Agenesis of the Corpus Callosum
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

The Genetic Heterogeneity of Brachydactyly Type A1: Identifying the Molecular Pathways
The genetic heterogeneity of brachydactyly type A1: Identifying the molecular pathways Lemuel Jean Racacho Thesis submitted to the Faculty of Graduate Studies and Postdoctoral Studies in partial fulfillment of the requirements for the Doctorate in Philosophy degree in Biochemistry Specialization in Human and Molecular Genetics Department of Biochemistry, Microbiology and Immunology Faculty of Medicine University of Ottawa © Lemuel Jean Racacho, Ottawa, Canada, 2015 Abstract Brachydactyly type A1 (BDA1) is a rare autosomal dominant trait characterized by the shortening of the middle phalanges of digits 2-5 and of the proximal phalange of digit 1 in both hands and feet. Many of the brachymesophalangies including BDA1 have been associated with genetic perturbations along the BMP-SMAD signaling pathway. The goal of this thesis is to identify the molecular pathways that are associated with the BDA1 phenotype through the genetic assessment of BDA1-affected families. We identified four missense mutations that are clustered with other reported BDA1 mutations in the central region of the N-terminal signaling peptide of IHH. We also identified a missense mutation in GDF5 cosegregating with a semi-dominant form of BDA1. In two families we reported two novel BDA1-associated sequence variants in BMPR1B, the gene which codes for the receptor of GDF5. In 2002, we reported a BDA1 trait linked to chromosome 5p13.3 in a Canadian kindred (BDA1B; MIM %607004) but we did not discover a BDA1-causal variant in any of the protein coding genes within the 2.8 Mb critical region. To provide a higher sensitivity of detection, we performed a targeted enrichment of the BDA1B locus followed by high-throughput sequencing. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

Abstracts Books 2014
TWENTY-FIFTH EUROPEAN MEETING ON DYSMORPHOLOGY 10 – 12 SEPTEMBER 2014 25th EUROPEAN MEETING ON DYSMORPHOLOGY LE BISCHENBERG WEDNESDAY 10th SEPTEMBER 5 p.m. to 7.30 p.m. Registration 7.30 p.m. to 8.30 p.m. Welcome reception 8.30 p.m. Dinner 9.30 p.m. Unknown THURSDAY 11th SEPTEMBER 8.15 a.m. Opening address 8.30 a.m. to 1.00 p.m. First session 1.00 p.m. Lunch 2.30 p.m. to 7.00 p.m. Second and third sessions 8.00 p.m. Dinner 9.00 p.m. to 11.00 p.m. Unknown FRIDAY 12th SEPTEMBER 8.30 a.m. to 1.00 p.m. Fourth and fifth sessions 1.00 p.m. Lunch 2.30 p.m. to 6.00 p.m. Sixth and seventh sessions 7.30 p.m. Dinner SATURDAY 13th SEPTEMBER Breakfast – Departure Note: This program is tentative and may be modified. WEDNESDAY 10th SEPTEMBER 9.30 UNKNOWN SESSION Chair: FRYNS J.P. H. VAN ESCH Case 1 H. VAN ESCH Case 2 H. JILANI, S. HIZEM, I. REJEB, F. DZIRI AND L. BEN JEMAA Developmental delay, dysmorphic features and hirsutism in a Tunisian girl. Cornelia de Lange syndrome? L. VAN MALDERGEM, C. CABROL, B. LOEYS, M. SALEH, Y. BERNARD, L. CHAMARD AND J. PIARD Megalophthalmos and thoracic great vessels aneurisms E. SCHAEFER AND Y. HERENGER An unknown diagnosis associating facial dysmorphism, developmental delay, posterior urethral valves and severe constipation P. RUMP AND T. VAN ESSEN What’s in the name G. MUBUNGU, A. LUMAKA, K. -
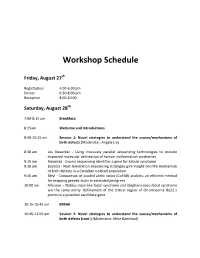
Workshop Schedule
Workshop Schedule Friday, August 27th Registration: 4:00‐6:30 pm Dinner 6:30‐8:00 pm Reception 8:00‐10:00 Saturday, August 28th 7:00‐8:15 am Breakfast: 8:15am Welcome and Introductions 8:30‐10:15 am Session 1: Novel strategies to understand the causes/mechanisms of birth defects (Moderator: Angela Lin) 8:30 am Les Biesecker ‐ Using massively parallel sequencing technologies to provide improved molecular delineation of human malformation syndromes 9:15 am Bamshad ‐ Exome sequencing identifies a gene for Kabuki syndrome 9:30 am Boycott ‐ Next‐Generation sequencing strategies give insight into the mechanism of birth defects in a Canadian isolated population 9:45 am Bleyl ‐ Comparison of pooled allelic ratios (CoPAR) analysis: an efficient method for mapping genetic traits in extended pedigrees 10:00 am Allanson – Nablus mask‐like facial syndrome and blepharo‐naso‐facial syndrome are the same entity. Refinement of the critical region of chromosome 8q22.1 points to a potential candidate gene 10:15‐10:45 am BREAK 10:45‐12:00 pm Session 2: Novel strategies to understand the causes/mechanisms of birth defects (cont.) (Moderator: Mike Bamshad) 10:45 am Krantz ‐ Applying novel genomic tools towards understanding an old chromosomal diagnosis: Using genome‐wide expression and SNP genotyping to identify the true cause of Pallister‐Killian syndrome 11:00 am Paciorkowski ‐ Bioinformatic analysis of published and novel copy number variants suggests candidate genes and networks for infantile spasms 11:15 am Bernier ‐ Identification of a novel Fibulin -

