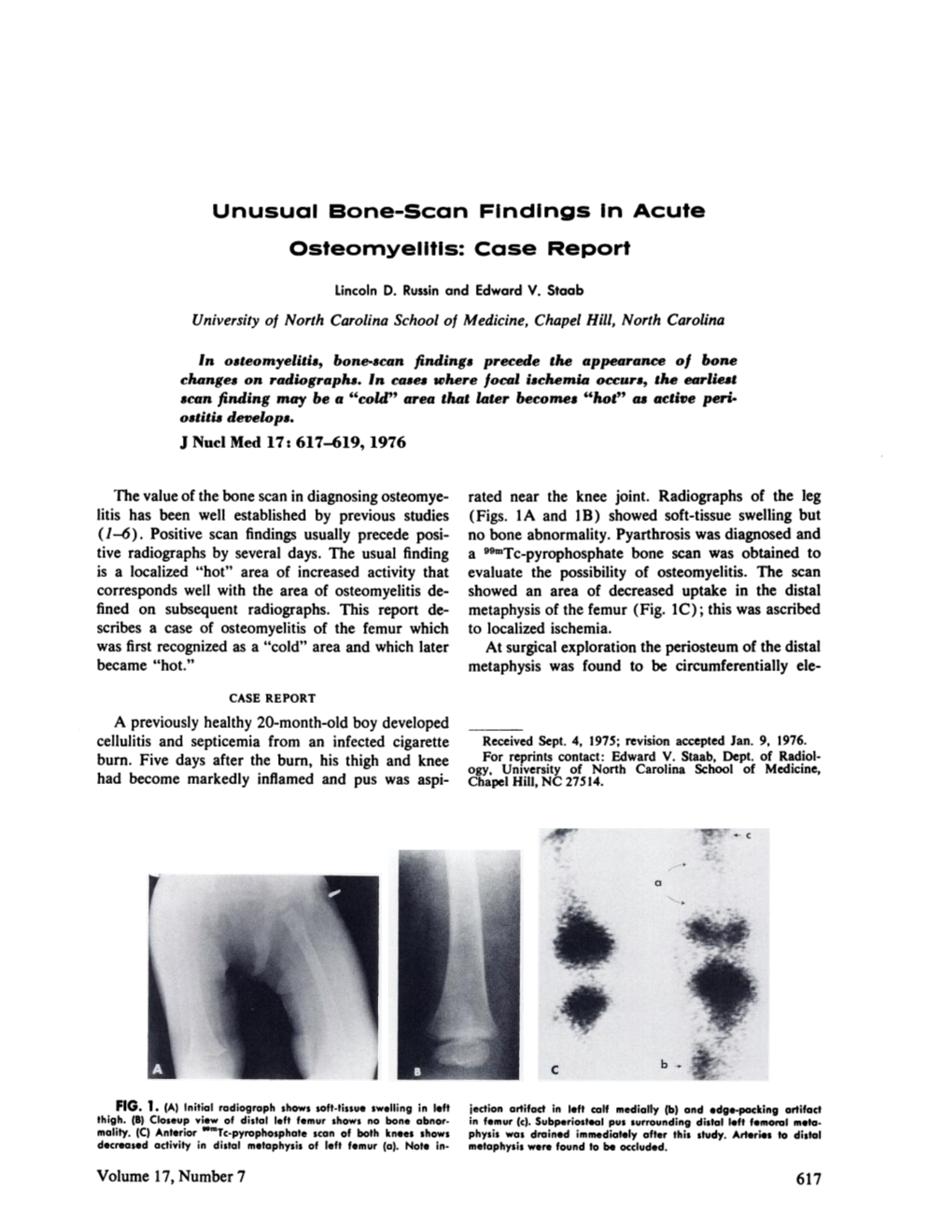
Unusual Bone—Scan Findings in Acute Osteomyelitis: Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paleopathological Analysis of a Sub-Adult Allosaurus Fragilis (MOR
Paleopathological analysis of a sub-adult Allosaurus fragilis (MOR 693) from the Upper Jurassic Morrison Formation with multiple injuries and infections by Rebecca Rochelle Laws A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science in Earth Sciences Montana State University © Copyright by Rebecca Rochelle Laws (1996) Abstract: A sub-adult Allosaurus fragilis (Museum of the Rockies specimen number 693 or MOR 693; "Big Al") with nineteen abnormal skeletal elements was discovered in 1991 in the Upper Jurassic Morrison Formation in Big Horn County, Wyoming at what became known as the "Big Al" site. This site is 300 meters northeast of the Howe Quarry, excavated in 1934 by Barnum Brown. The opisthotonic position of the allosaur indicated that rigor mortis occurred before burial. Although the skeleton was found within a fluvially-deposited sandstone, the presence of mud chips in the sandstone matrix and virtual completeness of the skeleton showed that the skeleton was not transported very far, if at all. The specific goals of this study are to: 1) provide a complete description and analysis of the abnormal bones of the sub-adult, male, A. fragilis, 2) develop a better understanding of how the bones of this allosaur reacted to infection and trauma, and 3) contribute to the pathological bone database so that future comparative studies are possible, and the hypothesis that certain abnormalities characterize taxa may be evaluated. The morphology of each of the 19 abnormal bones is described and each disfigurement is classified as to its cause: 5 trauma-induced; 2 infection-induced; 1 trauma- and infection-induced; 4 trauma-induced or aberrant, specific origin unknown; 4 aberrant; and 3 aberrant, specific origin unknown. -

