Role of Medication and Background Variables
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Examination of the Complex Pharmacological Properties of the Non-Selective Opioid Receptor Modulator Buprenorphine Leana J. P
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 17 November 2020 doi:10.20944/preprints202011.0443.v1 An Examination of the Complex Pharmacological Properties of the Non-Selective Opioid Receptor Modulator Buprenorphine Leana J. Pande1, Brian J. Piper1,2* 1Department of Medical Education, Geisinger Commonwealth School of Medicine 2Center for Pharmacy Innovation and Outcomes * Brian J. Piper, Ph.D.525 Pine Street, Geisinger Commonwealth School of Medicine Scranton, PA 18411, USA Abstract: Buprenorphine, an analogue of thebaine, is a Schedule III opioid in the United States used for opioid-use disorder and as an analgesic. Research has shown drugs like buprenorphine have a complicated pharmacology with characteristics that challenge traditional definitions of terms like agonist, antagonist, and efficacy. Buprenorphine has a high affinity for the mu (MOR), delta (DOR), kappa (KOR), and intermediate for the nociceptin opioid receptors (NOR). Buprenorphine is generally described as a partial MOR agonist with limited activity and decreased response at the mu- receptor relative to full agonists. In opioid naïve patients, the drug’s analgesic efficacy is equivalent to a full MOR agonist, despite decreased receptor occupancy and the “ceiling effect” produced from larger doses. Some argue buprenorphine’s effects depend on the endpoint measured, as it functions as a partial agonist for respiratory depression, but a full-agonist for pain. Buprenorphine’s active metabolite, norbuprenorphine, attenuates buprenorphine's analgesic effects due to NOR binding and respiratory depressant effects. The method of administration impacts efficacy and tolerance when administered for analgesia. There have been eleven-thousand reports involving buprenorphine and minors (age < 19) to US poison control centers, the preponderance (89.2%) with children. -
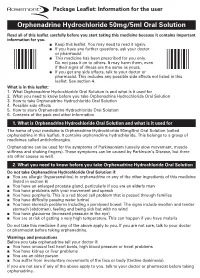
Orphenadrine Hydrochloride 50Mg/5Ml Oral Solution Rare (Affect More Than 1 in 10,000 People) N Forgetting Things More Than Usual
Uncommon (affect more than 1 in 1000 people) n Constipation Package Leaflet: Information for the user n Greater sensitivity to things around you or feeling nervous n Feeling light-headed and an unusual feeling of excitement (elation) n Difficulty sleeping or feeling tired. Orphenadrine Hydrochloride 50mg/5ml Oral Solution Rare (affect more than 1 in 10,000 people) n Forgetting things more than usual. Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Reporting of side effects n Keep this leaflet. You may need to read it again. If you get any side effects, talk to your doctor, n If you have any further questions, ask your doctor pharmacist or nurse. This includes any possible side or pharmacist. effects not listed in this leaflet. You can also report n This medicine has been prescribed for you only. side effects directly (see details below). By reporting Do not pass it on to others. It may harm them, even side effects you can help provide more information on if their signs of illness are the same as yours. the safety of this medicine. n If you get any side effects, talk to your doctor or United Kingdom pharmacist. This includes any possible side effects not listed in this Yellow Card Scheme leaflet. See section 4. Website: www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or What is in this leaflet: Apple App Store. 1. What Orphenadrine Hydrochloride Oral Solution is and what is it used for 2. -

Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

Use of Analgesics in Exotic Felids Edward C. Ramsay, DVM Professor, Department of Small Animal Clinical Sciences, University Of
Use of Analgesics in Exotic Felids Formatted: Centered Edward C. Ramsay, DVM Professor, Department of Small Animal Clinical Sciences, University of Tennessee, and Consulting Veterinarian, Knoxville Zoological Gardens, Knoxville, Tennessee. Corresponding address: Ed Ramsay Dept. of Sm Animal Clin Sci C247, Veterinary Teaching Hospital University of Tennessee Knoxville, TN 37996-4544 Phone: 865-755-8219 FAX: 865-974-5554 Email: [email protected] 2 Treatment of pain in domestic and non-domestic cats has been a challenge for the clinician. Many cat species are stoic and show few or very subtle external signs of pain. Additionally, the adverse effects of nonsteroidal antiinflammatory drugs (NSAIDs) in domestic cats are well documented and have discouraged many practitioners from trying novel NSAID’s in exotic felids. As in other animals, each cat’s response to pain and analgesics will vary, necessitating an individualized treatment plan. As a rule, always treat painful felids to effect, and not by rote reliance on published dosages. It is frequently necessary to try different agents and combinations to find which produces the optimal analgesic effect in exotic felids. In order to minimize adverse effects, it is desirable to work toward treatment with the lowest effective dose when treating chronic pain. Non-steroidal Antiinflammatory Drugs NSAIDs are antiinflammatory drugs which act both centrally and peripherally. The primary effects are believed to be caused by their ability to inhibit cyclooxygenase (COX) enzymes in the arachidonic acid metabolism cascade. The COX-1 isoform is regarded as constitutive (continuously expressed) and is responsible for many homeostatic processes, such as maintenance of gastric mucosal integrity, platelet function, and renal autoregulation. -

Prescription Regulations Summary Chart Who Hold an Approval to Prescribe Methadone from Their
Products included in the Triplicate Prescription Program* This is a reference list provided for convenience. While all generic medication names appear, only sample brand names are provided and it should not be viewed as an all-inclusive listing of all trade names of drugs included in the Triplicate Prescription Program. BUPRENORPHINE METHADONE BuTrans, Suboxone** Metadol, Methadose - May only be prescribed by physicians Prescription regulations summary chart who hold an approval to prescribe methadone from their BUTALBITAL PREPARATIONS provincial regulatory body*** Summary of federal and provincial laws governing prescription drug ordering, Fiorinal, Fiorinal C ¼ & C ½, Pronal, Ratio-Tecnal, records, prescription requirements, and refills Ratio-Tecnal C ¼ & C ½, Trianal, Trianal C ½ METHYLPHENIDATE Biphentin®, Foquest®, and Concerta® brands are excluded Revised 2019 BUTORPHANOL from TPP prescr ip t i o n p a d req u ir e m e n t s (generic versions Butorphanol NS, PMS-Butorphanol, Torbutrol (Vet), of these products require a triplicate presc ription) Torbugesic (Vet) Apo-Methyphenidate, PHL-Methylphenidate, PMS- Prescription regulations DEXTROPROPOXYPHENE Methylphenidate, PMS-Methylphenidate ER, Ratio- None identified Methylphenidate, Ritalin, Ritalin SR, Sandoz- According to the Standards of Practice for Pharmacists and Pharmacy Technicians: Methylphenidate SR, Teva-Methylphenidate ER-C FENTANYL/SUFENTANIL/ALFENTANIL 6.4 Neither a pharmacist nor a pharmacy technician may dispense a drug or blood product under a Alfentanil Injection, -

Choice of Drugs in the Treatment of Rheumatoid Arthritis
RHEUMATOLOGY IN GENERAL PRACTICE 7 Those with predominant but never exclusive involvement of the terminal finger joint, usually associated with changes in the nail of the same finger; they are serologically negative. There may be a swollen finger with loss of the skin markings-a sort of dactylitis, again serologically negative. (2) Those with a much more severe process which produces loss of movement in the spine and changes in the sacroiliac joints much the same as those in ankylosing spondylitis; unlike ankylosing spondylitis, it produces severe deformity often with ankylosis in peripheral joints. Many of the finger joints become deformed and ankylosed. (3) Those cases indistinguishable from rheumatoid arthritis although the majority are sero-negative. The Stevens Johnson syndrome produces acute effusions, particularly in large joints. It is sometimes associated with the rash of erythema multiforme, always with ulceration in the mouth and genital tract; the mouth ulcers are accompanied by sloughing, unlike those of Beh9et's syndrome which we come to next. BehCet's syndrome, originally described as a combination of orogenital ulceration with relapsing iritis, is now expanded to include skin lesions, other eye lesions, lesions of the central nervous system, thrombophlebitis migrans, and arthropathy (occurring in 64 per cent). The onset is acute, often affecting only a single joint and settling without residual trouble. Choice of drugs in the treatment of rheumatoid arthritis Dr Dudley Hart, M.D., F.R.C.P. (Consultant physician, Westminster Hospital and Medical School) There are many potential drugs for the treatment of rheumatoid disease, but what are we treating in this disorder? Pain in rheumatoid arthritis is but one of the symp- toms. -

