An Approach to the Management of Bleeding Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
What Does a Diagnosis of Myeloma Mean in 2015
What does a diagnosis of Myeloma mean in 2015 Dr Aristeidis Chaidos Consultant Haematologist Hammersmith Hospital Learning objectives • define myeloma and related disorders • diagnosis & disease monitoring • “many myelomas”: staging & prognostic systems • the evolving landscape in myeloma treatment • principles of management with emphasis to care in the community • future challenges and novel therapies Myeloma – overview • malignancy of the plasma cells (PC): the terminally differentiated, antibody producing B cells • myeloma cells infiltrate the bone marrow • IgG or IgA paraprotein (PP) and/or free light chains in blood and urine • bone destruction • kidney damage • anaemia • despite great advances in the last 15 years myeloma remains an incurable disease Myeloma in figures • 1% of all cancers – 13% of blood cancers • median age at diagnosis: 67 years • only 1% of patients <40 years • 4 – 5 new cases per 100,000 population annually, but different among ethnic groups • 4,800 new myeloma patients in the UK each year • the prevalence of myeloma in the community increases with outcome improvements and aging population Myeloma related conditions smoldering symptomatic remitting plasma cell MGUS refractory myeloma myeloma relapsing leukaemia <10% PC ≥10% PC +/- ≥10% PC or plasmacytoma circulating PC PP <30g/L PP ≥30g/L Any PP in serum and/or urine extramedullary no organ no organ disease damage or damage or organ damage & symptoms symptoms symptoms Death MGUS monoclonal gammopathy of unknown significance • The most common pre-malignant condition: -

Guidelines on the Assessment of Bleeding Risk Prior to Surgery Or Invasive Procedures
guideline Guidelines on the assessment of bleeding risk prior to surgery or invasive procedures British Committee for Standards in Haematology Y. L. Chee, 1 J. C. Crawford, 2 H. G. Watson1 and M. Greaves3 1Department of Haematology, Aberdeen Royal Infirmary, Aberdeen, 2Department of Anaesthetics, Southern General Hospital, Glasgow, and 3Department of Medicine and Therapeutics, School of Medicine, University of Aberdeen, Aberdeen, UK surgery or invasive procedures to predict bleeding risk. The Summary aim is to evaluate the use of indiscriminate testing. Appro- Unselected coagulation testing is widely practiced in the priate testing of patients with relevant clinical features on process of assessing bleeding risk prior to surgery. This may history or examination is not the topic of this guideline. The delay surgery inappropriately and cause unnecessary concern target population includes clinicians responsible for assess- in patients who are found to have ‘abnormal’ tests. In addition ment of patients prior to surgery and other invasive it is associated with a significant cost. This systematic review procedures. was performed to determine whether patient bleeding history and unselected coagulation testing predict abnormal periop- Methods erative bleeding. A literature search of Medline between 1966 and 2005 was performed to identify appropriate studies. The writing group was made up of UK haematologists with Studies that contained enough data to allow the calculation of a special interest in bleeding disorders and an anaesthetist. the predictive value and likelihood ratios of tests for periop- First, the commonly employed coagulation screening tests erative bleeding were included. Nine observational studies were identified and their general and specific limitations (three prospective) were identified. -

Familial Multiple Coagulation Factor Deficiencies
Journal of Clinical Medicine Article Familial Multiple Coagulation Factor Deficiencies (FMCFDs) in a Large Cohort of Patients—A Single-Center Experience in Genetic Diagnosis Barbara Preisler 1,†, Behnaz Pezeshkpoor 1,† , Atanas Banchev 2 , Ronald Fischer 3, Barbara Zieger 4, Ute Scholz 5, Heiko Rühl 1, Bettina Kemkes-Matthes 6, Ursula Schmitt 7, Antje Redlich 8 , Sule Unal 9 , Hans-Jürgen Laws 10, Martin Olivieri 11 , Johannes Oldenburg 1 and Anna Pavlova 1,* 1 Institute of Experimental Hematology and Transfusion Medicine, University Clinic Bonn, 53127 Bonn, Germany; [email protected] (B.P.); [email protected] (B.P.); [email protected] (H.R.); [email protected] (J.O.) 2 Department of Paediatric Haematology and Oncology, University Hospital “Tzaritza Giovanna—ISUL”, 1527 Sofia, Bulgaria; [email protected] 3 Hemophilia Care Center, SRH Kurpfalzkrankenhaus Heidelberg, 69123 Heidelberg, Germany; ronald.fi[email protected] 4 Department of Pediatrics and Adolescent Medicine, University Medical Center–University of Freiburg, 79106 Freiburg, Germany; [email protected] 5 Center of Hemostasis, MVZ Labor Leipzig, 04289 Leipzig, Germany; [email protected] 6 Hemostasis Center, Justus Liebig University Giessen, 35392 Giessen, Germany; [email protected] 7 Center of Hemostasis Berlin, 10789 Berlin-Schöneberg, Germany; [email protected] 8 Pediatric Oncology Department, Otto von Guericke University Children’s Hospital Magdeburg, 39120 Magdeburg, Germany; [email protected] 9 Division of Pediatric Hematology Ankara, Hacettepe University, 06100 Ankara, Turkey; Citation: Preisler, B.; Pezeshkpoor, [email protected] B.; Banchev, A.; Fischer, R.; Zieger, B.; 10 Department of Pediatric Oncology, Hematology and Clinical Immunology, University of Duesseldorf, Scholz, U.; Rühl, H.; Kemkes-Matthes, 40225 Duesseldorf, Germany; [email protected] B.; Schmitt, U.; Redlich, A.; et al. -

