Two Novel ECHS1 Variants, Affecting Splicing and Reducing Enzyme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Differential Mitochondrial Proteomic Analysis of A549 Cells Infected With
Yang et al. Virol J (2021) 18:39 https://doi.org/10.1186/s12985-021-01512-4 RESEARCH Open Access Diferential mitochondrial proteomic analysis of A549 cells infected with avian infuenza virus subtypes H5 and H9 Yuting Yang1, Yun Zhang1, Changcheng Yang1, Fang Fang1, Ying Wang1, Haiyan Chang1*, Ze Chen1,2* and Ping Chen1* Abstract Background: Both the highly pathogenic avian infuenza (HPAI) H5N1 and low pathogenic avian infuenza (LPAI) H9N2 viruses have been reported to cross species barriers to infect humans. H5N1 viruses can cause severe damage and are associated with a high mortality rate, but H9N2 viruses do not cause such outcomes. Our purpose was to use proteomics technology to study the diferential expression of mitochondrial-related proteins related to H5N1 and H9N2 virus infections. Methods: According to the determined viral infection titer, A549 cells were infected with 1 multiplicity of infec- tion virus, and the mitochondria were extracted after 24 h of incubation. The protein from lysed mitochondria was analyzed by the BCA method to determine the protein concentration, as well as SDS-PAGE (preliminary analysis), two-dimensional gel electrophoresis, and mass spectrometry. Diferential protein spots were selected, and Western blotting was performed to verify the proteomics results. The identifed proteins were subjected to GO analysis for subcellular localization, KEGG analysis for functional classifcation and signaling pathways assessment, and STRING analysis for functional protein association network construction. Results: In the 2-D gel electrophoresis analysis, 227 protein spots were detected in the H5N1-infected group, and 169 protein spots were detected in the H9N2-infected group. Protein spots were further subjected to mass spectrom- etry identifcation and removal of redundancy, and 32 diferentially expressed proteins were identifed. -
Blueprint Genetics ECHS1 Single Gene Test
ECHS1 single gene test Test code: S00619 Phenotype information Mitochondrial short-chain enoyl-CoA hydratase 1 deficiency Alternative gene names SCEH Panels that include the ECHS1 gene Epileptic Encephalopathy Panel Fatty Acid Oxidation Syndrome Panel Comprehensive Epilepsy Panel Beyond Paediatric Epilepsy Panel – for Europe and Middle East Comprehensive Metabolism Panel Test Strengths The strengths of this test include: CAP accredited laboratory CLIA-certified personnel performing clinical testing in a CLIA-certified laboratory Powerful sequencing technologies, advanced target enrichment methods and precision bioinformatics pipelines ensure superior analytical performance Careful construction of clinically effective and scientifically justified gene panels Our Nucleus online portal providing transparent and easy access to quality and performance data at the patient level Our publicly available analytic validation demonstrating complete details of test performance ~2,000 non-coding disease causing variants in our clinical grade NGS assay for panels (please see ‘Non-coding disease causing variants covered by this test’) Our rigorous variant classification scheme Our systematic clinical interpretation workflow using proprietary software enabling accurate and traceable processing of NGS data Our comprehensive clinical statements Test Limitations This test does not detect the following: Complex inversions Gene conversions Balanced translocations Mitochondrial DNA variants Repeat expansion disorders unless specifically mentioned Non-coding -

