Final Report of IMNCI Training Courses in Five Selected States and Regions 2016-2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Appendix 6 Satellite Map of Proposed Project Site
APPENDIX 6 SATELLITE MAP OF PROPOSED PROJECT SITE Hakha Township, Rim pi Village Tract, Chin State Zo Zang Village A6-1 Falam Township, Webula Village Tract, Chin State Kim Mon Chaung Village A6-2 Webula Village Pa Mun Chaung Village Tedim Township, Dolluang Village Tract, Chin State Zo Zang Village Dolluang Village A6-3 Taunggyi Township, Kyauk Ni Village Tract, Shan State A6-4 Kalaw Township, Myin Ma Hti Village Tract and Baw Nin Village Tract, Shan State A6-5 Ywangan Township, Sat Chan Village Tract, Shan State A6-6 Pinlaung Township, Paw Yar Village Tract, Shan State A6-7 Symbol Water Supply Facility Well Development by the Procurement of Drilling Rig Nansang Township, Mat Mon Mun Village Tract, Shan State A6-8 Nansang Township, Hai Nar Gyi Village Tract, Shan State A6-9 Hopong Township, Nam Hkok Village Tract, Shan State A6-10 Hopong Township, Pawng Lin Village Tract, Shan State A6-11 Myaungmya Township, Moke Soe Kwin Village Tract, Ayeyarwady Region A6-12 Myaungmya Township, Shan Yae Kyaw Village Tract, Ayeyarwady Region A6-13 Labutta Township, Thin Gan Gyi Village Tract, Ayeyarwady Region Symbol Facility Proposed Road Other Road Protection Dike Rainwater Pond (New) : 5 Facilities Rainwater Pond (Existing) : 20 Facilities A6-14 Labutta Township, Laput Pyay Lae Pyauk Village Tract, Ayeyarwady Region A6-15 Symbol Facility Proposed Road Other Road Irrigation Channel Rainwater Pond (New) : 2 Facilities Rainwater Pond (Existing) Hinthada Township, Tha Si Village Tract, Ayeyarwady Region A6-16 Symbol Facility Proposed Road Other Road -

5-Year Strategic Development Plan, 2018-2022 Pa-O Self-Administered Zone Shan State, Republic of the Union of Myanmar
5-Year Strategic Development Plan, 2018-2022 Pa-O Self-Administered Zone Shan State, Republic of the Union of Myanmar A PROSPEROUS COMMUNITY FOR THIS AND FUTURE VOLUME II: DEVELOPMENT PROPOSALS GENERATIONS Myanmar Institute for Integrated Development 12, Kanbawza Street, Bahan Township Yangon, Myanmar [email protected] | www.mmiid.org Author | Paul Knipe Contributors | Victoria Garcia, Mike Haynes, U Yae Htut, Qingrui Huang, Jolanda Jonkhart, Joern Kristensen, Daw Khin Yupar Kyaw, U Ko Lwin, Daw Hsu Myat Myint Lwin, U Myint Lwin, Daw Thet Htar Myint, U Nay Linn Oo, Samuel Pursch, Barbara Schott, Dr Khin Thawda Shein, U Kyaw Thein, Daw Nilar Win Yangon, August 2018 Cover image | Participant from the Pa-O Women’s Union at the Evaluation and Strategy Workshop TABLE OF CONTENTS Abbreviations .........................................................................................................................I Map of the Pa-O SAZ ..........................................................................................................II Introduction ...........................................................................................................................1 1. Infrastructure ...................................................................................................................2 Map 1: Hopong Township village road upgrade ...................................................3 Map 2: Hsihseng Township village road upgrade ................................................4 Map 3: Pinlaung Township village road upgrade .................................................5 -