Intracerebral Bleeding in Young Infants Due to Rare Etiologies–A
eona f N tal l o B a io n l r o u g y o J Tewari et al., J Neonatal Biol 2016, 5:2 Journal of Neonatal Biology DOI: 10.4172/2167-0897.1000221 ISSN: 2167-0897 Case Report Open access Intracerebral Bleeding in Young Infants due to Rare Etiologies–A Report of two Cases Vishal Vishnu Tewari1*, Kunal Tewari2 and Ritu Mehta3 1Department of Pediatrics, Army Hospital (Referral and Research), New Delhi, India 2Department of Anaesthesia, Classified Specialist Anesthesia, Base Hospital, New Delhi, India 3Department of Pathology, All India Institute of Medical Sciences, New Delhi, India *Corresponding author: Vishal Vishnu Tewari, Department of Pediatrics, Army Hospital, New Delhi, India,Tel: +91-8826118889, E-mail: [email protected] Rec date: April 29, 2016; Acc date: May 16, 2016; Pub date: May 23, 2016 Copyright: © 2016 Tewari VV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Neonates and young infants are physiologically encumbered by an inadequate hemostatic mechanism. They may also have inherited or acquired bleeding disorders which may have a catastrophic presentation with intracerebral hemorrhage. The need to reach an accurate diagnosis is paramount in order to provide accurate therapy and genetic counseling. We report two infants who presented with unprovoked life threatening massive intracerebral hemorrhage. The first infant was diagnosed and managed for congenital factor V deficiency while the second infant had Glanzmann thrombasthenia. Keywords: Intracerebral bleeding; Congenital factor V deficiency; disorder in the family. -
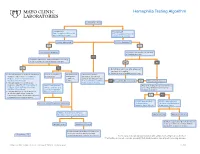
Hemophilia Testing Algorithm
Hemophilia Testing Algorithm Symptomatic male Hemophilia A Hemophilia B F8A / Coagulation Factor VIII F_9 / Coagulation Factor IX Activity Assay, Plasma Activity Assay, Plasma Activity decreased? Activity decreased? YES YES Hemophilia A diagnosis ■ Vitamin K antagonist (ie, warfarin) ■ Child/adolescent? NO F8 genetic testing has been performed on a family member and the specific mutation is known? YES NO YES NO ■ Retest when >4 weeks after antagonist treatment is complete ■ Adjust decreased activity levels for age ■ If known mutation is an Intron 1 Inversion Severe hemophilia: Moderate/mild If the activity assays mutation, order F81B / Hemophilia A activity <1% hemophilia: are normal, consider an F8 Gene, Intron 1 Inversion Known activity 1% alternate bleeding disorder: Mutation, Whole Blood* to 55% ALBLD / Bleeding Diathesis NO Is activity still decreased? YES Hemophilia B diagnosis ■ If known mutation is an Intron 22 Profile, Limited, Plasma inversion, order F822B / Hemophilia A F8INV / Hemophilia A F9 genetic testing has been performed F8 Gene, Intron 22 Inversion Known F8 Gene, Intron 1 and on a family member and the specific Mutation, Whole Blood* 22 Inversion Mutation mutation is known? ■ If known mutation is a point mutation Analysis, Whole Blood or deletion/duplication, contact a Laboratory Genetic Counselor to discuss YES NO targeted familial mutation testing FIXKM / Hemophilia B, NGSF9 / Hemophilia B, Inversion found Inversion not found F9 Gene Known F9 Gene, Next-Generation Mutation, Whole Blood* Sequencing, Varies F8NGS / -