Inactivation of the AMPK–GATA3–ECHS1 Pathway Induces Fatty Acid Synthesis That Promotes Clear Cell Renal Cell Carcinoma Grow
Published OnlineFirst November 5, 2019; DOI: 10.1158/0008-5472.CAN-19-1023 CANCER RESEARCH | TRANSLATIONAL SCIENCE Inactivation of the AMPK–GATA3–ECHS1 Pathway Induces Fatty Acid Synthesis That Promotes Clear Cell Renal Cell Carcinoma Growth A C Yuan-Yuan Qu1,2,3, Rui Zhao1, Hai-Liang Zhang1,3, Qian Zhou1, Fu-Jiang Xu1,3, Xuan Zhang2, Wen-Hao Xu1,3, Ning Shao1,3, Shu-Xian Zhou1,2, Bo Dai1,3, Yao Zhu1,3, Guo-Hai Shi1,3, Yi-Jun Shen1,3, Yi-Ping Zhu1,3, Cheng-Tao Han1,3, Kun Chang1,3, Yan Lin1,2,4, Wei-Dong Zang5, Wei Xu1,2,4, Ding-Wei Ye1,3, Shi-Min Zhao1,2,4, and Jian-Yuan Zhao1,2,4 ABSTRACT ◥ The tumorigenic role and underlying mechanisms of lipid accu- expression of GATA3, a transcriptional activator of ECHS1. BCAA mulation, commonly observed in many cancers, remain insuffi- accumulation induced activation of mTORC1 and de novo FA ciently understood. In this study, we identified an AMP-activated synthesis, and promoted cell proliferation. Furthermore, GATA3 protein kinase (AMPK)–GATA-binding protein 3 (GATA3)– expression phenocopied ECHS1 in predicting ccRCC progression enoyl-CoA hydratase short-chain 1 (ECHS1) pathway that induces and patient survival. The AMPK–GATA3–ECHS1 pathway may lipid accumulation and promotes cell proliferation in clear cell renal offer new therapeutic approaches and prognostic assessment for cell carcinoma (ccRCC). Decreased expression of ECHS1, which is ccRCC in the clinic. responsible for inactivation of fatty acid (FA) oxidation and acti- vation of de novo FA synthesis, positively associated with ccRCC Significance: These findings uncover molecular mechanisms progression and predicted poor patient survival. -

Downloaded from the App Store and Nucleobase, Nucleotide and Nucleic Acid Metabolism 7 Google Play
Hoytema van Konijnenburg et al. Orphanet J Rare Dis (2021) 16:170 https://doi.org/10.1186/s13023-021-01727-2 REVIEW Open Access Treatable inherited metabolic disorders causing intellectual disability: 2021 review and digital app Eva M. M. Hoytema van Konijnenburg1†, Saskia B. Wortmann2,3,4†, Marina J. Koelewijn2, Laura A. Tseng1,4, Roderick Houben6, Sylvia Stöckler‑Ipsiroglu5, Carlos R. Ferreira7 and Clara D. M. van Karnebeek1,2,4,8* Abstract Background: The Treatable ID App was created in 2012 as digital tool to improve early recognition and intervention for treatable inherited metabolic disorders (IMDs) presenting with global developmental delay and intellectual disabil‑ ity (collectively ‘treatable IDs’). Our aim is to update the 2012 review on treatable IDs and App to capture the advances made in the identifcation of new IMDs along with increased pathophysiological insights catalyzing therapeutic development and implementation. Methods: Two independent reviewers queried PubMed, OMIM and Orphanet databases to reassess all previously included disorders and therapies and to identify all reports on Treatable IDs published between 2012 and 2021. These were included if listed in the International Classifcation of IMDs (ICIMD) and presenting with ID as a major feature, and if published evidence for a therapeutic intervention improving ID primary and/or secondary outcomes is avail‑ able. Data on clinical symptoms, diagnostic testing, treatment strategies, efects on outcomes, and evidence levels were extracted and evaluated by the reviewers and external experts. The generated knowledge was translated into a diagnostic algorithm and updated version of the App with novel features. Results: Our review identifed 116 treatable IDs (139 genes), of which 44 newly identifed, belonging to 17 ICIMD categories. -

