Legislative Assembly of Alberta the 27Th Legislature Second Session
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Minutes of the Open Session of the University of Lethbridge Board of Governors Held Thursday, February 17, 2011 at 1:30 P.M
MINUTES OF THE OPEN SESSION OF THE UNIVERSITY OF LETHBRIDGE BOARD OF GOVERNORS HELD THURSDAY, FEBRUARY 17, 2011 AT 1:30 P.M. IN THE BOARD ROOM (W646) Present: Bob Turner (Chair), Mike Mahon, Jim Berezan, Don Chandler, Patrick Forrest, Eric Hawthorne, Gordon Jong, Taz Kassam, Heidi MacDonald, Doug McArthur, Kevin Nugent, Paul Walz, Kathleen Willms Regrets: Richard Davidson, Evelyn Good Striker, Blaine Kunz, Janice Varzari, Others: Andrew Hakin, Vice-President (Academic) & Provost Nancy Walker, Vice-President (Finance & Administration) Chris Horbachewski, Vice-President (Advancement) Karen Clearwater, Associate Vice-President (Financial Planning) Dan Weeks, Vice-President (Research) via Skype Laurel Corbiere, Senior Advisor to the President Richard Westlund (Regrets) Jill Sletto (Recording Secretary) ____________________________________________________________________________________ Bob Turner introduced Kathleen Willms to the Board of Governors and presented her with the Board of Governors briefcase and pin. Bob also introduced Jill Sletto to the Board, filling in for Jodie Black. 1. CONSENT AGENDA 1.1 Approval of the February 17, 2011 Open Session Agenda 1.2 Approval of the December 16, 2010 Open Session Minutes MOTION: opn.2011.02.01 MacDonald/Chandler That the Consent Agenda of the February 17, 2011 Open Session of the University of Lethbridge Board of Governors be approved with the addition of Item for Action 4.3 Associate VP Hr/Admin Appointment Committee. That the minutes of the Open Session of December 16, 2010 be approved with the change to Item 10 – Don Chandler’s Report, not James Berezan’s. Motion: Carried 2. BOARD CHAIR REMARKS 2.1 New Chancellor – Shirley McClellan The Chair reported that the University of Lethbridge has a new Chancellor, Dr. -

Legislative Assembly of Alberta the 27Th Legislature Fourth Session
Legislative Assembly of Alberta The 27th Legislature Fourth Session Standing Committee on the Economy Department of Advanced Education and Technology Consideration of Main Estimates Tuesday, April 12, 2011 6:30 p.m. Transcript No. 27-4-3 Legislative Assembly of Alberta The 27th Legislature Fourth Session Standing Committee on the Economy Bhardwaj, Naresh, Edmonton-Ellerslie (PC), Chair Chase, Harry B., Calgary-Varsity (AL), Deputy Chair Amery, Moe, Calgary-East (PC) Dallas, Cal, Red Deer-South (PC) Fawcett, Kyle, Calgary-North Hill (PC) Hinman, Paul, Calgary-Glenmore (W) Johnson, Jeff, Athabasca-Redwater (PC) Lund, Ty, Rocky Mountain House (PC) Taft, Dr. Kevin, Edmonton-Riverview (AL) Tarchuk, Janis, Banff-Cochrane (PC) Taylor, Dave, Calgary-Currie (AB) Woo-Paw, Teresa, Calgary-Mackay (PC) Xiao, David H., Edmonton-McClung (PC) * * substitution for Cal Dallas Department of Advanced Education and Technology Participant Hon. Greg Weadick Minister Also in Attendance Boutilier, Guy C., Fort McMurray-Wood Buffalo (W) Groeneveld, George, Highwood (PC) Notley, Rachel, Edmonton-Strathcona (ND) Support Staff W.J. David McNeil Clerk Shannon Dean Senior Parliamentary Counsel/ Director of House Services Robert H. Reynolds, QC Law Clerk/Director of Interparliamentary Relations Corinne Dacyshyn Committee Clerk