December 2008
cover_asia_report_2008_2:cover_asia_report_2007_2.qxd 28/11/2008 17:18 Page 1 Central Committee for Drug Lao National Commission for Drug Office of the Narcotics Abuse Control Control and Supervision Control Board Vienna International Centre, P.O. Box 500, A-1400 Vienna, Austria Tel: (+43 1) 26060-0, Fax: (+43 1) 26060-5866, www.unodc.org Opium Poppy Cultivation in South East Asia Lao PDR, Myanmar, Thailand OPIUM POPPY CULTIVATION IN SOUTH EAST ASIA IN SOUTH EAST CULTIVATION OPIUM POPPY December 2008 Printed in Slovakia UNODC's Illicit Crop Monitoring Programme (ICMP) promotes the development and maintenance of a global network of illicit crop monitoring systems in the context of the illicit crop elimination objective set by the United Nations General Assembly Special Session on Drugs. ICMP provides overall coordination as well as direct technical support and supervision to UNODC supported illicit crop surveys at the country level. The implementation of UNODC's Illicit Crop Monitoring Programme in South East Asia was made possible thanks to financial contributions from the Government of Japan and from the United States. UNODC Illicit Crop Monitoring Programme – Survey Reports and other ICMP publications can be downloaded from: http://www.unodc.org/unodc/en/crop-monitoring/index.html The boundaries, names and designations used in all maps in this document do not imply official endorsement or acceptance by the United Nations. This document has not been formally edited. CONTENTS PART 1 REGIONAL OVERVIEW ..............................................................................................3 -

Financial Inclusion
ANNUAL REPORT 2020 I LIFT Annual Report 2020 ANNUAL REPORT 2020 II III LIFT Annual Report 2020 ABBREVIATIONS AND ACRONYMS ADB Asian Development Bank LBVD Livestock Breeding and Veterinary ACKNOWLEDGEMENTS Department CBO Community-based Organisation We thank the governments of Australia, Canada, the European Union, LEARN Leveraging Essential Nutrition Ireland, New Zealand, Norway, Switzerland, the United Kingdom, and CSO Civil Society Organisation Actions To Reduce Malnutrition project the United States of America for their kind contributions to improving the livelihoods and food security of rural poor people in Myanmar. Their DAR Department of Agricultural MAM Moderate acute malnutrition support to the Livelihoods and Food Security Fund (LIFT) is gratefully Research acknowledged. M&E Monitoring and evaluation DC Donor Consortium MADB Myanmar Agriculture Department of Agriculture Development Bank DISCLAIMER DoA DoF Department of Fisheries MEAL Monitoring, evaluation, This document is based on information from projects funded by LIFT in accountability and learning 2020 and supported with financial assistance from Australia, Canada, the DRD Department for Rural European Union, Ireland, New Zealand, Norway, Switzerland, the United Development MoALI Ministry of Agriculture, Kingdom, and the United States of America. The views expressed herein Livestock and Irrigation should not be taken to reflect the official opinion of the LIFT donors. DSW Department of Social Welfare MoE Ministry of Education Exchange rate: This report converts MMK into -

Social Assessment for Ayeyarwady Region and Shan State
AND DEVELOPMENT May 2019 Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized SOCIAL ASSESSMENT FOR AYEYARWADY REGION AND SHAN STATE Public Disclosure Authorized Myanmar: Maternal and Child Cash Transfers for Improved Nutrition 1 Myanmar: Maternal and Child Cash Transfers for Improved Nutrition Ministry of Social Welfare, Relief and Resettlement May 2019 2 TABLE OF CONTENTS Executive Summary ........................................................................................................................... 5 List of Abbreviations .......................................................................................................................... 9 List of Tables ................................................................................................................................... 10 List of BOXES ................................................................................................................................... 10 A. Introduction and Background....................................................................................................... 11 1 Objectives of the Social Assessment ................................................................................................11 2 Project Description ..........................................................................................................................11 3 Relevant Country and Sector Context..............................................................................................12 3.1 -
The Use of Geospatial Data and Technologies in Support of Immunization Microplanning in Myanmar Implementation Report (2017 - 2018)
The Use of Geospatial Data and Technologies in Support of Immunization Microplanning in Myanmar Implementation Report (2017 - 2018) 1 Acknowledgements This report was compiled by Rocco Panciera (UNICEF) and Steeve Ebener (Health GeoLab collaborative - HGLC) in the continuity of the support provided to the Department of Public Health (DOPH) by the Asian Development Bank (ADB), and with significant contributions by Nay Myo Thu (UNICEF). The authors would like to thank Daw Aye Aye Sein (Deputy Director General Ministry of Health and Sports - MOHS, Myanmar) and Dr. Htar Htar Lin (Myanmar EPI manager) for the invaluable support provided for the implementation of these activities. The following individuals have also provided invaluable support to different phases of this project: Maria Muniz, Health Specialist, UNICEF Lei Lei Mon (WHO) Dr. Than Tun Aung, Deputy Director General - Disaster/CEU, Ministry of Health and Sports, Myanmar Dr. Aung Kyaw Moe (Deputy Director, CEU/cEPI) Dr Tin Tun Win (MOHS) Lin Sein (MOHS) Nan Thida Phyo (MOHS) Izay Pantanilla (HGLC) Dr. Kaung Myat Thwin (MOHS) Maung Maung Htay Zaw (MOHS) May 2018 All reasonable precautions have been taken by UNICEF to verify the information contained in this publication. 2 Table of Contents ACKNOWLEDGEMENTS ........................................................................................................................................... 2 TABLE OF CONTENTS ............................................................................................................................................. -