A High-Throughput Approach to Uncover Novel Roles of APOBEC2, a Functional Orphan of the AID/APOBEC Family
Rockefeller University Digital Commons @ RU Student Theses and Dissertations 2018 A High-Throughput Approach to Uncover Novel Roles of APOBEC2, a Functional Orphan of the AID/APOBEC Family Linda Molla Follow this and additional works at: https://digitalcommons.rockefeller.edu/ student_theses_and_dissertations Part of the Life Sciences Commons A HIGH-THROUGHPUT APPROACH TO UNCOVER NOVEL ROLES OF APOBEC2, A FUNCTIONAL ORPHAN OF THE AID/APOBEC FAMILY A Thesis Presented to the Faculty of The Rockefeller University in Partial Fulfillment of the Requirements for the degree of Doctor of Philosophy by Linda Molla June 2018 © Copyright by Linda Molla 2018 A HIGH-THROUGHPUT APPROACH TO UNCOVER NOVEL ROLES OF APOBEC2, A FUNCTIONAL ORPHAN OF THE AID/APOBEC FAMILY Linda Molla, Ph.D. The Rockefeller University 2018 APOBEC2 is a member of the AID/APOBEC cytidine deaminase family of proteins. Unlike most of AID/APOBEC, however, APOBEC2’s function remains elusive. Previous research has implicated APOBEC2 in diverse organisms and cellular processes such as muscle biology (in Mus musculus), regeneration (in Danio rerio), and development (in Xenopus laevis). APOBEC2 has also been implicated in cancer. However the enzymatic activity, substrate or physiological target(s) of APOBEC2 are unknown. For this thesis, I have combined Next Generation Sequencing (NGS) techniques with state-of-the-art molecular biology to determine the physiological targets of APOBEC2. Using a cell culture muscle differentiation system, and RNA sequencing (RNA-Seq) by polyA capture, I demonstrated that unlike the AID/APOBEC family member APOBEC1, APOBEC2 is not an RNA editor. Using the same system combined with enhanced Reduced Representation Bisulfite Sequencing (eRRBS) analyses I showed that, unlike the AID/APOBEC family member AID, APOBEC2 does not act as a 5-methyl-C deaminase. -

Attenuation of Enoyl Coenzyme a Hydratase 1 Expression in Colorectal Cancer Cells Using Small Interfering RNA Inhibits Cell Proliferation and Migration
470 MOLECULAR MEDICINE REPORTS 12: 470-474, 2015 Attenuation of enoyl coenzyme A hydratase 1 expression in colorectal cancer cells using small interfering RNA inhibits cell proliferation and migration QING-MEI ZHAO1*, FEI KUANG2*, HAN WU3 and YU-HAO ZHANG3 1Department of Oncology, Sichuan Mianyang 404 Hospital, Mianyang, Sichuan 621000; 2Department of General Surgery, Changhai Hospital of The Second Military Medical University, Shanghai 200433; 3Department of General Surgery, The 1745th Hospital of the PLA, Zhangzhou, Fujian 562001, P.R. China Received March 23, 2014; Accepted January 29, 2015 DOI: 10.3892/mmr.2015.3418 Abstract. Colorectal cancer is one of the most commonly cell proliferation and migration via activation of Akt- and diagnosed types of cancer and is a leading cause of GSK3β-associated signaling pathways. cancer-associated mortality worldwide. Short chain enoyl coenzyme A hydratase 1 (ECHS1) is an important gene Introduction involved in the mitochondrial fatty acid β-oxidation pathway. In addition, ECHS1 has been implicated in a variety of Colorectal cancer is one of the most commonly diagnosed types cancers, including breast, prostate, colon and liver cancer. of cancer and is a leading cause of cancer-associated mortality The aim of the present study was to examine the expression worldwide, particularly among populations in Eastern Asia, of ECHS1 in the human HCT-8 colorectal cancer cell line. Eastern Europe and South America (1,2). Risk factors for The results showed that ECHS1 expression was significantly colorectal cancer include infection, cigarette smoking, alcohol increased in poorly-differentiated cells compared with that consumption, diet and genetic variations (3). Although certain in well-differentiated cells. -

