Metopic and Sagittal Synostosis in Greig Cephalopolysyndactyly Syndrome: five Cases with Intragenic Mutations Or Complete Deletions of GLI3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Second Family with the Bostontype Craniosynostosis Syndrome: Novel Mutation and Expansion of the Clinical Spectrum
CLINICAL REPORT Second Family With the Boston-Type Craniosynostosis Syndrome: Novel Mutation and Expansion of the Clinical Spectrum Alexander Janssen,1 Mohammad J. Hosen,2 Philippe Jeannin,3 Paul J. Coucke,2 Anne De Paepe,2 and Olivier M. Vanakker2* 1Department of Neurosurgery, Ghent University Hospital, Ghent, Belgium 2Center for Medical Genetics, Ghent University Hospital, Ghent, Belgium 3Department of Pediatrics, Jan Palfijn Hospital, Ghent, Belgium Manuscript Received: 11 January 2013; Manuscript Accepted: 3 May 2013 Craniosynostosis, caused by early fusion of one or more cranial sutures, can affect the coronal or lambdoid sutures, or include How to Cite this Article: premature fusion of the sagittal (scaphocephaly) or metopic Janssen A, Hosen MJ, Jeannin P, Coucke suture (trigonocephaly). Often occurring as isolated finding, PJ, De Paepe A, Vanakker OM. 2013. their co-existence in a craniosynostosis syndrome is infrequent. Second family with the Boston-type We describe a four-generation family with variable expression of craniosynostosis syndrome: Novel mutation a craniosynostosis phenotype with scaphocephaly and a partic- and expansion of the clinical spectrum. ularly severe trigonocephaly. Molecular analysis revealed a mis- sense mutation in the MSX2—associated with the Boston-type Am J Med Genet Part A 161A:2352–2357. craniosynostosis syndrome—affecting the same amino-acid res- idue as in the original Boston family. Besides unique features such as the cranial sutures involved, minor limb abnormalities isolated sagittal synostosis, accounting for more than half of all and incomplete penetrance, our patients share with the original reported cases. Premature fusion of the sagittal suture results in family autosomal dominant inheritance and the presence of decreased width and inverse elongation of the anteroposterior axis multiple endocranial erosions on CT imaging. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

The Genetic Heterogeneity of Brachydactyly Type A1: Identifying the Molecular Pathways
The genetic heterogeneity of brachydactyly type A1: Identifying the molecular pathways Lemuel Jean Racacho Thesis submitted to the Faculty of Graduate Studies and Postdoctoral Studies in partial fulfillment of the requirements for the Doctorate in Philosophy degree in Biochemistry Specialization in Human and Molecular Genetics Department of Biochemistry, Microbiology and Immunology Faculty of Medicine University of Ottawa © Lemuel Jean Racacho, Ottawa, Canada, 2015 Abstract Brachydactyly type A1 (BDA1) is a rare autosomal dominant trait characterized by the shortening of the middle phalanges of digits 2-5 and of the proximal phalange of digit 1 in both hands and feet. Many of the brachymesophalangies including BDA1 have been associated with genetic perturbations along the BMP-SMAD signaling pathway. The goal of this thesis is to identify the molecular pathways that are associated with the BDA1 phenotype through the genetic assessment of BDA1-affected families. We identified four missense mutations that are clustered with other reported BDA1 mutations in the central region of the N-terminal signaling peptide of IHH. We also identified a missense mutation in GDF5 cosegregating with a semi-dominant form of BDA1. In two families we reported two novel BDA1-associated sequence variants in BMPR1B, the gene which codes for the receptor of GDF5. In 2002, we reported a BDA1 trait linked to chromosome 5p13.3 in a Canadian kindred (BDA1B; MIM %607004) but we did not discover a BDA1-causal variant in any of the protein coding genes within the 2.8 Mb critical region. To provide a higher sensitivity of detection, we performed a targeted enrichment of the BDA1B locus followed by high-throughput sequencing. -
Dysmorphology and Dysfunction in the Brain and Calvarial Vault of Nonsyndromic Craniosynostosis
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine January 2013 Dysmorphology And Dysfunction In The rB ain And Calvarial Vault Of Nonsyndromic Craniosynostosis Joel Stanley Beckett Yale School of Medicine, [email protected] Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Beckett, Joel Stanley, "Dysmorphology And Dysfunction In The rB ain And Calvarial Vault Of Nonsyndromic Craniosynostosis" (2013). Yale Medicine Thesis Digital Library. 1781. http://elischolar.library.yale.edu/ymtdl/1781 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. Dysmorphology and Dysfunction in the Brain and Calvarial Vault of Nonsyndromic Craniosynostosis Yale University School of Medicine in Partial Fulfillment of the Requirements for the Degree of Doctor of Medicine by Joel Stanley Beckett 2013 Abstract Craniosynostosis is a premature pathologic fusion of one or more sutures in the calvarial vault. The six calvarial sutures are growth sites between adjacent intramembranous bones, which allow for flexibility during passage through the birth canal and accommodation for the growing brain. (1) Premature fusion results in obvious cranial morphologic abnormality and can be associated with elevated intracranial pressure, visual dysfunction, mental retardation and various forms of subtler learning disability. (2) A category of disease called isolated nonsyndromic craniosynostosis (NSC) represents nearly 85% of cases. -

