Analysis of RP2 and RPGR Mutations in Five X-Linked Chinese Families
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Retinal Dystrophy Panel Plus
ANALYSIS REPORT Patient: Test, Test 1; DoB: 1989-Apr-10; Order ID: 54324 SUMMARY DIAGNOSTIC FINDING Retinal Dystrophy Panel Plus PATIENT INFORMATION NAME DOB SSN AGE GENDER ORDER ID Test, test1 1989-Apr-10 10041989-xxxx 28 Male 54324 REFERRING HEALTHCARE PROFESSIONAL NAME HOSPITAL Anna Smith Test hospital SUMMARY OF CLINICAL HISTORY Patient is a 28-year-old male with VA 20/40 OD, 20/50 OS, constricted visual fields, non-detectable rod ffERG, and a family history consistent with X-linked retinitis pigmentosa. SEQUENCE ANALYSIS RESULTS GENE NOMENCLATURE INHERITANCE ZYGOSITY CLASSIFICATION RPGR c.2655_2656del, p.(Glu886Glyfs*192) X-linked HEM LIKELY PATHOGENIC DEL/DUP (CNV) ANALYSIS RESULTS Del/Dup (CNV) analysis did not detect any known disease-causing copy number variation or novel or rare deletion/duplication that was considered deleterious. CONCLUSION We classify the identifiedRPGR c.2655_2656del, p.(Glu886Glyfs*192) as likely pathogenic and the probable cause for the patient’s disease, considering the current evidence of the variant (established association between the gene and the patient’s phenotype, rarity in control populations, identification of the variant in an individual with the same phenotype, and mutation type: frameshift). However, additional information is still needed to confirm the pathogenicity of the variant, which could allow independent risk stratification based on this mutation. Genetic counseling and family member testing is recommended. Disease caused by RPGR mutations is inherited in an X-linked manner. We recommend carrier testing of the mother. If the mother is a carrier, then each offspring has a 50% chance of inheriting the mutation. Disease caused byRPGR mutations is inherited in an X-linked manner, and thus each daughter of an affected male will inherit the mutation, while sons will remain unaffected. -

Building the Vertebrate Codex Using the Gene Breaking Protein Trap Library
Genetics, Development and Cell Biology Publications Genetics, Development and Cell Biology 2020 Building the vertebrate codex using the gene breaking protein trap library Noriko Ichino Mayo Clinic Gaurav K. Varshney National Institutes of Health Ying Wang Iowa State University Hsin-kai Liao Iowa State University Maura McGrail Iowa State University, [email protected] See next page for additional authors Follow this and additional works at: https://lib.dr.iastate.edu/gdcb_las_pubs Part of the Molecular Genetics Commons, and the Research Methods in Life Sciences Commons The complete bibliographic information for this item can be found at https://lib.dr.iastate.edu/ gdcb_las_pubs/261. For information on how to cite this item, please visit http://lib.dr.iastate.edu/howtocite.html. This Article is brought to you for free and open access by the Genetics, Development and Cell Biology at Iowa State University Digital Repository. It has been accepted for inclusion in Genetics, Development and Cell Biology Publications by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Building the vertebrate codex using the gene breaking protein trap library Abstract One key bottleneck in understanding the human genome is the relative under-characterization of 90% of protein coding regions. We report a collection of 1200 transgenic zebrafish strains made with the gene- break transposon (GBT) protein trap to simultaneously report and reversibly knockdown the tagged genes. Protein trap-associated mRFP expression shows previously undocumented expression of 35% and 90% of cloned genes at 2 and 4 days post-fertilization, respectively. Further, investigated alleles regularly show 99% gene-specific mRNA knockdown. -