Jody Rempel Committee Clerk Karen Sawchuk Committee Clerk Rhonda Sorensen Manager of Corporate Communications and Broadcast Services Melanie Friesacher Communications Consultant Tracey Sales Communications Consultant Philip Massolin Committee Research Co-ordinator Stephanie LeBlanc Legal Research Officer Diana Staley Research Officer Rachel Stein Research Officer Liz Sim Managing Editor of Alberta Hansard Transcript produced by Alberta Hansard April 12, 2011 Economy EC-447 6:30 p.m. Tuesday, April 12, 2011 cannot propose to reduce the estimate by its full amount. -

Alberta Hansard
Province of Alberta The 28th Legislature First Session Alberta Hansard Wednesday evening, November 27, 2013 Issue 75e The Honourable Gene Zwozdesky, Speaker Legislative Assembly of Alberta The 28th Legislature First Session Zwozdesky, Hon. Gene, Edmonton-Mill Creek (PC), Speaker Rogers, George, Leduc-Beaumont (PC), Deputy Speaker and Chair of Committees Jablonski, Mary Anne, Red Deer-North (PC), Deputy Chair of Committees Allen, Mike, Fort McMurray-Wood Buffalo (Ind) Kennedy-Glans, Donna, Calgary-Varsity (PC) Amery, Moe, Calgary-East (PC) Khan, Stephen, St. Albert (PC) Anderson, Rob, Airdrie (W), Klimchuk, Hon. Heather, Edmonton-Glenora (PC) Official Opposition House Leader Kubinec, Maureen, Barrhead-Morinville-Westlock (PC) Anglin, Joe, Rimbey-Rocky Mountain House-Sundre (W), Lemke, Ken, Stony Plain (PC) Official Opposition Whip Leskiw, Genia, Bonnyville-Cold Lake (PC) Barnes, Drew, Cypress-Medicine Hat (W) Luan, Jason, Calgary-Hawkwood (PC) Bhardwaj, Naresh, Edmonton-Ellerslie (PC) Lukaszuk, Hon. Thomas A., Edmonton-Castle Downs (PC) Bhullar, Hon. Manmeet Singh, Calgary-Greenway (PC) Mason, Brian, Edmonton-Highlands-Norwood (ND), Bikman, Gary, Cardston-Taber-Warner (W) Leader of the New Democrat Opposition Bilous, Deron, Edmonton-Beverly-Clareview (ND) McAllister, Bruce, Chestermere-Rocky View (W) Blakeman, Laurie, Edmonton-Centre (AL), McDonald, Everett, Grande Prairie-Smoky (PC) Liberal Opposition House Leader McIver, Hon. Ric, Calgary-Hays (PC), Brown, Dr. Neil, QC, Calgary-Mackay-Nose Hill (PC) Deputy Government House Leader Calahasen, Pearl, Lesser Slave Lake (PC) McQueen, Hon. Diana, Drayton Valley-Devon (PC) Campbell, Hon. Robin, West Yellowhead (PC), Notley, Rachel, Edmonton-Strathcona (ND), Deputy Government House Leader New Democrat Opposition House Leader Cao, Wayne C.N., Calgary-Fort (PC) Oberle, Hon. -

(April 2015) Conservative Candidate Wildrose
Election 2015 MLA Candidate Contact Info Current as of April 23, 2015 Liberal Constituency (April 2015) Conservative Candidate Wildrose Candidate NDP Candidate Candidate Lacombe-Ponoka Peter Dewit Ron Orr Doug Hart No Candidate • Central Alberta Christian High [email protected] [email protected] [email protected] School • College Heights Christian School Bay 14, Lacombe Centre Mall, Phone: (403)755-6280 (403) 963-4278 • Lacombe Christian School 5230 45 Street • Living Truth Christian School Lacombe, T4L 2A1 • Mamawi Atosketan Native School • Parkview Adventist Academy Phone: (888)343-3716 • Ponoka Christian School • Prairie Adventist Christian eSchool • Woodlands Adventist School Calgary-Currie Christine Cusaneli Terry DeVries Brian Malkinson Shelley Wark- • Banbury Crossroads School [email protected] [email protected] [email protected] Martyn • Calgary Quest Children's Society • Maria Montessori Education Suite 80, 3915 - 51 