Laboratory Aspects in Vpds Surveillance and Outbreak Investigation
Laboratory Aspect of VPD Surveillance and Outbreak Investigation Dr Ommar Swe Tin Consultant Microbiologist In-charge National Measles & Rubella Lab, Arbovirus section, National Influenza Centre NHL Fever with Rash Surveillance Measles and Rubella Achieving elimination of measles and control of rubella/CRS by 2020 – Regional Strategic Plan Key Strategies: 1. Immunization 2. Surveillance 3. Laboratory network 4. Support & Linkages Network of Regional surveillance officers (RSO) and Laboratories NSC Office 16 RSOs Office Subnational Measles & Rubella Lab, Subnational JE lab National Measles/Rubella Lab (NHL, Yangon) • Surveillance began in 2003 • From 2005 onwards, case-based diagnosis was done • Measles virus isolation was done since 2006 • PCR since 2016 Sub-National Measles/Rubella Lab (PHL, Mandalay) • Training 29.8.16 to 2.9.16 • Testing since Nov 2016 • Accredited in Oct 2017 Measles Serology Data Measles Measles IgM Measles IgM Measles IgM Test Done Positive Negative Equivocal 2011 1766 1245 452 69 2012 1420 1182 193 45 2013 328 110 212 6 2014 282 24 254 4 2015 244 6 235 3 2016 531 181 334 16 2017 1589 1023 503 62 Rubella Serology Data Rubella Test Rubella IgM Rubella IgM Rubella IgM Done Positive Negative Equivocal 2011 425 96 308 21 2012 195 20 166 9 2013 211 23 185 3 2014 257 29 224 4 2015 243 34 196 13 2016 535 12 511 12 2017 965 8 948 9 Measles Genotypes circulating in Myanmar 1. Isolation in VERO h SLAM cell line 2. Positive culture shows syncytia formation 3. Isolated MeV or sample by PCR 4. Positive PCR product is sent to RRL for sequencing 5. -
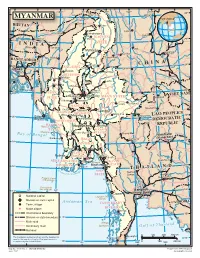
Map of Myanmar
94 96 98 J 100 102 ° ° Indian ° i ° ° 28 n ° Line s Xichang Chinese h a MYANMAR Line J MYANMAR i a n Tinsukia g BHUTAN Putao Lijiang aputra Jorhat Shingbwiyang M hm e ra k Dukou B KACHIN o Guwahati Makaw n 26 26 g ° ° INDIA STATE n Shillong Lumding i w d Dali in Myitkyina h Kunming C Baoshan BANGLADE Imphal Hopin Tengchong SH INA Bhamo C H 24° 24° SAGAING Dhaka Katha Lincang Mawlaik L Namhkam a n DIVISION c Y a uan Gejiu Kalemya n (R Falam g ed I ) Barisal r ( r Lashio M a S e w k a o a Hakha l n Shwebo w d g d e ) Chittagong y e n 22° 22° CHIN Monywa Maymyo Jinghong Sagaing Mandalay VIET NAM STATE SHAN STATE Pongsali Pakokku Myingyan Ta-kaw- Kengtung MANDALAY Muang Xai Chauk Meiktila MAGWAY Taunggyi DIVISION Möng-Pan PEOPLE'S Minbu Magway Houayxay LAO 20° 20° Sittwe (Akyab) Taungdwingyi DEMOCRATIC DIVISION y d EPUBLIC RAKHINE d R Ramree I. a Naypyitaw Loikaw w a KAYAH STATE r r Cheduba I. I Prome (Pye) STATE e Bay Chiang Mai M kong of Bengal Vientiane Sandoway (Viangchan) BAGO Lampang 18 18° ° DIVISION M a e Henzada N Bago a m YANGON P i f n n o aThaton Pathein g DIVISION f b l a u t Pa-an r G a A M Khon Kaen YEYARWARDY YangonBilugyin I. KAYIN ATE 16 16 DIVISION Mawlamyine ST ° ° Pyapon Amherst AND M THAIL o ut dy MON hs o wad Nakhon f the Irra STATE Sawan Nakhon Preparis Island Ratchasima (MYANMAR) Ye Coco Islands 92 (MYANMAR) 94 Bangkok 14° 14° ° ° Dawei (Krung Thep) National capital Launglon Bok Islands Division or state capital Andaman Sea CAMBODIA Town, village TANINTHARYI Major airport DIVISION Mergui International boundary 12° Division or state boundary 12° Main road Mergui n d Secondary road Archipelago G u l f o f T h a i l a Railroad 0 100 200 300 km Chumphon The boundaries and names shown and the designations Kawthuang 10 used on this map do not imply official endorsement or ° acceptance by the United Nations. -