WHO Manual of Diagnostic Imaging Radiographic Anatomy and Interpretation of the Musculoskeletal System
The WHO manual of diagnostic imaging Radiographic Anatomy and Interpretation of the Musculoskeletal System Editors Harald Ostensen M.D. Holger Pettersson M.D. Authors A. Mark Davies M.D. Holger Pettersson M.D. In collaboration with F. Arredondo M.D., M.R. El Meligi M.D., R. Guenther M.D., G.K. Ikundu M.D., L. Leong M.D., P. Palmer M.D., P. Scally M.D. Published by the World Health Organization in collaboration with the International Society of Radiology WHO Library Cataloguing-in-Publication Data Davies, A. Mark Radiography of the musculoskeletal system / authors : A. Mark Davies, Holger Pettersson; in collaboration with F. Arredondo . [et al.] WHO manuals of diagnostic imaging / editors : Harald Ostensen, Holger Pettersson; vol. 2 Published by the World Health Organization in collaboration with the International Society of Radiology 1.Musculoskeletal system – radiography 2.Musculoskeletal diseases – radiography 3.Musculoskeletal abnormalities – radiography 4.Manuals I.Pettersson, Holger II.Arredondo, F. III.Series editor: Ostensen, Harald ISBN 92 4 154555 0 (NLM Classification: WE 141) The World Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. Applications and enquiries should be addressed to the Office of Publications, World Health Organization, CH-1211 Geneva 27, Switzerland, which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © World Health Organization 2002 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. -

Osteochondrosis – Primary Epiphyseal (Articular/Subchondral) Lesion Can Heal Or Can Progress
60 120 180 1 distal humeral condyles 2 medial epicondyle 3 proximal radial epiphysis 4 anconeal process Lab Ret study N=1018 . Normal . Affected . Total 688 (67.6%) . Total 330 (32.4%) . Male 230 (62.2%) . Male 140 (37.8%) . Female 458 (70.7%) . Female 190 (29.3%) Affected dogs N=330 1affected site - 250 (75.7%) 2 affected sites - 68 (20.6%) 3 affected sites - 12 (3.6%) immature skeletal diseases denis novak technique for skeletal radiography tissue < 12 cm “non-grid” (“table-top”) technique “high detail” system radiation safety diagnosis X – rays examination Ultrasound CT bilateral lesions - clinical signs ? unilateral present > one type of lesion 2ry arthrosis Common Osteochondrosis – primary epiphyseal (articular/subchondral) lesion can heal or can progress Osteochondritis dissecans – free articular fragment will progress Arthrosis Osteochondrosis talus / tarsus Lumbosacral OCD Lumbosacral OCD Inflammatory diseases Panosteitis – non infectious Hypertrophic osteodystrophy (HOD) – perhaps infectious Osteomyelitis - infectious Panosteitis New medullary bone Polyostotic Multiple lesions in one bone Symmetrical or nonsymmetrical Sclerotic pattern B I L A T E R A L periosteal new bone forms with chronicity Cross sections of a tibia different locations Hypertrophic osteodystrophy (HOD) Dogs are systemically ill, febrile, anorectic, reluctant to walk most will recover Radiographic changes of HOD . Polyostotic . Metaphyseal . Symmetrical . Changes of lesion Early Mid Late lytic “plates” in acute case HOD - 4 m ret – lesions are present -