Syndromic Ear Anomalies and Renal Ultrasounds
Syndromic Ear Anomalies and Renal Ultrasounds Raymond Y. Wang, MD*; Dawn L. Earl, RN, CPNP‡; Robert O. Ruder, MD§; and John M. Graham, Jr, MD, ScD‡ ABSTRACT. Objective. Although many pediatricians cific MCA syndromes that have high incidences of renal pursue renal ultrasonography when patients are noted to anomalies. These include CHARGE association, Townes- have external ear malformations, there is much confusion Brocks syndrome, branchio-oto-renal syndrome, Nager over which specific ear malformations do and do not syndrome, Miller syndrome, and diabetic embryopathy. require imaging. The objective of this study was to de- Patients with auricular anomalies should be assessed lineate characteristics of a child with external ear malfor- carefully for accompanying dysmorphic features, includ- mations that suggest a greater risk of renal anomalies. We ing facial asymmetry; colobomas of the lid, iris, and highlight several multiple congenital anomaly (MCA) retina; choanal atresia; jaw hypoplasia; branchial cysts or syndromes that should be considered in a patient who sinuses; cardiac murmurs; distal limb anomalies; and has both ear and renal anomalies. imperforate or anteriorly placed anus. If any of these Methods. Charts of patients who had ear anomalies features are present, then a renal ultrasound is useful not and were seen for clinical genetics evaluations between only in discovering renal anomalies but also in the diag- 1981 and 2000 at Cedars-Sinai Medical Center in Los nosis and management of MCA syndromes themselves. Angeles and Dartmouth-Hitchcock Medical Center in A renal ultrasound should be performed in patients with New Hampshire were reviewed retrospectively. Only pa- isolated preauricular pits, cup ears, or any other ear tients who underwent renal ultrasound were included in anomaly accompanied by 1 or more of the following: the chart review. -