Chapter 1 Introduction to the Geology of Myanmar
Downloaded from http://mem.lyellcollection.org/ by guest on October 2, 2021 Chapter 1 Introduction to the geology of Myanmar KHIN ZAW1*, WIN SWE2, A. J. BARBER3, M. J. CROW4 & YIN YIN NWE5 1CODES ARC Centre of Excellence in Ore Deposits, University of Tasmania, Private Bag 126, Hobart, Tasmania 7001, Australia 2Myanmar Geosciences Society, 303 MES Building, Hlaing University Campus, Yangon, Myanmar 3Department of Earth Sciences, Southeast Asian Research Group, Royal Holloway, Egham TW20 0EX, UK 428a Lenton Road, The Park, Nottingham NG7 1DT, UK 5Myanmar Applied Earth Sciences Association (MAESA), 15 (C) Pyidaungsu Lane, Bahan, Yangon, Myanmar *Correspondence: [email protected] Gold Open Access: This article is published under the terms of the CC-BY 3.0 license. The Republic of the Union of Myanmar (Pyidaungsu Tham- northern part of the Andaman Sea and the Gulf of Mottama mada Myanmar NaingNganDaw), formerly Burma, occupies (Martaban). The central lowlands are divided into two unequal the northwestern part of the Southeast Asian peninsula. It is parts by the Bago Yoma Ranges, the larger Ayeyarwaddy Valley bounded to the west by India, Bangladesh, the Bay of Bengal and the smaller Sittaung Valley. The Bago Yoma Ranges pass and the Andaman Sea, and to the east by China, Laos and Thai- northwards into a line of extinct volcanoes with small crater land. It comprises seven administrative regions (Ayeyarwaddy lakes and eroded cones; the largest of these is Mount Popa (Irrawaddy), Bago, Magway, Mandalay, Sagaing, Tanintharyi (1518 m). Coastal lowlands and offshore islands margin the (Tenasserim) and Yangon) and seven states (Chin, Kachin, Bay of Bengal to the west of the Rakhine Yoma and the Anda- Kayah, Kayin, Mon, Rakhine (Arakan) and Shan). -

