first aid measures Eye contact - rinse immediately with tap water for 10 minutes - open eyelids forcibly Skin contact - drench affected skin with plenty of water Inhalation - remove the casualty to fresh air - in the event of symptoms get medical treatment 4.2.