Diagnosis of Inherited Platelet Disorders on a Blood Smear
Journal of Clinical Medicine Article Diagnosis of Inherited Platelet Disorders on a Blood Smear Carlo Zaninetti 1,2,3 and Andreas Greinacher 1,* 1 Institut für Immunologie und Transfusionsmedizin, Universitätsmedizin Greifswald, 17489 Greifswald, Germany; [email protected] 2 University of Pavia, and IRCCS Policlinico San Matteo Foundation, 27100 Pavia, Italy 3 PhD Program of Experimental Medicine, University of Pavia, 27100 Pavia, Italy * Correspondence: [email protected]; Tel.: +49-3834-865482; Fax: +49-3834-865489 Received: 19 January 2020; Accepted: 12 February 2020; Published: 17 February 2020 Abstract: Inherited platelet disorders (IPDs) are rare diseases featured by low platelet count and defective platelet function. Patients have variable bleeding diathesis and sometimes additional features that can be congenital or acquired. Identification of an IPD is desirable to avoid misdiagnosis of immune thrombocytopenia and the use of improper treatments. Diagnostic tools include platelet function studies and genetic testing. The latter can be challenging as the correlation of its outcomes with phenotype is not easy. The immune-morphological evaluation of blood smears (by light- and immunofluorescence microscopy) represents a reliable method to phenotype subjects with suspected IPD. It is relatively cheap, not excessively time-consuming and applicable to shipped samples. In some forms, it can provide a diagnosis by itself, as for MYH9-RD, or in addition to other first-line tests as aggregometry or flow cytometry. In regard to genetic testing, it can guide specific sequencing. Since only minimal amounts of blood are needed for the preparation of blood smears, it can be used to characterize thrombocytopenia in pediatric patients and even newborns further. -

Approach to Bleeding Diathesi
Approach to Bleeding Diathesis Dr.Nalini K Pati MD, DNB, DCH (Syd), FRCPA Paediatric Haematologist Royal Children’s Hospital Melbourne Australia Objectives Objectives - I I. Clinical aspects of bleeding Clinical aspects of bleeding II. Hematologic disorders causing bleeding • Coagulation factor disorders • Platelet disorders III. Approach to acquired bleeding disorders • Hemostasis in liver disease • Surgical patients • Warfarin toxicity IV. Approach to laboratory abnormalities • Diagnosis and management of thrombocytopenia V. Drugs and blood products used for bleeding Clinical Features of Bleeding Disorders Petechiae Platelet Coagulation (typical of platelet disorders) disorders factor disorders Site of bleeding Skin Deep in soft tissues Mucous membranes (joints, muscles) (epistaxis, gum, vaginal, GI tract) Petechiae Yes No Ecchymoses (“bruises”) Small, superficial Large, deep Hemarthrosis / muscle bleeding Extremely rare Common Do not blanch with pressure Bleeding after cuts & scratches Yes No (cf. angiomas) Bleeding after surgery or trauma Immediate, Delayed (1-2 days), usually mild often severe Not palpable (cf. vasculitis) Ecchymoses (typical of coagulation factor disorders) Objectives - II Hematologic disorders causing bleeding – Coagulation factor disorders – Platelet disorders Coagulation factor disorders Hemophilia A and B Inherited bleeding Acquired bleeding Hemophilia A Hemophilia B disorders disorders Coagulation factor deficiency Factor VIII Factor IX – Hemophilia A and B – Liver disease – vonWillebrands disease – Vitamin K Inheritance X-linked X-linked recessive recessive – Other factor deficiencies deficiency/warfarin overdose Incidence 1/10,000 males 1/50,000 males –DIC Severity Related to factor level <1% - Severe - spontaneous bleeding 1-5% - Moderate - bleeding with mild injury 5-25% - Mild - bleeding with surgery or trauma Complications Soft tissue bleeding Hemarthrosis (acute) Hemophilia Clinical manifestations (hemophilia A & B are indistinguishable) Hemarthrosis (most common) Fixed joints Soft tissue hematomas (e. -