MYANMAR A? Flood Kachin, Shan (North) State and Sagaing, Mandalay, Magway Region Imagery Analysis: 25 July 2020 | Published 5 August 2020 | Version 1.0 FL20200730MMR
MYANMAR A? Flood Kachin, Shan (North) State and Sagaing, Mandalay, Magway Region Imagery analysis: 25 July 2020 | Published 5 August 2020 | Version 1.0 FL20200730MMR 94?40'0"E 95?20'0"E 96?0'0"E 96?40'0"E 97?20'0"E M O H N Y I N M Y I T K Y I N A H K A M T I Map location T A M U K A T H A K A C H I N B H A M O M Y A N M A R N " 0 ' 0 ? N 4 " 2 0 ' 0 ? 4 2 M AW L A I K K A W L I N M U S E M O N G M I T N " 0 ' 0 2 N ? " 3 0 ' 2 0 2 ? K A N B A L U Satellite detected water extent as 3 2 S A G A I N G of 25 July 2020 in central part of P A L A U N G S E L F - A D M I N I S T E R E D Z O N E Myanmar This map illustrates satellite-detected surface K A L E L A S H I O S H A N ( N O R T H ) waters over Kachin, Shan (North) State and MOGOK Sagaing, Mandalay, Magway Region of Myanmar as observed from a Terra(MODIS) L A S H I O N " 0 image acquired on 25 July 2020 due to the ' S H W E B O 0 4 N ? " 2 0 ' 2 current monsoon rains. -

Fact Book of Political Parties in Myanmar
Myanmar Development Research (MDR) (Present) Enlightened Myanmar Research (EMR) Wing (3), Room (A-305) Thitsar Garden Housing. 3 Street , 8 Quarter. South Okkalarpa Township. Yangon, Myanmar +951 562439 Acknowledgement of Myanmar Development Research This edition of the “Fact Book of Political Parties in Myanmar (2010-2012)” is the first published collection of facts and information of political parties which legally registered at the Union Election Commission since the pre-election period of Myanmar’s milestone 2010 election and the post-election period of the 2012 by-elections. This publication is also an important milestone for Myanmar Development Research (MDR) as it is the organization’s first project that was conducted directly in response to the needs of civil society and different stakeholders who have been putting efforts in the process of the political transition of Myanmar towards a peaceful and developed democratic society. We would like to thank our supporters who made this project possible and those who worked hard from the beginning to the end of publication and launching ceremony. In particular: (1) Heinrich B�ll Stiftung (Southeast Asia) for their support of the project and for providing funding to publish “Fact Book of Political Parties in Myanmar (2010-2012)”. (2) Party leaders, the elected MPs, record keepers of the 56 parties in this book who lent their valuable time to contribute to the project, given the limited time frame and other challenges such as technical and communication problems. (3) The Chairperson of the Union Election Commission and all the members of the Commission for their advice and contributions. -

Cases Related to COVID-19 Pandemic
Cases Related to COVID-19 Pandemic The Assistance Association for Political Prisoners (AAPP) has documented cases in relation to the COVID-19 Pandemic. According to our documentation from March to end of April, a total of 670 people have been charged and punished in Burma during the pandemic. The detailed information is shown below: (455) under Section 188 of the Penal Code and (18) under Section 18 of the Prevention and Control of Communicable Diseases Law are facing trials and serving sentences for failing abide-by the night curfew In addition, (166) are charged and convicted under Section 25, 26, 26(a), 27, 28(b), 30(a) (b) of the Natural Disaster Management Law and Section 15 and 18 of the Prevention and Control of Communicable Diseases Law and (2) are awaiting trial inside and outside prison under Section 16(c) of the Narcotic Drugs and Psychotropic Substances Law for failing to comply with the quarantine measures. Moreover, (3) under Sections 325,114 of the Penal Code, (4) under Sections 294, 506, 353, 324 of the Penal Code, (11) under Sections 333, 323, 427, 506, 114 of the Penal Code, (1) under Sections 333, 506, 294 of the Penal Code, (1) under Section 19 of the Peaceful Assembly and Peaceful Procession Law, (2) under Sections 336, 353, 294, 114 of the Penal Code, (1) under Sections 353, 506, 323, 294 of the Penal Code and (3) under Section 295(a) of the Penal Code are awaiting trial inside and outside prison and (2) under Section 47 of the Police Act and (1) under Section 5(1) of the Foreign Registration Act are serving the sentences for contravention of specified orders.