RP2 Antibody / XRP2 (RQ4671)
RP2 Antibody / XRP2 (RQ4671) Catalog No. Formulation Size RQ4671 0.5mg/ml if reconstituted with 0.2ml sterile DI water 100 ug Bulk quote request Availability 1-3 business days Species Reactivity Human, Mouse, Rat Format Antigen affinity purified Clonality Polyclonal (rabbit origin) Isotype Rabbit IgG Purity Antigen affinity purified Buffer Lyophilized from 1X PBS with 2% Trehalose and 0.025% sodium azide UniProt O75695 Applications Western blot : 0.5-1ug/ml Immunohistochemistry (FFPE) : 1-2ug/ml Immunofluorescence : 2-4ug/ml Flow cytometry : 1-3ug/million cells Direct ELISA : 0.1-0.5ug/ml (human recombinant protein) Limitations This RP2 antibody is available for research use only. Western blot testing of 1) human placenta, 2) human SGC-7901, 3) rat lung and 4) mouse lung lysate with RP2 antibody at 0.5ug/ml. Predicted molecular weight ~40 kDa. IHC staining of FFPE human placenta with RP2 antibody at 1ug/ml. HIER: boil tissue sections in pH6, 10mM citrate buffer, for 10-20 min followed by cooling at RT for 20 min. IHC staining of FFPE human placenta with RP2 antibody at 1ug/ml. HIER: boil tissue sections in pH6, 10mM citrate buffer, for 10-20 min followed by cooling at RT for 20 min. IHC staining of FFPE human lung cancer with RP2 antibody at 1ug/ml. HIER: boil tissue sections in pH6, 10mM citrate buffer, for 10-20 min followed by cooling at RT for 20 min. IHC staining of FFPE human breast cancer with RP2 antibody at 1ug/ml. HIER: boil tissue sections in pH6, 10mM citrate buffer, for 10-20 min followed by cooling at RT for 20 min. -

Pigmentosa in a Large Kindred
J Med Genet: first published as 10.1136/jmg.28.7.453 on 1 July 1991. Downloaded from I Med Genet 1991; 28: 453-457 453 Genetic localisation of the RP2 type of X linked retinitis pigmentosa in a large kindred A F Wright, SS Bhattacharya, M A Aldred, M Jay, A D Carothers, N S T Thomas, A C Bird, B Jay, H J Evans Abstract and usually loss of central vision before the fourth Genetic linkage and deletion studies have led to the decade. At least 14 to 15% of families and 15 to 28% of proposal that there are at least two loci on the X retinitis pigmentosa patients in the UK have the X chromosome which are responsible for X linked linked disorder' 2 so that the population prevalence is retinitis pigmentosa (XLRP). One locus (RP3) has in the region of 1 in 10 000 to 30 000. been closely defined by genetic linkage and deletion XLRP was first mapped to the proximal short arm analyses and localised to the region between the of the X chromosome by genetic linkage to DXS7, ornithine transcarbamylase (OTC) and chronic localised to Xpl l.-pll .3.3 Subsequent linkage granulomatous disease (CYBB) loci in Xp2l.1- studies have supported locations both proximal49 and pII.4. The other locus (RP2) has been assigned by distal'o'3 to the DXS7 locus. The situation was linkage analysis alone to region Xpll.4-pll.2, but clarified by a heterogeneity analysis of 62 XLRP its localisation is less weli defined. The results of a kindreds from nine centres, in which it was shown multipoint linkage analysis of a single large XLRP that the overall likelihood was 6-4x 109:1 in favour of kindred using eight informative loci provide further two loci versus a single XLRP locus. -
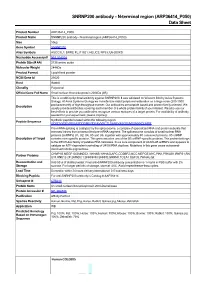
ARP36414 P050) Data Sheet
SNRNP200 antibody - N-terminal region (ARP36414_P050) Data Sheet Product Number ARP36414_P050 Product Name SNRNP200 antibody - N-terminal region (ARP36414_P050) Size 50ug Gene Symbol SNRNP200 Alias Symbols ASCC3L1; BRR2; FLJ11521; HELIC2; RP33; U5-200KD Nucleotide Accession# NM_014014 Protein Size (# AA) 2136 amino acids Molecular Weight 244kDa Product Format Lyophilized powder NCBI Gene Id 23020 Host Rabbit Clonality Polyclonal Official Gene Full Name Small nuclear ribonucleoprotein 200kDa (U5) This is a rabbit polyclonal antibody against SNRNP200. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Peptide Sequence Synthetic peptide located within the following region: GDEDVYGEVREEASDDDMEGDEAVVRCTLSANLVASGELMSSKKKDLHPR Pre-mRNA splicing is catalyzed by the spliceosome, a complex of specialized RNA and protein subunits that removes introns from a transcribed pre-mRNA segment. The spliceosome consists of small nuclear RNA proteins (snRNPs) U1, U2, U4, U5 and U6, together with approximately 80 conserved proteins. U5 snRNP Description of Target contains nine specific proteins. This gene encodes one of the U5 snRNP-specific proteins. This protein belongs to the DEXH-box family of putative RNA helicases. It is a core component of U4/U6-U5 snRNPs and appears to catalyze an ATP-dependent unwinding of U4/U6 RNA duplices. -
Supplementary File 2A Revised
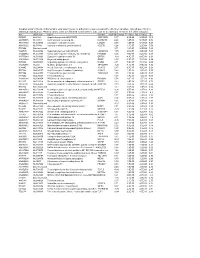
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06 -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement. -