Literature Review of Prescription Analgesics in the Causal Path to Pain
Literature Review: Opioids and Death compiled by Bill Stockdale ([email protected]) This review is the result of searches for the terms opioid/opioid-related-disorders and death/ADE done in the PubMed database. This bibliography includes selected articles from the 1,075 found by searching during May, 2008, which represent key findings in the study of opioids. Articles for which there is no abstract are excluded. Also case reports and initial clinical trial reports are excluded. This is a compendium of all articles and do not lead to a specific target. There are three major topics developed in the literature as shown in this table of contents; • Topic One: Opioids in Causal Path to Death (page 1) o Prescription Drug Deaths (page 1) o Illicit Drug Deaths (page 30) o Neonatal Deaths (page 49) • Topic Two: Deaths in Palliative Care and Pain Treatment (page 57) • Topic Three: Pharmacology, Psychology, Origins of Abuse Relating to Death (page 72) • Bibliography (page 77) The three topics are presented below; each is followed in chronological order. Topic One: Opioids in Causal Path to Death Prescription Drug Deaths Karlson et al. describe differences in treatment of acute myocardial infarction, including different opioid use among men and women. The question whether women and men with acute myocardial infarction (AMI) are treated differently is currently debated. In this analysis we compared pharmacological treatments and revascularization procedures during hospitalization and during 1 year of follow-up in 300 women and 621 men who suffered an AMI in 1986 or 1987 at our hospital. During hospitalization, the mean dose of morphine (+/- SD) during the first 3 days was higher in men compared to women (14.5 +/- 15.7 vs. -

Integrating Buprenorphine Treatment for Opioid Use Disorder in HIV Primary Care
Integrating Buprenorphine Treatment for Opioid Use Disorder in HIV Primary Care Michael MacVeigh, MD K r i st en Meyer s, BS, C A D C 1 May 10-12, 2017 Por t land Our Clinic Building Overview • W elcome Back and Overview of Bup TA training • Sit e Specific Updat es • Opioid Crisis: Nationwide Overview • Stigma, Shame, and the Power of Language • Relapse Sensitive Environments and Retention in Care • Met hods t o Reduce Diversion • Higher Level of Care, Alt ernat ives t o OBOT, Tapering Off Bup • Mental Health and OUD • Pain and OUD Metro Health Clinic Bluegrass Care Clinic Centro Ararat Clinic Opioid Crisis Nationwide Nationally, opioids were involved in more than 61 percent of deaths from overdoses in 2014 By HAEYOUN PARK and MATTHEW BLOCH JAN. 19, 2016, New York Times The C.D.C. says that 91 people in the United States die every day from opioid overdose. By CHRISTINE HAUSERFEB. 13, 2017, New York Times 2015 Data Comparison Overdose deaths: 52,404. Car crashes deaths: 37,757 Gun deaths, including homicides and suicides: 36,252 NBC News, Dec 9 2016 N gggg 2016 National Drug Threat Summary Opiate Crisis Nationwide “Deaths from overdoses are reaching levels similar to the H.I.V. epidemic at its peak” Robert Anderson, the C.D.C.’s chief of mortality statistics. HIV and OUD: ?W h o ? W h a t ? a r e w e t r e a t i n g ? 29 year old m ale 1/18/2017: HIV Viral Load= <20 1/25/2016: Pain MGMT Profile: +Amphetamines +Methamphetamines +Benzodiazepines +Mar ijuana +Opiat es +Morphine HIV and OUD 32 year old m ale 11/15/2016: HIV Viral Load= 26 2/19/2017: -