Musculoskeletal Radiology
MUSCULOSKELETAL RADIOLOGY Developed by The Education Committee of the American Society of Musculoskeletal Radiology 1997-1998 Charles S. Resnik, M.D. (Co-chair) Arthur A. De Smet, M.D. (Co-chair) Felix S. Chew, M.D., Ed.M. Mary Kathol, M.D. Mark Kransdorf, M.D., Lynne S. Steinbach, M.D. INTRODUCTION The following curriculum guide comprises a list of subjects which are important to a thorough understanding of disorders that affect the musculoskeletal system. It does not include every musculoskeletal condition, yet it is comprehensive enough to fulfill three basic requirements: 1.to provide practicing radiologists with the fundamentals needed to be valuable consultants to orthopedic surgeons, rheumatologists, and other referring physicians, 2.to provide radiology residency program directors with a guide to subjects that should be covered in a four year teaching curriculum, and 3.to serve as a “study guide” for diagnostic radiology residents. To that end, much of the material has been divided into “basic” and “advanced” categories. Basic material includes fundamental information that radiology residents should be able to learn, while advanced material includes information that musculoskeletal radiologists might expect to master. It is acknowledged that this division is somewhat arbitrary. It is the authors’ hope that each user of this guide will gain an appreciation for the information that is needed for the successful practice of musculoskeletal radiology. I. Aspects of Basic Science Related to Bone A. Histogenesis of developing bone 1. Intramembranous ossification 2. Endochondral ossification 3. Remodeling B. Bone anatomy 1. Cellular constituents a. Osteoblasts b. Osteoclasts 2. Non cellular constituents a. -

Osteomyelitis and Beyond
Osteomyelitis and Beyond R. Paul Guillerman, MD Associate Professor of Radiology Baylor College of Medicine Department of Pediatric Radiology Texas Children’s Hospital Houston, Texas Disclosure of Commercial Interest Neither I or a member of my immediate family have a financial relationship with a commercial organization that may have an interest in the content of this educational activity Objectives Review the characteristic imaging findings of pediatric musculoskeletal infections Focus particularly on MRI and invasive community- acquired Staphylococcus aureus (CA-SA) infections Present the differentiating features of potential mimics of infection Pediatric Osteomyelitis Classic clinical signs of fever, pain, swelling, and decreased mobility present in only a slight majority ↑ wbc count in 30-65% Blood cultures + in 30-75% Organism isolated by tissue biopsy in 50-85% ↑ ESR or fever in 70-90% ↑ CRP in 98% Conventional Approach to Imaging Acute Pediatric Musculoskeletal Infections Obtain bone scan if XR negative Reserve MRI for suspected spinal or pelvic osteomyelitis or lack of treatment response No longer optimal with advent of community-acquired Staphylococcus aureus (CA-SA) Community-Acquired Staphylococcus aureus (CA-SA) Distinctions from traditional Staphylococcus aureus: Community-acquired Affects otherwise healthy, immunocompetent children Can have rapid, invasive course Can be methicillin-resistant (MRSA) or sensitive (MSSA) Surgical debridement and drainage of associated abscesses and effusions is the mainstay of therapy Gadolinium-enhanced -