Street SW Phone (403)648-5140 Phone: (587) 434-3062 Centre Calgary, T3E 6N1 321, 3132 26 St. NE • Mountain View Academy Calgary, AB T1Y 6Z1 • New Heights School & Learning Services Edmonton-Glenora Heather Klimchuk Don Koiziak Sarah Hoffman Karen Sevcik • Coralwood Adventist Academy [email protected] [email protected] [email protected] • Edmonton Menorah Academy • Elves Special Needs Society 14215 Stony Plain Road Phone: (780)809-1328 Phone: (780) 756-7310 • MAC Islamic Academy Edmonton, T5N 3R4 10998 124 St • Progressive Academy Edmonton, AB T5M -

Legislative Assembly of Alberta the 28Th Legislature Second Session Standing Committee on Resource Stewardship
Legislative Assembly of Alberta The 28th Legislature Second Session Standing Committee on Resource Stewardship Ministry of Municipal Affairs Consideration of Main Estimates Tuesday, April 8, 2014 3:30 p.m. Transcript No. 28-2-5 Legislative Assembly of Alberta The 28th Legislature Second Session Standing Committee on Resource Stewardship Khan, Stephen, St. Albert (PC), Chair Anglin, Joe, Rimbey-Rocky Mountain House-Sundre (W), Deputy Chair Allen, Mike, Fort McMurray-Wood Buffalo (Ind) Bikman, Gary, Cardston-Taber-Warner (W) Bilous, Deron, Edmonton-Beverly-Clareview (ND) Blakeman, Laurie, Edmonton-Centre (AL) Brown, Dr. Neil, QC, Calgary-Mackay-Nose Hill (PC) Calahasen, Pearl, Lesser Slave Lake (PC) Casey, Ron, Banff-Cochrane (PC) Goudreau, Hector G., Dunvegan-Central Peace-Notley (PC) Hale, Jason W., Strathmore-Brooks (W) Johnson, Linda, Calgary-Glenmore (PC) Webber, Len, Calgary-Foothills (Ind) Xiao, David H., Edmonton-McClung (PC) Young, Steve, Edmonton-Riverview (PC) Also in Attendance Donovan, Ian, Little Bow (W) Rowe, Bruce, Olds-Didsbury-Three Hills (W) Stier, Pat, Livingstone-Macleod (W) Wilson, Jeff, Calgary-Shaw (W) Support Staff W.J. David McNeil Clerk Robert H. Reynolds, QC Law Clerk/Director of Interparliamentary Relations Shannon Dean Senior Parliamentary Counsel/ Director of House Services Philip Massolin Manager of Research Services Stephanie LeBlanc Legal Research Officer Sarah Leonard Legal Research Officer Nancy Zhang Legislative Research Officer Nancy Robert Research Officer Corinne Dacyshyn Committee Clerk Jody Rempel Committee Clerk Karen Sawchuk Committee Clerk Christopher Tyrell Committee Clerk Rhonda Sorensen Manager of Corporate Communications and Broadcast Services Jeanette Dotimas Communications Consultant Tracey Sales Communications Consultant Janet Schwegel Managing Editor of Alberta Hansard Transcript produced by Alberta Hansard Standing Committee on Resource Stewardship Participants Ministry of Municipal Affairs Hon. -
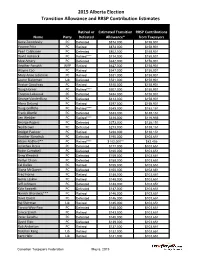
2015 Alberta Election Transition Allowance and RRSP Contribution Estimates
2015 Alberta Election Transition Allowance and RRSP Contribution Estimates Retired or Estimated Transition RRSP Contributions Name Party Defeated Allowance* from Taxpayers Gene Zwozdesky PC Defeated $874,000 $158,901 Yvonne Fritz PC Retired $873,000 $158,901 Pearl Calahasen PC Defeated $802,000 $158,901 David Hancock PC Retired**** $714,000 $158,901 Moe Amery PC Defeated $642,000 $158,901 Heather Forsyth WRP Retired $627,000 $158,901 Wayne Cao PC Retired $547,000 $158,901 Mary Anne Jablonski PC Retired $531,000 $158,901 Laurie Blakeman Lib Defeated $531,000 $158,901 Hector Goudreau PC Retired $515,000 $158,901 Doug Horner PC Retired**** $507,000 $158,901 Thomas Lukaszuk PC Defeated $484,000 $158,901 George VanderBurg PC Defeated $413,000 $158,901 Alana DeLong PC Retired $397,000 $158,901 Doug Griffiths PC Retired**** $349,000 $152,151 Frank Oberle PC Defeated $333,000 $138,151 Len Webber PC Retired**** $318,000 $116,956 George Rogers PC Defeated $273,000 $138,151 Neil Brown PC Defeated $273,000 $138,151 Bridget Pastoor PC Retired $238,000 $138,151 Heather Klimchuk PC Defeated $195,000 $103,651 Alison Redford** PC Retired**** $182,000** $82,456 Jonathan Denis PC Defeated $177,000 $103,651 Robin Campbell PC Defeated $160,000 $103,651 Greg Weadick PC Defeated $159,000 $103,651 Verlyn Olson PC Defeated $158,000 $103,651 Cal Dallas PC Retired $155,000 $103,651 Diana McQueen PC Defeated $150,000 $103,651 Fred Horne PC Retired $148,000 $103,651 Genia Leskiw PC Retired $148,000 $103,651 Jeff Johnson PC Defeated $148,000 $103,651 Kyle Fawcett -

Download Year in Review of 2012-2013
UNIVERSITY OF LETHBRIDGE STUDENTS' UNION The General Assembly Photo by deJourdan’s Photographics BACK TO FRONT (left to right, back to front) Zack Moline, Scott Anderson, Sean Glydon Abby Morning Bull, Maxine Saretsky, Liisa Kleemola, Brady Schnell, Katie Kalmar, Michael Kawchuk, Rafaela Da Cruz, Julia Adolf, Armin Escher, Shuna Talbot, Felipe Ferreira, Shashi Kant Ghai. MISSING James Forbes, Brandon McNally, Chris Hollingsworth, Victoria Wells, Jesse Mullett, Bonnie Farries (Chair). A YEAR IN REVIEW OF 2012-2013 Table of Contents Welcome General Assembly Reports Introduction . 2 Non Faculty Year End Reports . 28 How we Began the Year . 2 Edmonton Campus Photos . 31 Our General Assembly Chair. 3 Students’ Union Awards Student Council & Staff Award Winners . 32 General Assembly of 2012-2013 . 5 Commissioners . 5 Financial Matters New & Permanent Staff . 5 Sponsorship & Funding . 36 Scholarships, Bursaries & Awards . 38 Advocacy & Representation Notable ULSU Committee Activity . 6 Operations University Affairs . 7 Health & Dental, Bookings, Food Court . 39 Travel: Conferences, Seminars, Meetings . .10 ULSU Food Bank . 40 Meetings with Politicians . 13 Election & Referendums Clubs, Fraternities, Sororities Election & Referendum . 42 Report & Award Winners . 14 Club Benefits . 15 Incoming & Previous Council Ratified Groups for 2012-2013 . 16 Incoming Council . 43 Club Photos . .17 Previous Council . .44 Notable Initiatives Vision & Mission Statement New & Re-occurring Initiatives . 18 Vision . 45 Mission . 45 Events & Activities Notable ULSU Academic Events . 20 In the Lethbridge Community . 21 Fresh Fest . 22 Event List of 2012-2013 . 24 Frostbite . 25 Campus Community Events . 26 The Media . 27 Editor and Designer: Susan Curtis - executive assistant. Contributing writers: general assembly representatives, students’ union staff members. Portrait photos (page 4 & 44): by deJourdan's Photographics Ltd. -

Legislative Assembly of Alberta the 27Th Legislature First Session