PCF4 Revised Monographs (Since Publication September 2011 to July 2014)
www.palliativedrugs.com PCF4 revised monographs (since publication September 2011 to July 2014) Monograph Chapter number Date updated 5HT3 antagonists Chapter 04 Correction Apr-13 5HT3 antagonists Chapter 04 Jun-14 Adjuvant analgesics Chapter 05 Jun-14 Alfentanil Chapter 05 May-14 Amitriptyline Chapter 04 Oct-13 Anaemia Chapter 09 Apr-14 Analgesic drugs and fitness to drive Chapter 19 Jun-14 Anaphylaxis Chapter 27 May-13 Anaphylaxis Chapter 27 Correction Oct-13 Anaphylaxis Chapter 27 Jul-14 Antacids Chapter 01 Sep-12 Antacids Chapter 01 Minor update Jun-14 Antibacterials in palliative care Chapter 06 Sep-12 Antibacterials in palliative care Chapter 06 Minor update Apr-14 Anticoagulants Chapter 02 Minor update Aug-13 Anticoagulants (new) Chapter 02 New May-13 Antidepressants Chapter 04 Oct-13 Anti-emetics Chapter 04 Jun-14 Anti-epileptics pre-synaptic calcium channel blockers Chapter 04 Discontinued May-14 Anti-epileptics sodium channel blockers Chapter 04 Discontinued May-14 Anti-epileptics Chapter 04 Merged monograph May-14 Antifibrinolytics Chapter 02 Aug-13 Antihistaminic antimuscarinic anti-emetics Chapter 04 Jun-14 Antimuscarinics Chapter 01 Correction Apr-13 Antimuscarinics Chapter 01 Apr-14 Antipsychotics Chapter 04 Jun-14 Antitussives Chapter 03 Mar-14 Artificial saliva Chapter 11 Jun-14 Ascorbic acid Chapter 09 Nov-12 Baclofen Chapter 10 Jun-14 Barrier products Chapter 12 Apr-14 Benzodiazepines Chapter 04 Jun-14 Bisphosphonates Chapter 07 Merged monograph Jun-14 Buprenorphine Chapter 05 Jun-13 Buprenorphine Chapter 05 Jun-14 -

CEDIA® Buprenorphine II Assay
CEDIA® Buprenorphine II Assay For In Vitro Diagnostic Use Only Rx Only 10020849 (3 x 17 mL Kit) 10020850 (65 mL Kit) Intended Use Warnings and Precautions The CEDIA® Buprenorphine II Assay is a homogeneous enzyme immunoassay for the DANGER: Powder reagents contain ≤55% w/w Bovine Serum Albumin (BSA) fragments and qualitative and/or semi-quantitative determination for the presence of buprenorphine and its ≤1% w/w Sodium Azide. Liquid reagents contain ≤0.5% Bovine Serum, ≤0.2% Sodium Azide, metabolites in human urine at a cut-off concentration of 10 ng/mL. The assay is intended to and ≤0.1% Drug-Specific Antibody (Mouse). be used in laboratories and provides a simple and rapid analytical screening procedure to detect buprenorphine and its metabolites in human urine. The assay is designed for use with a The reagents are harmful if swallowed. number of clinical chemistry analyzers. H317 - May cause allergic skin reaction. The semi-quantitative mode is for the purpose of enabling laboratories to determine an H334 - May cause allergy or asthma symptoms or breathing difficulties if inhaled. appropriate dilution of the specimen for confirmation by a confirmatory method such as EUH032 - Contact with acids liberates very toxic gas. Liquid chromatography/tandem mass spectrometry (LC-MS/MS) or permitting laboratories to establish quality control procedures. Avoid breathing mist or vapor. Contaminated work clothing should not be allowed out of the workplace. Wear protective gloves/eye protection/face protection. In case of inadequate The assay provides only a preliminary analytical test result. A more specific alternative ventilation wear respiratory protection. -