Endoscopy-Assisted Early Correction of Single-Suture Metopic Craniosynostosis: a 19-Year Experience
CLINICAL ARTICLE J Neurosurg Pediatr 23:61–74, 2019 Endoscopy-assisted early correction of single-suture metopic craniosynostosis: a 19-year experience David F. Jimenez, MD,1 Michael J. McGinity, MD,1 and Constance M. Barone, MD2 1Department of Neurosurgery, University of Texas Health San Antonio; and 2Cosmetic Surgery Center, San Antonio, Texas OBJECTIVE The objective of this study was to present the authors’ 19-year experience treating metopic craniosynos- tosis by using an endoscopy-assisted technique and postoperative cranial orthotic therapy. The authors also aimed to provide a comprehensive, comparative statistical analysis of minimally invasive surgery (MIS) versus open surgery in reports previously published in the literature (through 2014) regarding only patients with metopic synostosis. METHODS A total of 141 patients with single-suture metopic nonsyndromic craniosynostosis sutures were treated between 1998 and 2017 by endoscopically resecting the synostosed bone followed by postoperative custom cranial orthosis use. All data used in the case series were collected prospectively and stored in a secure database. A compre- hensive literature review was performed that included all previous case series reporting common surgical performance measures. A statistical comparison of traditional open methods versus MIS techniques was performed with regard to age, length of hospital stay (LOS), surgical time, estimated blood loss (EBL), and transfusion rate. RESULTS The mean age at the time of surgery in the current series was 4.1 months. The mean EBL was 33 ml (range 5–250 ml). One patient underwent an intraoperative blood transfusion and 5 underwent postoperative blood transfu- sion for a total transfusion rate of 4.3%. -
Macrocephaly Information Sheet 6-13-19
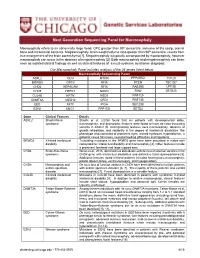
Next Generation Sequencing Panel for Macrocephaly Clinical Features: Macrocephaly refers to an abnormally large head, OFC greater than 98th percentile, inclusive of the scalp, cranial bone and intracranial contents. Megalencephaly, brain weight/volume ratio greater than 98th percentile, results from true enlargement of the brain parenchyma [1]. Megalencephaly is typically accompanied by macrocephaly, however macrocephaly can occur in the absence of megalencephaly [2]. Both macrocephaly and megalencephaly can been seen as isolated clinical findings as well as clinical features of a mutli-systemic syndromic diagnosis. Our Macrocephaly Panel includes analysis of the 36 genes listed below. Macrocephaly Sequencing Panel ASXL2 GLI3 MTOR PPP2R5D TCF20 BRWD3 GPC3 NFIA PTEN TBC1D7 CHD4 HEPACAM NFIX RAB39B UPF3B CHD8 HERC1 NONO RIN2 ZBTB20 CUL4B KPTN NSD1 RNF125 DNMT3A MED12 OFD1 RNF135 EED MITF PIGA SEC23B EZH2 MLC1 PPP1CB SETD2 Gene Clinical Features Details ASXL2 Shashi-Pena Shashi et al. (2016) found that six patients with developmental delay, syndrome macrocephaly, and dysmorphic features were found to have de novo truncating variants in ASXL2 [3]. Distinguishing features were macrocephaly, absence of growth retardation, and variability in the degree of intellectual disabilities The phenotype also consisted of prominent eyes, arched eyebrows, hypertelorism, a glabellar nevus flammeus, neonatal feeding difficulties and hypotonia. BRWD3 X-linked intellectual Truncating mutations in the BRWD3 gene have been described in males with disability nonsyndromic intellectual disability and macrocephaly [4]. Other features include a prominent forehead and large cupped ears. CHD4 Sifrim-Hitz-Weiss Weiss et al., 2016, identified five individuals with de novo missense variants in the syndrome CHD4 gene with intellectual disabilities and distinctive facial dysmorphisms [5]. -

West Texas Craniofacial Center of Excellence
TEAM MEMBERS Tammy Camp, M.D. PAID PERMIT #68 LUBBOCK, TX LUBBOCK, U.S. POSTAGE POSTAGE U.S. NONPROFIT ORG Pediatrician, Texas Tech Physicians Desiree Pendergrass, M.D. Pediatrician Dr. Camp Dr. Camp and Dr. Pendergrass will screen infants and children for cardiac, renal, feeding or airway problems often associated with syndromic craniofacial deformities. Alan Eisenbaum, M.D. Pediatric ophthalmologist, Dr. Pendergrass Texas Tech Physicians Curt Cockings, M.D. Pediatric ophthalmologist Dr. Eisenbaum and Dr. Cockings will screen infants and children with abnormal head shapes for any evidence of optic disc swelling of papilledema Dr. Eisenbaum suggestive of elevated intracranial pressure. They will also screen for any visual loss secondary to optic neuropathy, amblyopia or exposure keratopathy as a results of small orbital volume in syndromic synostoses. APPOINTMENTS Dr. Demke sees patients at the Texas Tech Physicians Medical Pavilion in the Surgery Clinic. His clinic days are Tuesday and Thursday, 8 a.m. – 5 p.m. Please call (806)743-2373 for a referral. SURGERY Dr. Nagy sees patients at Covenant Women’s and Children’s Hospital on Tuesdays and Wednesdays 9am – 5pm weekly. For this clinic location, Lubbock, 79430 Texas please call (806) 743-7700 for a referral. He also sees patients at Texas Department Surgery of Tech Physicians Medical Pavilion, 3rd floor, on Mondays from 9am – 5pm 8312 – MS Street 4th 3601 weekly. For this clinic location, please call (806) 743-7335 for a referral. If a patient needs to see both Dr. Demke and Dr. Nagy, arrangements SURGERY will be made to see the patient on the same day. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