Legislative Assembly of Alberta The 27th Legislature First Session Standing Committee on the Economy Wednesday, September 10, 2008 10:31 a.m. Transcript No. 27-1-3 Legislative Assembly of Alberta The 27th Legislature First Session Standing Committee on the Economy Allred, Ken, St. Albert (PC), Chair Taylor, Dave, Calgary-Currie (L), Deputy Chair Amery, Moe, Calgary-East (PC) Bhullar, Manmeet Singh, Calgary-Montrose (PC) Blakeman, Laurie, Edmonton-Centre (L) Campbell, Robin, West Yellowhead (PC) Johnson, Jeff, Athabasca-Redwater (PC) * Marz, Richard, Olds-Didsbury-Three Hills (PC) Mason, Brian, Edmonton-Highlands-Norwood (NDP) McFarland, Barry, Little Bow (PC) Weadick, Greg, Lethbridge-West (PC) Xiao, David H., Edmonton-McClung (PC) * substitution for Robin Campbell Bill 204 Sponsor Johnston, Art, Calgary-Hays (PC) Department of Transportation Participants Marlene Anderson Manager, Policy and Research Jeanette Espie Executive Director, Office of Traffic Safety Shaun Hammond Assistant Deputy Minister, Transportation Safety and Services Division Support Staff W.J. David McNeil Clerk Louise J. Kamuchik Clerk Assistant/Director of House Services Micheline S. Gravel Clerk of Journals/Table Research Robert H. Reynolds, QC Senior Parliamentary Counsel Shannon Dean Senior Parliamentary Counsel Corinne Dacyshyn Committee Clerk Erin Norton Committee Clerk Jody Rempel Committee Clerk Karen Sawchuk Committee Clerk Rhonda Sorensen Manager of Communications Services Melanie Friesacher Communications Consultant Tracey Sales Communications Consultant Philip Massolin Committee Research Co-ordinator Stephanie LeBlanc Legal Research Officer Diana Staley Research Officer Rachel Stein Research Officer Liz Sim Managing Editor of Alberta Hansard Transcript produced by Alberta Hansard September 10, 2008 Economy EC-25 10:31 a.m. Wednesday, September 10, 2008 agenda has been posted on the web. -

Premier Promotes Verlyn Olson and Greg Weadick to Cabinet Cal Dallas Becomes the New Parliamentary Assistant to Finance
February 17, 2011 Premier promotes Verlyn Olson and Greg Weadick to cabinet Cal Dallas becomes the new Parliamentary Assistant to Finance Edmonton... Premier Ed Stelmach announced today that Wetaskiwin-Camrose MLA Verlyn Olson, QC, has been named Minister of Justice and Attorney General, and Lethbridge West MLA Greg Weadick has been named Minister of Advanced Education and Technology. “I’m pleased to welcome Verlyn and Greg to the cabinet table,” said Premier Stelmach. “Verlyn and Greg bring the necessary talent and experience - Greg as a parliamentary assistant and Verlyn as a long-time member of the bar - to complete our cabinet team. Our cabinet will continue to provide the steady leadership required right now to continue building a better Alberta.” Premier Stelmach also named a new Parliamentary Assistant to the Minister of Finance and Enterprise. “I’m pleased that Red Deer South MLA Cal Dallas, who had been serving as the Parliamentary Assistant in Environment, will take over this important role and work closely with Finance Minister Lloyd Snelgrove,” said the Premier. Premier Stelmach also announced changes to committee memberships. Joining the Agenda and Priorities Committee are Sustainable Resource Development Minister Mel Knight, Children and Youth Services Minister Yvonne Fritz and Agriculture and Rural Development Minister Jack Hayden. New members of Treasury Board are Len Webber, Minister of Aboriginal Relations, Heather Klimchuk, Minister of Service Alberta, and Naresh Bhardwaj, MLA for Edmonton-Ellerslie. The new Cabinet members will be sworn in Friday, February 18 at 8:30 a.m. at Government House. Lloyd Snelgrove was sworn in as Minister of Finance and Enterprise on January 31. -

The Friendly Centre” 1904—13Th Ave