Bone Pathology for the Surgical Pathologist Disclosure Outline
5/25/19 Disclosure UCSF Current Issues in Pathology 2019 Company Relationship type Presage Biosciences Consultant Bone Pathology for the Surgical Pathologist Andrew Horvai MD PhD Clinical Professor, Pathology UCSF, San Francisco, CA Outline Diseases of bone • Approach to bone pathology Developmental • 1% Inflammatory Decalcification 4% • Osteomyelitis Metabolic • Avascular necrosis 17% Trauma Metastatic • Infected arthroplasty 76% 1% Neoplasm Primary <1% 1 5/25/19 Approach to bone diagnosis Approach to bone diagnosis Pathology Clinical Clinical Imaging Clinical Pathology Pathology Imaging Fracture Metastatic carcinoma Imaging Osteoporosis Myeloma, lymphoma Anatomy Composition osteon epiphysis Physis – Osteoid: (growth plate) • Collagen (mostly type I) metaphysis • Other proteins – Mineral periosteum • Carbonated calcium hydroxylapatite diaphysis trabeculae • Ca10(PO4)6(OH)2 Haversian canal bone Volkmann canal osteoid cortex medulla http://classes.midlandstech.edu 2 5/25/19 Decalcification Sample case • Bone = Protein + Carbonated Calcium hydroxylapatite [Ca10(PO4)6(OH)2] A 16 year old girl with travel to Costa Rica • Calcium crystals in tissue are hard to cut several weeks ago sustained an insect bite on • Acid decalcifiers destroy nucleic acids Product Constituents UCSF use the right leg. This evolved into a presumed Easy-Cut Formic Acid + HCl Non-neoplastic bone (toes etc.), septic arthritis which was managed with cortical bone antibiotics in Costa Rica. She returned to the US Formical2000 Formic Acid + EDTA Bone biopsy, intramedullary bone tumor with persistent right leg pain and sustained a Decal-Stat EDTA + HCl Bone marrow fracture of the left femur 3 days ago. Imaging IED Formic Acid + HCl + exchange Histology resin revealed a pathologic fracture which was Immunocal Formic acid Not used at UCSF biopsied. -

Bone and Soft Tissue Pathology Specimens and 127 Surgicals (Biopsies and Resections)
ANNUAL MEETING ABSTRACTS 11A the morphologic spectrum and etiology of DAD encountered during adult autopsy in (non-EWSR1) NR4A3 gene fusions (TAF15, TCF12) showed distinctive plasmacytoid an inner city teaching hospital. The diagnostic utility of post mortem lung culture was / rhabdoid morphology, with increased cellularity, cytologic atypia and high mitotic also evaluated. counts. Follow-up showed that only 1 of 16 patients with EWSR1-rearranged tumors Design: A retrospective study was performed on all adult autopsies from July 2010 to died of disease, in contrast to 3 of 7 (43%) patients with TAF15–rearranged tumors. July 2013 with fi nal histopathologic diagnosis of DAD. The histopathological features Conclusions: In conclusion, EMCs with variant NR4A3 gene fusions show a higher of DAD were re-evaluated by one autopsy pathologist and one pathology resident, incidence of rhabdoid phenotype, high grade morphology and a more aggressive based on the duration (exudative or proliferative phase), severity (bilateral/unilateral; outcome compared to the more common EWSR1-NR4A3 positive tumors. Furthermore, focal/extensive) and pattern (classical vs. acute fi brinous and organizing pneumonia as EWSR1 FISH break-apart assay is the preferred ancillary test to confi rm diagnosis aka AFOP). Clinical history, pre and post mortem laboratory investigations, including of EMC, tumors with variant NR4A3 gene fusions remain under-recognized and often postmortem lung culture (for bacteria, mycobacteria, fungi and virus) were reviewed misdiagnosed. FISH assay for NR4A3 rearrangements recognizes >95% of EMCs and to elucidate etiology. should be an additional tool in EWSR1-negative tumors. Results: 36 (16.2 %) cases showed histopathologic features of DAD out of 222 adult autopsies in the three year study period. -