Blueprint Genetics Craniosynostosis Panel
Craniosynostosis Panel Test code: MA2901 Is a 38 gene panel that includes assessment of non-coding variants. Is ideal for patients with craniosynostosis. About Craniosynostosis Craniosynostosis is defined as the premature fusion of one or more cranial sutures leading to secondary distortion of skull shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Premature closure of the sutures (fibrous joints) causes the pressure inside of the head to increase and the skull or facial bones to change from a normal, symmetrical appearance resulting in skull deformities with a variable presentation. Craniosynostosis may occur in an isolated setting or as part of a syndrome with a variety of inheritance patterns and reccurrence risks. Craniosynostosis occurs in 1/2,200 live births. Availability 4 weeks Gene Set Description Genes in the Craniosynostosis Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ALPL Odontohypophosphatasia, Hypophosphatasia perinatal lethal, AD/AR 78 291 infantile, juvenile and adult forms ALX3 Frontonasal dysplasia type 1 AR 8 8 ALX4 Frontonasal dysplasia type 2, Parietal foramina AD/AR 15 24 BMP4 Microphthalmia, syndromic, Orofacial cleft AD 8 39 CDC45 Meier-Gorlin syndrome 7 AR 10 19 EDNRB Hirschsprung disease, ABCD syndrome, Waardenburg syndrome AD/AR 12 66 EFNB1 Craniofrontonasal dysplasia XL 28 116 ERF Craniosynostosis 4 AD 17 16 ESCO2 SC phocomelia syndrome, Roberts syndrome -

Prenatal Ultrasonography of Craniofacial Abnormalities
Prenatal ultrasonography of craniofacial abnormalities Annisa Shui Lam Mak, Kwok Yin Leung Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Hong Kong SAR, China REVIEW ARTICLE https://doi.org/10.14366/usg.18031 pISSN: 2288-5919 • eISSN: 2288-5943 Ultrasonography 2019;38:13-24 Craniofacial abnormalities are common. It is important to examine the fetal face and skull during prenatal ultrasound examinations because abnormalities of these structures may indicate the presence of other, more subtle anomalies, syndromes, chromosomal abnormalities, or even rarer conditions, such as infections or metabolic disorders. The prenatal diagnosis of craniofacial abnormalities remains difficult, especially in the first trimester. A systematic approach to the fetal Received: May 29, 2018 skull and face can increase the detection rate. When an abnormality is found, it is important Revised: June 30, 2018 to perform a detailed scan to determine its severity and search for additional abnormalities. Accepted: July 3, 2018 Correspondence to: The use of 3-/4-dimensional ultrasound may be useful in the assessment of cleft palate and Kwok Yin Leung, MBBS, MD, FRCOG, craniosynostosis. Fetal magnetic resonance imaging can facilitate the evaluation of the palate, Cert HKCOG (MFM), Department of micrognathia, cranial sutures, brain, and other fetal structures. Invasive prenatal diagnostic Obstetrics and Gynaecology, Queen Elizabeth Hospital, Gascoigne Road, techniques are indicated to exclude chromosomal abnormalities. Molecular analysis for some Kowloon, Hong Kong SAR, China syndromes is feasible if the family history is suggestive. Tel. +852-3506 6398 Fax. +852-2384 5834 E-mail: [email protected] Keywords: Craniofacial; Prenatal; Ultrasound; Three-dimensional ultrasonography; Fetal structural abnormalities This is an Open Access article distributed under the Introduction terms of the Creative Commons Attribution Non- Commercial License (http://creativecommons.org/ licenses/by-nc/3.0/) which permits unrestricted non- Craniofacial abnormalities are common. -

Polydactyly of the Hand
A Review Paper Polydactyly of the Hand Katherine C. Faust, MD, Tara Kimbrough, BS, Jean Evans Oakes, MD, J. Ollie Edmunds, MD, and Donald C. Faust, MD cleft lip/palate, and spina bifida. Thumb duplication occurs in Abstract 0.08 to 1.4 per 1000 live births and is more common in Ameri- Polydactyly is considered either the most or second can Indians and Asians than in other races.5,10 It occurs in a most (after syndactyly) common congenital hand ab- male-to-female ratio of 2.5 to 1 and is most often unilateral.5 normality. Polydactyly is not simply a duplication; the Postaxial polydactyly is predominant in black infants; it is most anatomy is abnormal with hypoplastic structures, ab- often inherited in an autosomal dominant fashion, if isolated, 1 normally contoured joints, and anomalous tendon and or in an autosomal recessive pattern, if syndromic. A prospec- ligament insertions. There are many ways to classify tive San Diego study of 11,161 newborns found postaxial type polydactyly, and surgical options range from simple B polydactyly in 1 per 531 live births (1 per 143 black infants, excision to complicated bone, ligament, and tendon 1 per 1339 white infants); 76% of cases were bilateral, and 3 realignments. The prevalence of polydactyly makes it 86% had a positive family history. In patients of non-African descent, it is associated with anomalies in other organs. Central important for orthopedic surgeons to understand the duplication is rare and often autosomal dominant.5,10 basic tenets of the abnormality. Genetics and Development As early as 1896, the heritability of polydactyly was noted.11 As olydactyly is the presence of extra digits.