De Novo GLI3 Mutation in Acrocallosal Syndrome
804 SHORT REPORT J Med Genet: first published as 10.1136/jmg.39.11.804 on 1 November 2002. Downloaded from De novo GLI3 mutation in acrocallosal syndrome: broadening the phenotypic spectrum of GLI3 defects and overlap with murine models E Elson, R Perveen, D Donnai, S Wall,GCMBlack ............................................................................................................................. J Med Genet 2002;39:804–806 condition at birth and weighed 4240 g (90th-97th centile) Acrocallosal syndrome (ACS) is characterised by postaxial with an OFC of 39.5 cm (>97th centile). He had bilateral cleft polydactyly, hallux duplication, macrocephaly, and ab- lip and palate, a large anterior fontanelle extending down his sence of the corpus callosum, usually with severe develop- forehead, overriding coronal sutures, and small ears with mental delay. The condition overlaps with Greig uplifted lobes (fig 1A). Hypertelorism was confirmed by cephalopolysyndactyly syndrome (GCPS), an autosomal measurement and cranial MR showed agenesis of the corpus dominant disorder that results from mutations in the GLI3 callosum. His hands showed bilateral postaxial nubbins, a gene. Here we report a child with agenesis of the corpus broad thumb on the right hand, and a partially duplicated callosum and severe retardation, both cardinal features of thumb on the left. He also had 2/3 partial cutaneous syndac- ACS and rare in GCPS, who has a mutation in GLI3. tyly on the right and 3/4 partial cutaneous syndactyly on the Since others have excluded GLI3 in ACS, we suggest that left. There was a single flexor crease on the index finger of the ACS may represent a heterogeneous group of disorders right hand. -

Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel
Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel Overview Arthrogryposis or arthrogryposis multiplex congenita (AMC) is a group of nonprogressive conditions characterized by multiple joint contractures found throughout the body at birth. It usually appears as a feature of other neuromuscular conditions or part of systemic diseases. Primary cases may present prenatally with decreased fetal movements associated with joint contractures as well as brain abnormalities, decreased muscle bulk and polyhydramnios whereas secondary causes may present with isolated contractures. Congenital Myasthenic Syndromes (CMS) are a clinically and genetically heterogeneous group of disorders characterized by impaired neuromuscular transmission. Clinically they usually present with abnormal fatigability upon exertion, transient weakness of extra-ocular, facial, bulbar, truncal or limb muscles. Severity ranges from mild, phasic weakness, to disabling permanent weakness with respiratory difficulties and ultimately death. The mode of inheritance of these diseases typically follows and autosomal recessive pattern, although dominant forms can be seen. The Igenomix Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel can be as a tool for an accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved, and their high or intermediate penetrance. -