Chronic Osteomyelitis in Children Evaluation and Management
CHRONIC OSTEOMYELITIS IN CHILDREN EVALUATION AND MANAGEMENT Ketut Siki Kawiyana Orthopaedi & Traumatology Subdivision Udayana University Sanglah General Hospital, Denpasar-Bali INTRODUCTION . Chronic osteomyelitis A daunting challenge to orthopaedic surgeons Often described as a disease that can never truly be cured . 10 to 30% of acute haematogenous osteomyelitis chronic osteomyelitis . Socio-economically underdeveloped regions high incidence of osteomyelitis in childhood. High incidence of Immunosuppression, Malnutrition trauma EPIDEMIOLOGY . Open fractures (3–50%) . The surgical management of closed fractures may (1–5%) . Primary hip or knee replacement (0.5‒2%) . Revision surgery (5%) . Second stage revision for periprosthetic infection (20%) . Overall complication of orthopaedic cases during the life-time of the prosthesis or implant (5%) EPIDEMIOLOGY DEFINITION Chronic osteomyelitis • Long-standing infection of the bone characterized by persistence of microorganisms, presence of sequestrum, low-grade inflammation, and fistulae . This definition originated from Observation acute Formation of a source of on- haematogenous Left untreated necrotic segments going or chronic osteomyelitis of bone infection Pathophysiology Inadequately treated hematogenous acute osteomyelitis or more commonly from a contiguous source of infection Inflammatory process causes obliteration and compression of the vascular channels. Part of the bone undergoes necrosis sequestrum Destruction of bone, and microorganisms propagate within the destroyed bone. -

Musculoskeletal Infection Extremities • Pathophysiology Nuttaya Pattamapaspong M.D
12/05/60 Topics • Role of imaging in extremity infection Musculoskeletal Infection Extremities • Pathophysiology Nuttaya Pattamapaspong M.D. Department of Radiology, Faculty of • Imaging features Medicine, Chiang Mai University, Chiang Mai, Thailand Detection of Infection Role of Imaging in Extremity Infection Challenges • Detection of infection • Musculoskeletal infections have multiple patterns of presentation. • Variability of the host immune response and • Determination the disease extent virulence of pathogen. • Clinical presentation & radiological features may • Guidance for intervention procedure similar to those of non-infectious process. • 50% of children having musculoskeletal infection are misdiagnosed as tumors or other conditions.* * Rasool MN, JBJS(Br) 2001 Detection of Infection Anatomy & infection Challenges • Superficial soft tissue • Increased immunocompromised patients infection (AIDs, chemotherapy, steroid, - Skin immunosupressive drugs) - Subcutaneous tissue • If untreated, musculoskeletal infection leads to - Superficial fascia fatal outcome or amputation. (Cellulitis) • Infectious diseases are common problems of the tropical region. 1 12/05/60 Anatomy & infection Detection of Infection Imaging of choices • Deep soft tissue infection • Radiographs - Deep/inter-compartment fascia (fasciitis) - Muscle (pyomyositis) • CT - Bursitis/tenosynovitis - Arthritis • US - Osteomyelitis • MRI Detection of Infection: Radiographs Detection of Infection: Radiographs • Osseous lesions: • Osseous lesions: • Radio opaque Bone destruction, -

Osteomyelitis Pathophysiology and Treatment Decisions 2017
Osteomyelitis David Shearer Dave Lowenberg Created June 2016 Definitions • Osteomyelitis – Infection involving bone • Acute osteomyelitis – Infection of short duration – Characterized by suppuration (i.e. abscess) but not biofilm – Systemic symptoms common Definitions • Chronic osteomyelitis – Long standing infection (weeks to years) – Characterized by necrotic bone and bacterial colonies in protein/polysaccharide matrix (biofilm) – Often no systemic symptoms • Occurs along spectrum with no clear time cutoff to separate acute vs. chronic infection Etiologies • Hematogenous – Metaphysis of long bones • Most common in children – Vertebral osteomyelitis • Contiguous spread – Post-traumatic • Open fractures • Infections associated with deep implants – Prosthetic Joint Infections • Vascular Insufficiency and/or Diabetes – Secondary to ulceration – Commonly affects the forefoot bones Epidemiology • Estimates vary widely, but overall increasing incidence in US – Increasing • Osteomyelitis from a contiguous focus of infection (e.g. post-trauma, post-surgery) • Osteomyelitis of the foot and ankle related to diabetes – Stable/Decreasing • Hematogenous osteomyelitis in children Kremers, et al. JBJS 2015 Pathogens • Staph aureus most common (45% in series by Kremers et al., JBJS, 2015) • Staph epidermidis and steptococcal species next most common • Diabetes more commonly polymicrobial Pathophysiology: Implant-associated osteomyelitis – Planktonic cells attach to metal substrate – Initial cells undergo apoptosis – “Sacrificial cells” become matrix -