Buprenorphine
Buprenorphine: Everything You Need to Know OCTOBER 2016 uprenorphine, a medication that is FDA-approved others are FDA-approved for pain (injectable, patch, and for addiction treatment and pain relief, has also buccal mucoadhesive film). Bbeen found to dramatically decrease death rates from opioid overdose. Only 10% of patients needing Per the Drug Addiction Treatment Act of 2000 (DATA treatment, however, have access to the medication. 2000), physicians need a waiver to prescribe buprenor- phine for addiction; attendance in an eight-hour This document provides answers to frequently asked in-person or online course is required to obtain a waiver. questions about buprenorphine and supplements the The Comprehensive Addiction and Recovery Act of 2016 California Health Care Foundation (CHCF) webinars allows nurse practitioners and physician assistants to pre- “Expanding Access to Buprenorphine in Primary scribe buprenorphine treatment after 24 hours of certified Care Practices” and “Is Buprenorphine for Pain a training. Clinicians are capped at 30 patients the first year Safer Alternative to High-Dose or Long-Term Opioid and 100 patients per year thereafter. The cap increases Use?”1, 2 The clinical information contained in this paper to 275 patients for physicians board-certified in addic- is intended to act as a guideline, not a replacement for tion, or those in practices that meet certain qualifications: onsite medical judgment. Based on information cov- 24-hour call coverage, use of health information technol- ered in the CHCF webinars, the content was reviewed ogy, provision of care management services, registration by addiction specialists Howard Kornfeld, MD, James with CURES (Controlled Substance Utilization Review and Gasper, PharmD, and Andrew Herring, MD. -
![Chapter 329 [New] Uniform Controlled Substances Act](https://docslib.b-cdn.net/cover/1442/chapter-329-new-uniform-controlled-substances-act-1221442.webp)
Chapter 329 [New] Uniform Controlled Substances Act
CHAPTER 329 [NEW] UNIFORM CONTROLLED SUBSTANCES ACT Part I. General Provisions Section 329-1 Definitions 329-2 Hawaii advisory commission on drug abuse and controlled substances; number; appointment 329-3 Annual report 329-4 Duties of the commission Part II. Standards and Schedules 329-11 Authority to schedule controlled substances 329-12 Nomenclature 329-13 Schedule I tests 329-14 Schedule I 329-15 Schedule II tests 329-16 Schedule II 329-17 Schedule III Tests 329-18 Schedule III 329-19 Schedule IV tests 329-20 Schedule IV 329-21 Schedule V tests 329-22 Schedule V 329-23 Republishing and distribution of schedules Part III. Regulation of Manufacture, Distribution, Prescription, and Dispensing of Controlled Substances 329-31 Rules 329-31.5 Clinics 329-32 Registration requirements 329-33 Registration 329-34 Revocation and suspension of registration 329-35 Order to show cause 329-36 Records of registrants 329-37 Filing requirements 329-38 Prescriptions 329-39 Labels 329-40 Methadone treatment programs Part IV. Offenses and Penalties 329-41 Prohibited acts B-penalties 329-42 Prohibited acts C-penalties 329-43 Penalties under other laws 329-43.5 Prohibited acts related to drug paraphernalia Amended 0612 1 329-44 Notice of conviction to be sent to licensing board, department of commerce and consumer affairs 329-45 Repealed 329-46 Prohibited acts related to visits to more than one practitioner to obtain controlled substance prescriptions 329-49 Administrative penalties 329-50 Injunctive relief Part V. Enforcement and Administrative Provisions 329-51 Powers of enforcement personnel 329-52 Administrative inspections 329-53 Injunctions 329-54 Cooperative arrangements and confidentiality 329-55 Forfeitures 329-56 Burden of proof; liabilities 329-57 Judicial review 329-58 Education and research 329-59 Controlled substance registration revolving fund; established Part VI.