TPA-2012-2ING:Layout 1
106 Original Article DOI: 10.4274/tpa.823 Glanzmann thrombasthenia: Cerrahpaşa Medical Faculty experience Büşra Kutlubay, Gül Nihal Özdemir, Gülen Tüysüz, Hilmi Apak, Tiraje Celkan İstanbul University Cerrahpaşa Medical Faculty, Department of Pediatrics, Division of Pediatric Hematology-Oncology, İstanbul, Turkey Sum mary Aim: Glazmann thrombasthenia is a rare autosomal recessive disease characterized by a defect in platelet aggregation. Herein, we report the management of children with Glazmann thrombasthenia followed up at Cerrahpasa Medical Faculty Pediatric Hematology Department. Material and Method: The files of nineteen patients (42% girls, 58% boys; median age: 10 months) were retrospectively reviewed. Results: The median age of onset of bleeding symptoms was 9 months (2 weeks-24 months). All patients presented with easy bruising and mucosal bleeding. Fourteen patients’ parents were consanguineous. In 15 patients, flow cytometry was performed. According to this, 7 patients had type I, 6 patients had type II and 2 patients had type III disease. Nine patients were treated with thrombocyte transfusion, tranexamic acid, recombinant active factor VII and fibrin glue as a single or combined therapy; none of them had a major bleeding complication. Conclusions: Bleeding control during invasive procedures may be challenging in children with Glazmann thrombasthenia; local treatments, DDAVP, steroid and antifibrinolytics may be used with success. (Turk Arch Ped 2012; 47: 106-8) Key words: Glanzmann thrombasthenia, thrombocyte function disorder Introduction test, GT platelets do not aggregate following interaction with any substance except for ristocetin. In addition to Glanzmann thrombasthenia (GT) was described by Dr. aggregometer, low than normal levels of glycoprotein (GP) IIb- Eduard Glanzmann in 1918 for the first time as abnormal clot IIIa can be determined with flow cytometer using CD41 and retraction and defects in platelets (1). -

The Patient Is Bleeding & the PT/Aptt Are Normal
The Patient is Bleeding & the PT/aPTT are Normal Dorothy Adcock, MD Title: The patient is bleeding but the APTT and PT are normal As Dr. Worfolk mentioned, the topic of the discussion this morning, the patient is bleeding, but the aPTT and PT are normal. Title: The patient is bleeding but the APTT and PT are normal - Outline What we will discuss this morning is, first of all, we will review the aPTT and PT assays, and I will be referring to the aPTT as just the PTT in the future. We will discuss hemorrhagic disorders of the intrinsic, extrinsic, and common pathway systems that may have a normal PTT and PT. We will then discuss hemorrhagic disorders associated with abnormal fibrin clot formation of the fibrinolytic system. And then finally, we will list disorders of platelets and vasculature that may be associating with bleeding diathesis as well. 1 Title: Screening tests of hemostasis - APTT and PT Now I am certain that all of you are aware that the PTT and PT are the most common screening tests of the hemostatic system. These tests are of course readily available to us in our laboratories; they are familiar to us and inexpensive. And really what I would like to do this morning is bring some more material to us regarding these assays. In the sense that, since these assays have been in the laboratory for such a long period of time, we tend to take these assays for granted, and perhaps expect too much out of these assays. So what I would like to review with you this morning are some of the limitations of these assays. -

Role of Thromboelastography Versus Coagulation Screen As a Safety
The Journal of Obstetrics and Gynecology of India (September–October 2016) 66(S1):S340–S346 DOI 10.1007/s13224-016-0906-y ORIGINAL ARTICLE Role of Thromboelastography Versus Coagulation Screen as a Safety Predictor in Pre-eclampsia/Eclampsia Patients Undergoing Lower-Segment Caesarean Section in Regional Anaesthesia 1 2 2 3 2 Asrar Ahmad • Monica Kohli • Anita Malik • Megha Kohli • Jaishri Bogra • 2 2 2 Haider Abbas • Rajni Gupta • B. B. Kushwaha Received: 6 February 2016 / Accepted: 12 April 2016 / Published online: 22 June 2016 Ó Federation of Obstetric & Gynecological Societies of India 2016 About the Author Asrar Ahmad graduated from Ganesh Shankar Vidyarthi Memorial Medical College, Kanpur, and postgraduated (in Anaesthesiology) from King George Medical University, Lucknow. Presently, he works as Assistant Professor in Department of Anaesthesiology in T. S. Mishra Medical College and Hospital, Lucknow. He works in all fields of anaesthesiology, but has special interest in obstetric anaesthesia. Abstract Purpose In this study, we aimed to correlate thromboe- Dr. Asrar Ahmad M.D. (Anesthesiology), Assistant Professor, T. lastography (TEG) variables versus conventional coagula- S. Mishra Medical College and Hospital; Prof. Monica Kohli M.D. tion profile in all patients presenting with pre-eclampsia/ (Anesthesiology), PDCC, Professor, King George’s Medical eclampsia and to see whether TEG would be helpful for University; Prof. Anita Malik M.D. (Anesthesiology), Professor, King George’s Medical University; Dr. Megha Kohli, Junior Resident 3 evaluating coagulation in parturients before regional (Anesthesiology and Intensive Care), Maulana Azad Medical anaesthesia. College; Prof. Jaishri Bogra D.A., M.D. (Anesthesiology), Professor, Materials and Methods This was a prospective study on King George’s Medical University; Prof. -