Lineage-Specific Programming Target Genes Defines Potential for Th1 Temporal Induction Pattern of STAT4
Downloaded from http://www.jimmunol.org/ by guest on October 1, 2021 is online at: average * The Journal of Immunology published online 26 August 2009 from submission to initial decision 4 weeks from acceptance to publication J Immunol http://www.jimmunol.org/content/early/2009/08/26/jimmuno l.0901411 Temporal Induction Pattern of STAT4 Target Genes Defines Potential for Th1 Lineage-Specific Programming Seth R. Good, Vivian T. Thieu, Anubhav N. Mathur, Qing Yu, Gretta L. Stritesky, Norman Yeh, John T. O'Malley, Narayanan B. Perumal and Mark H. Kaplan Submit online. Every submission reviewed by practicing scientists ? is published twice each month by http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://www.jimmunol.org/content/suppl/2009/08/26/jimmunol.090141 1.DC1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* • Why • • Material Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2009 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of October 1, 2021. Published August 26, 2009, doi:10.4049/jimmunol.0901411 The Journal of Immunology Temporal Induction Pattern of STAT4 Target Genes Defines Potential for Th1 Lineage-Specific Programming1 Seth R. Good,2* Vivian T. Thieu,2† Anubhav N. Mathur,† Qing Yu,† Gretta L. -

RP2 Phenotype and Pathogenetic Correlations in X-Linked Retinitis Pigmentosa
OPHTHALMIC MOLECULAR GENETICS SECTION EDITOR: JANEY L. WIGGS, MD, PhD RP2 Phenotype and Pathogenetic Correlations in X-Linked Retinitis Pigmentosa Thiran Jayasundera, MD; Kari E. H. Branham, MS; Mohammad Othman, PhD; William R. Rhoades, BS; Athanasios J. Karoukis, BS; Hemant Khanna, PhD; Anand Swaroop, PhD; John R. Heckenlively, MD Objectives: To assess the phenotype of patients with function. All 3 female carriers had macular atrophy in 1 X-linked retinitis pigmentosa (XLRP) with RP2 muta- or both eyes and were myopic (mean, −6.23 D). All 9 non- tions and to correlate the findings with their genotype. sense and frameshift and 5 of 7 missense mutations (71%) resulted in severe clinical presentations. Methods: Six hundred eleven patients with RP were screened for RP2 mutations. From this screen, 18 pa- Conclusions: Screening of the RP2 gene should be pri- tients with RP2 mutations were evaluated clinically with oritized in patients younger than 16 years characterized standardized electroretinography, Goldmann visual fields, by X-linked inheritance, decreased best-corrected vi- and ocular examinations. In addition, 7 well-docu- sual acuity (eg, Ͼ20/40), high myopia, and early-onset mented cases from the literature were used to augment macular atrophy. Patients exhibiting a choroideremia- genotype-phenotype correlations. like fundus without choroideremia gene mutations should also be screened for RP2 mutations. Results: Of 11 boys younger than 12 years, 10 (91%) had macular involvement and 9 (82%) had best- Clinical Relevance: An identifiable phenotype for corrected visual acuity worse than 20/50. Two boys from RP2-XLRP aids in clinical diagnosis and targeted genetic different families (aged 8 and 12 years) displayed a cho- roideremia-like fundus, and 9 boys (82%) were myopic screening. -