Genome Informatics
Joint Cold Spring Harbor Laboratory/Wellcome Trust Conference GENOME INFORMATICS September 15–September 19, 2010 View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Cold Spring Harbor Laboratory Institutional Repository Joint Cold Spring Harbor Laboratory/Wellcome Trust Conference GENOME INFORMATICS September 15–September 19, 2010 Arranged by Inanc Birol, BC Cancer Agency, Canada Michele Clamp, BioTeam, Inc. James Kent, University of California, Santa Cruz, USA SCHEDULE AT A GLANCE Wednesday 15th September 2010 17.00-17.30 Registration – finger buffet dinner served from 17.30-19.30 19.30-20:50 Session 1: Epigenomics and Gene Regulation 20.50-21.10 Break 21.10-22.30 Session 1, continued Thursday 16th September 2010 07.30-09.00 Breakfast 09.00-10.20 Session 2: Population and Statistical Genomics 10.20-10:40 Morning Coffee 10:40-12:00 Session 2, continued 12.00-14.00 Lunch 14.00-15.20 Session 3: Environmental and Medical Genomics 15.20-15.40 Break 15.40-17.00 Session 3, continued 17.00-19.00 Poster Session I and Drinks Reception 19.00-21.00 Dinner Friday 17th September 2010 07.30-09.00 Breakfast 09.00-10.20 Session 4: Databases, Data Mining, Visualization and Curation 10.20-10.40 Morning Coffee 10.40-12.00 Session 4, continued 12.00-14.00 Lunch 14.00-16.00 Free afternoon 16.00-17.00 Keynote Speaker: Alex Bateman 17.00-19.00 Poster Session II and Drinks Reception 19.00-21.00 Dinner Saturday 18th September 2010 07.30-09.00 Breakfast 09.00-10.20 Session 5: Sequencing Pipelines and Assembly 10.20-10.40 -

Novel ECHS1 Mutations in Leigh Syndrome Identified by Whole
Sun et al. BMC Medical Genetics (2020) 21:149 https://doi.org/10.1186/s12881-020-01083-1 CASE REPORT Open Access Novel ECHS1 mutations in Leigh syndrome identified by whole-exome sequencing in five Chinese families: case report Dan Sun1†, Zhimei Liu2†, Yongchu Liu3, Miaojuan Wu4, Fang Fang2*, Xianbo Deng5* , Zhisheng Liu1, Liang Song6, Kei Murayama7, Chunhua Zhang8 and Yuanyuan Zhu3 Abstract Background: Short-chain enoyl-CoA hydratase deficiency (ECHS1D), also known as ECHS1 deficiency, is a rare inborn metabolic disorder with clinical presentations characterized by Leigh syndrome (LS). Thirty-four different pathogenic mutations have been identified from over 40 patients to date. Case presentation: Here, we report five Chinese patients with clinical syndromes typified as LS. Despite different initial symptoms, all patients presented developmental regression, dystonia, common radiological features such as symmetrical bilateral brain abnormalities, and similar metabolic results such as elevated plasma lactate and 2,3- dihydroxy-2-methylbutyrate. Utilizing whole-exome sequencing (WES), we identified eight distinct variants in ECHS1, with six novel variants, and the remaining two variants have been previously reported. Interestingly, one of the six novel variants, c.463G > A (p.Gly155Ser), was detected in three patients from unrelated families, suggesting a potential founder effect already described for a few mutations in LS. Incorporating both genetic analysis and medical results, including magnetic resonance imaging (MRI), electroencephalography (EEG), and biochemical testing, our study enriched the mutation spectrum of the ECHS1 gene and confirmed the phenotypic presentations of LS. Conclusions: The severity of ECHS1 deficiency seems to vary. It was affected by both genetics and external environmental factors that lead to increased metabolism. -