Coagulation Assessment in Normal Pregnancy: Thrombelastography with Citrated Non Activated Samples
Anno: 2012 Lavoro: Mese: December titolo breve: COAGULATION ASSESSMENT IN NORMAL PREGNANCY Volume: 78 primo autore: DELLA ROCCA No: 12 pagine: 1357-64 Rivista: MINERVA ANESTESIOLOGICA Cod Rivista: Minerva Anestesiol © , COPYRIGHT 2012 EDIZIONI MINERVA MEDICA ORIGINAL ARTICLE Coagulation assessment in normal pregnancy: thrombelastography with citrated non activated samples G. DELLA ROCCA 1, T. DOGARESCHI 1, T. CECCONET 1, S. BUTTERA 1, A. SPASIANO 1, P. NADBATH 1, M. ANGELINI 2, C. GALLUZZO 2, D. MARCHESONI 2 1Department of Anesthesia and Intensive Care Medicine, University of Udine, Udine, Italy; 2Department of Obstetrics and Gynecology, University of Udine, Udine, Italy ABSTRACT Backgound. Thrombelastography (TEG) provides an effective and convenient means of whole blood coagulation monitoring. TEG evaluates the elastic properties of whole blood and provides a global assessment of hemostatic function. Previous studies performed TEG on native blood sample, but no data are available with citrated samples in healthy pregnant women at term. The aim of this study was to investigate the effect of pregnancy on coagula- tion assessed by TEG and establish normal ranges of TEG values in pregnant women at term comparing them with healthy non pregnant young women. Methods. We enrolled pregnant women at term undergoing elective cesarean section or labour induction (PREG group) and healthy non-pregnant women (CTRL group). Women with fever or inflammatory syndrome, defined as C-reactive protein (CRP) >5 mg/L and with a platelet count <150.000/mm3 have been excluded. For each women hemochrome and standard coagulation test were assessed. At the same time we performed a thrombelastographic test with Hemoscope TEG® after sample recalcification without using any activator. -

Pathophysiology of Bleeding Diathesis in Haemophilia-A
The Egyptian Journal of Medical Human Genetics 19 (2018) 285–295 Contents lists available at ScienceDirect The Egyptian Journal of Medical Human Genetics journal homepage: www.sciencedirect.com Review Pathophysiology of bleeding diathesis in haemophilia-A: A sequential and critical appraisal of non-FVIII related haemostatic dysfunctions and their therapeutic implications ⇑ Umma A. Ibrahim a, Sagir G. Ahmed b, a Department of Paediatrics, Bayero University, PMB 3011, Kano, Kano State, Nigeria b Department of Haematology, Aminu Kano Teaching Hospital, PMB 3452, Kano, Kano State, Nigeria article info abstract Article history: Haemophilia-A is characterized by deficiency of FVIII, but the bleeding diathesis is not a mere reflection Received 29 December 2017 low FVIII activity. The pathophysiology of haemophilic bleeding diathesis is a complex interplay between Accepted 14 January 2018 defective procoagulant function and up-regulated fibrinolysis. Moreover, haemophilic bleeding diathesis Available online 1 February 2018 is frequently compounded by treatment-related and infective complications such as FVIII inhibitors, hep- atitis, HIV infection, non-steroidal anti-inflammatory drugs (NSAID) induced gastritis, and infective Keywords: mucosal injuries such as H pylori gastritis and intestinal and urinary helminthiasis. Hence, pathophysi- Haemophilia ology of haemophilic bleeding is multi-factorial, encompassing both FVIII and non-FVIII haemostatic Bleeding diathesis defects. Currently available literature on pathophysiologic roles of non-FVIII haemostatic defects in hae- Pathophysiology Targeted therapy mophilia is fragmented. This articles is aimed at providing a composite and comprehensive review of the Non-FVIII therapy roles of non-FVIII haemostatic defects and their therapeutic implications in haemophilic bleeding diathe- FVIII by-pass sis, which will enable a holistic approach towards clinical management of the bleeding diathesis.