Review of Adult Foot Radiology
4 Review of Adult Foot Radiology LAWRENCE OSHER In the workup of a hallux valgus deformity the practi- Metabolic disease (dystrophies included) tioner is often faced with unexpected radiographic Infections and inflammatory processes findings. Usually, the first course of action is to order Tumor and tumor-like conditions additional pedal studies, which may provide the addi- Degenerative disease and ischemic necrosis tional detail needed to help resolve or localize the apparent pathology. If the problem is within the pur- However, this approach is presumptive; not only is view of conventional radiography, a library text, if an understanding of these basic bone radiographic available, is often hurriedly consulted. changes clearly required, but one is expected to iden- It is clearly not possible to encompass all of pedal tify and then classify any lesion(s). Many radiographic radiology within the confines of a single chapter of bony abnormalities simply cannot be categorized at this volume. Designed for the physician already famil- first glance by the average physician, despite the ability iar with basic musculoskeletal radiographic terminol- to correctly describe the basic pathologic changes. For ogy, the following information will serve as a handy these practitioners, a more intuitive approach utilizing outline of foot pathology that may be encountered in clinical and laboratory data is required (studies clearly the routine workup of the patient with hallux valgus show improved accuracy in the reading of radiographs deformity. Particular effort has been given to simplify when appropriate clinical and laboratory data are pro- the process of generating basic differential diagnoses. vided). The following steps are recommended: Pictorial examples are provided throughout this chapter. -

Newsletter # 245, Mon, December 24, 2018
winter 2018 AMHE Newsletter december 24 Haitian Medical Association Abroad Association Medicale Haïtienne à l'Étranger Newsletter # 245 AMHE NEWSLETTER Editor in Chief: Maxime J-M Coles, MD Editorial Board: Rony Jean Mary, MD Reynald Altema, MD Technical Adviser: Jacques Arpin Chers lecteurs et lectrices de l’infolettre de la AMHE, In this number 2 - Words of the Editor, Maxime Coles,MD - Poème de Marlène Apollon - SAPHO Syndrome, Maxime Coles,MD - Poème de Dr Jean Serge Dorismond - Henry R Ford MD, MHA recently became Dean and Chief… - Dr. Brutus Maurice Dieudonne - La chronique de Rony Jean-Mary,M.D. - Sickle cell Clinic in Leogane - La chronique de Reynald Altéma,M.D. - Upcoming Events - AHDH’s Mission Report - Published on the AMHE Facebook page last two weeks - Outcomes of minority patients with very severe hypertension - And more... SAPHO Syndrome Maxime Coles MD SAPHO Syndrome (Acquired Hyperostosis 1987 by Chamot to describe this spectrum of Syndrome, Pustulosis, Hyperostosis and inflammatory bone disorder, often but not Osteomyelitis, Synovitis acne pustulosis always associated with dermatologic lesions. hyperostosis osteitis) is described as any Symptoms will vary from person to person. combination of Synovitis (inflammation of the People diagnosed with the disease may have joints), with acne, Pustulosis (thick yellow blisters different symptoms based on the human containing pus) often in the palms and soles, phenotype ontology (HPO). The information Hyperostosis (increase in bone substance) and collected is updated regularly with bone pain, Osteitis (inflammation of the bone). The cause of arthralgia, chest pain, cranio-fascial Sapho syndrome is unknown, but not fully osteosclerosis, Enthesitis (SC Joints).