Next Generation Sequencing by Multiple Samples Pooling Reveals
Next generation sequencing of pooled samples reveals new SNRNP200 mutations associated with retinitis pigmentosa Paola Benaglio1, Terri L. McGee2, Leonardo P. Capelli1,3, Shyana Harper2, Eliot L. Berson2 and Carlo Rivolta1 1Department of Medical Genetics, University of Lausanne, Lausanne, Switzerland 2The Berman-Gund Laboratory for the Study of Retinal Degenerations, Harvard Medical School, Massachusetts Eye and Ear Infirmary, Boston, Massachusetts, USA 3Department of Genetics and Evolutionary Biology, Institute of Biosciences, University of São Paulo, São Paulo, Brazil Correspondence to: Carlo Rivolta Department of Medical Genetics University of Lausanne Rue du Bugnon 27 1005 Lausanne Switzerland; Phone: +41(21) 692-5451 FAX: +41(21) 692-5455 email: [email protected] 1 ABSTRACT The gene SNRNP200 is composed of 45-exons and encodes a protein essential for pre- mRNA splicing, the 200 kDa helicase hBrr2. Despite the fact that complete lack of this protein is incompatible with cell survival, two independent heterozygous mutations in SNRNP200 have recently been found to be associated with the retinal degenerative disease retinitis pigmentosa (RP) in two families from China. In this work the entire 35-Kb SNRNP200 genomic region was analyzed in a cohort of 96 unrelated North American patients with autosomal dominant RP. To carry out this large-scale sequencing project, we performed ultra high-throughput sequencing of pooled, untagged PCR products and verified the presence of the detected DNA changes by Sanger sequencing of individual samples. One of the two previously known mutations (p.S1087L) was identified in 3 patients, and 4 new missense changes (p.R681C, p.R681H, p.V683L, p.Y689C) affecting highly conserved codons were identified in 6 unrelated individuals. -

Mechanism of Regulation of Spliceosome Activation by Brr2 And
I Mechanism of regulation of spliceosome activation by Brr2 and Prp8 and links to retinal disease Dissertation for the award of the degree “Doctor of Philosophy” (Ph.D.) in the Molecular Biology Program Division of Mathematics and Natural Sciences of the Georg-August-Universität Göttingen submitted by Sina Mozaffari-Jovin born in Sabzevar, Iran Göttingen 2012 II Members of the thesis committee: Prof. Dr. Reinhard Lührmann (Reviewer) Department of Cellular Biochemistry, Max Planck Institute for Biophysical Chemistry, Göttingen Prof. Dr. Reinhard Jahn Department of Neurobiology, Max Planck Institute for Biophysical Chemistry, Göttingen Prof. Dr. Ralf Ficner Department of Molecular Structural Biology, Institute for Microbiology and Genetics, Göttingen Date of submission of Thesis: December, 14th, 2012 III Affidavit I declare that my Ph.D. thesis entitled “Mechanism of regulation of spliceosome activation by Brr2 and Prp8 and links to retinal disease” has been written independently and with no other sources and aids than quoted. Sina Mozaffari-Jovin Göttingen, 2012 IV “The knowledge of anything, since all things have causes, is not acquired or complete unless it is known by its causes” Avicenna (Father of Modern Medicine; c. 980- June 1037) V Table of Contents 1 Abstract ......................................................................................................................... 1 2 Introduction .................................................................................................................. 4 2.1 The chemistry -

Open Data for Differential Network Analysis in Glioma
International Journal of Molecular Sciences Article Open Data for Differential Network Analysis in Glioma , Claire Jean-Quartier * y , Fleur Jeanquartier y and Andreas Holzinger Holzinger Group HCI-KDD, Institute for Medical Informatics, Statistics and Documentation, Medical University Graz, Auenbruggerplatz 2/V, 8036 Graz, Austria; [email protected] (F.J.); [email protected] (A.H.) * Correspondence: [email protected] These authors contributed equally to this work. y Received: 27 October 2019; Accepted: 3 January 2020; Published: 15 January 2020 Abstract: The complexity of cancer diseases demands bioinformatic techniques and translational research based on big data and personalized medicine. Open data enables researchers to accelerate cancer studies, save resources and foster collaboration. Several tools and programming approaches are available for analyzing data, including annotation, clustering, comparison and extrapolation, merging, enrichment, functional association and statistics. We exploit openly available data via cancer gene expression analysis, we apply refinement as well as enrichment analysis via gene ontology and conclude with graph-based visualization of involved protein interaction networks as a basis for signaling. The different databases allowed for the construction of huge networks or specified ones consisting of high-confidence interactions only. Several genes associated to glioma were isolated via a network analysis from top hub nodes as well as from an outlier analysis. The latter approach highlights a mitogen-activated protein kinase next to a member of histondeacetylases and a protein phosphatase as genes uncommonly associated with glioma. Cluster analysis from top hub nodes lists several identified glioma-associated gene products to function within protein complexes, including epidermal growth factors as well as cell cycle proteins or RAS proto-oncogenes.