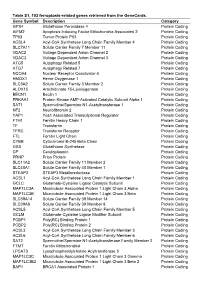
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

Differential Expression Gene Symbol Upregulated
Table S1. 1658 differential expressed genes with P-value < 0.05 in myeloid dendritic cells patients with all ergies compared to healthy controls. Differential Gene Symbol Expression Upregulated KIAA1217, RP11-111M22.2, RP11-21M24.2, FAM221B, TRIM9, CNKSR3, LRIT3, (N=771) RP11-26J3.1, RP11-708J19.1, RPS3AP35, AC096574.4, RBPMS, JPH3, RASGRF1, RP11-118E18.4, TPPP, KCNJ9, ARMC12, TUBB8P7, KCND3, CTD-2083E4.4, SLCO5A1, EGLN3, NOS3, RPS3AP40, OR10A4, AC007551.2, RP11-110I1.12, ZNF732, RP4-800G7.3, RNFT2, SFXN2, SEPT5, UFSP1, KRT8P26, RP11- 634H22.1, RP11-357G3.1, CTC-487M23.5, RP11-804H8.6, ROPN1L, E2F2, RP11- 983P16.4, SOX12, KRTAP16-1, FAM188B, TTC28, CTB-66B24.1, PLS1, SHF, ESR1, SOCS2, MNS1, GPR55, RP11-1020A11.2, C4orf32, BHLHE22, RP11- 63E5.6, SIGLEC15, FGFBP3, AP000692.10, CTD-2357A8.3, RP1-102E24.6, ZC4H2, AC074367.1, WDR86-AS1, YPEL1, HOXB-AS1, RP3-522P13.2, OR7E47P, AC068039.4, NUDT8, IBA57, PPP1R3G, CACNB3, KB-1460A1.1, IQCJ-SCHIP1-AS1, CRHR2, CD27-AS1, RP11-368J22.2, MANSC4, FITM2, AC002467.7, RPS5P2, SNHG17, GCAT, C10orf91, CTB-61M7.1, ATP8A2P2, RP11-50E11.2, TFAP4, CTD-2060C23.1, MED9, RP11-583F2.1, GAPDHP62, RN7SL801P, CYB5RL, ALG14, IGLV5-52, AC106801.1, RP11-403A21.3, LAD1, EARS2, NEURL3, DUSP14, RP11-116K4.1, PKNOX1, RP11-248J23.5, ZNF730, PSMF1, PINLYP, HOXA10, PTMAP8, RNLS, NANOGP7, FOXD1, AIFM2, KCNJ14, AC114730.8, RP11-804H8.5, C1orf109, PANK1, RPL32P26, RP11- 528A10.2, KL, METTL21B, CTD-2186M15.1, UBE3D, SMARCA5-AS1, SCARF2, AC000003.2, AC013470.6, PEX10, LRP11, ACTBP14, RP11-93B14.5, MIR1182, LIMCH1, IFI27L1, FSTL3, -

Deficiency of ECHS1 Causes Mitochondrial Encephalopathy With
RESEARCH ARTICLE Deficiency of ECHS1 causes mitochondrial encephalopathy with cardiac involvement Tobias B. Haack1,2,a, Christopher B. Jackson3, Kei Murayama4, Laura S. Kremer1,2, Andre Schaller5, Urania Kotzaeridou6, Maaike C. de Vries7, Gudrun Schottmann8, Saikat Santra9, Boriana Buchner€ 10, Thomas Wieland1,2, Elisabeth Graf1,2, Peter Freisinger11, Sandra Eggimann3, Akira Ohtake12, Yasushi Okazaki13,14, Masakazu Kohda13, Yoshihito Kishita14, Yoshimi Tokuzawa14, Sascha Sauer15, Yasin Memari16, Anja Kolb-Kokocinski16, Richard Durbin16, Oswald Hasselmann17, Kirsten Cremer18, Beate Albrecht19, Dagmar Wieczorek19, Hartmut Engels18, Dagmar Hahn3, Alexander M. Zink18, Charlotte L. Alston20, Robert W. Taylor20, Richard J. Rodenburg7, Regina Trollmann21, Wolfgang Sperl22, Tim M. Strom1,2, Georg F. Hoffmann6, Johannes A. Mayr22, Thomas Meitinger1,2,23,24, Ramona Bolognini5, Markus Schuelke8, Jean-Marc Nuoffer3,a, Stefan Kolker€ 6,a, Holger Prokisch1,2,a, & Thomas Klopstock10,23,24,a 1Institute of Human Genetics, Technische Universitat€ Munchen,€ 81675, Munich, Germany 2Institute of Human Genetics, Helmholtz Zentrum Munchen,€ German Research Center for Environmental Health, 85764, Neuherberg, Germany 3Institute of Clinical Chemistry and University Children’s Hospital, University of Bern, 3010, Bern, Switzerland 4Department of Metabolism, Chiba Children’s Hospital, Chiba, 266-0007, Japan 5Division of Human Genetics, Department of Pediatrics, University of Bern, 3010, Bern, Switzerland 6Divisions of Inherited Metabolic Disease and Neuropediatrics,