Joubert Syndrome and Related Disorders Precision Panel Overview Indications Clinical Utility
Joubert Syndrome and Related Disorders Precision Panel Overview Joubert Syndrome (JS) and Related Disorders (JSRD) are a group of ciliopathies characterized by mid-hindbrain malformation, developmental delay, hypotonia, oculomotor apraxia, and breathing abnormalities. Cilia play a crucial role in appropriate axonal growth and connectivity which are essential for functional wiring of the brain. The classic midbrain-hindbrain malformation is a hallmark image finding known as molar tooth sign. Joubert Syndrome and Related Disorders are a group of clinically and genetically heterogeneous disorders involving ciliopathy-related genes. Therefore, clinical manifestations have multiorgan involvement, mainly retinal dystrophy, hepatic fibrosis and polydactyly, among others. With the exception of rare X-linked recessive cases, Joubert Syndrome and Related Disorders follow an autosomal recessive inheritance pattern. The Igenomix Joubert Syndrome and Related Disorders Precision Panel can serve as a screening and diagnostic tool ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Joubert Syndrome and Related Disorders Precision Panel is indicated for those patients with clinical and/or imaging findings suggestive of Joubert Syndrome and Related Disorders presenting with the following manifestations: ‐ Hypotonia ‐ Ataxia ‐ Developmental delay ‐ Abnormal eye and tongue movements ‐ Respiratory control disturbances ‐ Polydactyly ‐ Cleft lip or palate ‐ Seizures Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. 1 - Early initiation of treatment involving a multidisciplinary team focusing on respiratory and feeding problems in neonates and infants. -

Blueprint Genetics Neuronal Migration Disorder Panel
Neuronal Migration Disorder Panel Test code: MA2601 Is a 59 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of neuronal migration disorder. About Neuronal Migration Disorder Neuronal migration disorders (NMDs) are a group of birth defects caused by the abnormal migration of neurons in the developing brain and nervous system. During development, neurons must migrate from the areas where they are originate to the areas where they will settle into their proper neural circuits. The structural abnormalities found in NMDs include schizencephaly, porencephaly, lissencephaly, agyria, macrogyria, polymicrogyria, pachygyria, microgyria, micropolygyria, neuronal heterotopias, agenesis of the corpus callosum, and agenesis of the cranial nerves. Mutations of many genes are involved in neuronal migration disorders, such as DCX in classical lissencephaly spectrum, TUBA1A in microlissencephaly with agenesis of the corpus callosum, and RELN and VLDLR in lissencephaly with cerebellar hypoplasia. Mutations in ARX cause a variety of phenotypes ranging from hydranencephaly or lissencephaly to early-onset epileptic encephalopathies, including Ohtahara syndrome and infantile spasms or intellectual disability with no brain malformations. Availability 4 weeks Gene Set Description Genes in the Neuronal Migration Disorder Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ACTB* Baraitser-Winter syndrome AD 55 60 ACTG1* Deafness, Baraitser-Winter syndrome AD 27 47 ADGRG1 -

A Large Duplication Involving the IHH Locus Mimics Acrocallosal Syndrome
European Journal of Human Genetics (2012) 20, 639–644 & 2012 Macmillan Publishers Limited All rights reserved 1018-4813/12 www.nature.com/ejhg ARTICLE A large duplication involving the IHH locus mimics acrocallosal syndrome Memnune Yuksel-Apak1, Nina Bo¨gershausen2,3, Barbara Pawlik2,3, Yun Li2,3, Selcuk Apak4, Oya Uyguner1, Esther Milz2,3, Gudrun Nu¨rnberg2,5, Birsen Karaman1, Ayan Gu¨lgo¨ren6, Karl-Heinz Grzeschik7, Peter Nu¨rnberg2,5,8,Hu¨lya Kayserili1 and Bernd Wollnik*,2,3,8 Indian hedgehog (Ihh) signaling is a major determinant of various processes during embryonic development and has a pivotal role in embryonic skeletal development. A specific spatial and temporal expression of Ihh within the developing limb buds is essential for accurate digit outgrowth and correct digit number. Although missense mutations in IHH cause brachydactyly type A1, small tandem duplications involving the IHH locus have recently been described in patients with mild syndactyly and craniosynostosis. In contrast, a B600-kb deletion 5¢ of IHH in the doublefoot mouse mutant (Dbf) leads to severe polydactyly without craniosynostosis, but with craniofacial dysmorphism. We now present a patient resembling acrocallosal syndrome (ACS) with extensive polysyndactyly of the hands and feet, craniofacial abnormalities including macrocephaly, agenesis of the corpus callosum, dysplastic and low-set ears, severe hypertelorism and profound psychomotor delay. Single-nucleotide polymorphism (SNP) array copy number analysis identified a B900-kb duplication of the IHH locus, which was confirmed by an independent quantitative method. A fetus from a second pregnancy of the mother by a different spouse showed similar craniofacial and limb malformations and the same duplication of the IHH-locus. -

Metopic and Sagittal Synostosis in Greig Cephalopolysyndactyly Syndrome: five Cases with Intragenic Mutations Or Complete Deletions of GLI3
European Journal of Human Genetics (2011) 19, 757–762 & 2011 Macmillan Publishers Limited All rights reserved 1018-4813/11 www.nature.com/ejhg ARTICLE Metopic and sagittal synostosis in Greig cephalopolysyndactyly syndrome: five cases with intragenic mutations or complete deletions of GLI3 Jane A Hurst1,2, Dagan Jenkins3, Pradeep C Vasudevan4, Maria Kirchhoff5, Flemming Skovby5, Claudine Rieubland6, Sabina Gallati6, Olaf Rittinger7, Peter M Kroisel8, David Johnson2, Leslie G Biesecker9 and Andrew OM Wilkie*,1,2,3 Greig cephalopolysyndactyly syndrome (GCPS) is a multiple congenital malformation characterised by limb and craniofacial anomalies, caused by heterozygous mutation or deletion of GLI3. We report four boys and a girl who were presented with trigonocephaly due to metopic synostosis, in association with pre- and post-axial polydactyly and cutaneous syndactyly of hands and feet. Two cases had additional sagittal synostosis. None had a family history of similar features. In all five children, the diagnosis of GCPS was confirmed by molecular analysis of GLI3 (two had intragenic mutations and three had complete gene deletions detected on array comparative genomic hybridisation), thus highlighting the importance of trigonocephaly or overt metopic or sagittal synostosis as a distinct presenting feature of GCPS. These observations confirm and extend a recently proposed association of intragenic GLI3 mutations with metopic synostosis; moreover, the three individuals with complete deletion of GLI3 were previously considered to have Carpenter syndrome, highlighting an important source of diagnostic confusion. European Journal of Human Genetics (2011) 19, 757–762; doi:10.1038/ejhg.2011.13; published online 16 February 2011 Keywords: trigonocephaly; metopic synostosis; sagittal synostosis; Greig cephalopolysyndactyly syndrome; GLI3; Carpenter syndrome INTRODUCTION (SHH) pathway. -

Carrier Screening Panel
Advancing Non-Invasive Healthcare Cell3TM Target: Carrier Screening Panel Detects 448 childhood recessive disorders DISORDER GENE DISEASE TYPE 2-Methylbutryl-CoA dehydrogenase deficiency ACADSB Metabolic 3-Hydroxy-3-methylglutaryl- CoA lyase deficiency HMGCL Metabolic 3-Hydroxyacyl- CoA dehydrogenase deficiency HADH Metabolic 3-Methylcrotonyl- CoA carboxylase 2 deficiency MCCC2 Metabolic 3-Methylglutaconic aciduria, i AUH Metabolic 3-Methylglutaconic aciduria, iii OPA3 Metabolic 3-Methylglutaconic aciduria, v DNAJC19 Metabolic α -Thalassemia/mental retardation syndrome, nondeletion, XLR ATRX ATRX Hematologic ABCD syndrome EDNRB Cutaneous Abetalipoproteinemia; ABL MTTP Metabolic Achalasia-Addisonianism-Alacrima syndrome; AAA AAAS Endocrine Achondrogenesis, Ib; ACG1b SLC26A2 Skeletal Achromatopsia 3; ACHM3 CNGB3 Ocular Acrocallosal syndrome; ACLS GLI3 Developmental Acyl-CoA dehydrogenase family, member 9, deficiency of ACAD9 Metabolic Acyl-CoA dehydrogenase, long-chain, deficiency of ACADL Metabolic Acyl-CoA dehydrogenase, medium-chain, deficiency of ACADM Metabolic Acyl-CoA dehydrogenase, short-chain, deficiency of ACADS Metabolic Acyl-CoA dehydrogenase, very long-chain, deficiency of ACADVL Metabolic Adrenal hyperplasia, congenital, due to 21-hydroxylase deficiency CYP21A2 Endocrine Adrenoleukodystrophy; ALD ABCD1 Neurological Afibrinogenemia, congenital FGA Hematologic Afibrinogenemia, congenital FGB Hematologic Afibrinogenemia, congenital FGG Hematologic Agammaglobulinemia, XLR, XLA BTK Immunodeficiency Agenesis of the corpus callosum