NORD - BRIDGE SENIORS Newsletter March 2014 “The Friendly Centre” 1904—13th Ave. North Lethbridge, Alberta T1H 4W9 Open Monday to Friday - 8:30 a.m. to 4:30 p.m. Telephone 403-329-3222 Fax 403-329-8824 E-mail: [email protected] 2013-2014 Computer Training Lethbridge Community Network NORD-BRIDGE SENIORS Library Marie Areshenko, Janet Bobinec EXECUTIVE Mind Joggers Judy Knox, Jack Simmons President Jim Hahn Ted Sillito, Melvin Horn Vice-President Pat Santa FUNDRAISING Pat Santa *, Board Rep Treasurer Roberta Svennes Secretary Marilynn Heaton GAMING Harry Fischer *, Board Rep Past-President Harry Fischer Casino Coordinator Mike Bennett In-House Bingo Coordinators Shirley Cavanaugh & Frances BOARD OF DIRECTORS Wallace FIRST YEAR SECOND YEAR THIRD YEAR Monday Jam Draws Helen Gepneris, Blaine Hyggen Delores Bourk Kaz Tomomitsu Eva Deringer Winners Bingo Rep/Co-ord Bonnie Hammond Clay Olsen Rodney Foster Walter “Red” Nowell Winners Bingo Alternate Leonard Hutchinson Donna Takeda Elaine Molyneux Paul White HEALTH & FITNESS Paul White *, Board Rep ADMINISTRATIVE STAFF Keep Fit Classes Erin Ko & Melanie Hillaby Executive Director Randy Smith Tai Chi Lynn Hunter-Johnston Sr. Administrative Ass’t Kathleen Filkowski (Wed, Thur, Fri) Yoga/Pilates Melanie Hillaby Administrative Assistant Shirley Trefan (Mon, Tues, Wed) Fitball/Exercise With Arthritis T. J. Dunn Financial Officer Roberta Svennes Zumba Jeannie Williamson Bookkeeper Tracy Beauchemin Fitness 55 Club Jim Scott (Volunteer Trainer) Director of Programming David Ng Reception Supervisor -

Legislative Assembly of Alberta the 27Th Legislature First Session Standing Committee on the Economy
Legislative Assembly of Alberta The 27th Legislature First Session Standing Committee on the Economy Monday, September 29, 2008 10 a.m. Transcript No. 27-1-4 Legislative Assembly of Alberta The 27th Legislature First Session Standing Committee on the Economy Allred, Ken, St. Albert (PC), Chair Taylor, Dave, Calgary-Currie (L), Deputy Chair Amery, Moe, Calgary-East (PC) Bhullar, Manmeet Singh, Calgary-Montrose (PC) Blakeman, Laurie, Edmonton-Centre (L) Campbell, Robin, West Yellowhead (PC) Marz, Richard, Olds-Didsbury-Three Hills (PC) Mason, Brian, Edmonton-Highlands-Norwood (NDP) McFarland, Barry, Little Bow (PC) Weadick, Greg, Lethbridge-West (PC) Xiao, David H., Edmonton-McClung (PC) Bill 204 Sponsor Johnston, Art, Calgary-Hays (PC) Department of Solicitor General and Public Security Participant Al Sauve Executive Director, Sheriffs Branch Police Services Participants George Harper Staff Sergeant, Traffic Commander, Provincial Capital District, Royal Canadian Mounted Police Barry Maron Acting Staff Sergeant, Traffic Section, Edmonton Police Service Michael O’Connor Constable, Traffic Education, Calgary Police Service Ben Wilkowski Sergeant, Traffic Commander, Strathcona County Traffic Services, Royal Canadian Mounted Police Support Staff W.J. David McNeil Clerk Louise J. Kamuchik Clerk Assistant/Director of House Services Micheline S. Gravel Clerk of Journals/Table Research Robert H. Reynolds, QC Senior Parliamentary Counsel Shannon Dean Senior Parliamentary Counsel Corinne Dacyshyn Committee Clerk Erin Norton Committee Clerk Jody Rempel Committee Clerk Karen Sawchuk Committee Clerk Rhonda Sorensen Manager of Communications Services Melanie Friesacher Communications Consultant Tracey Sales Communications Consultant Philip Massolin Committee Research Co-ordinator Stephanie LeBlanc Legal Research Officer Diana Staley Research Officer Rachel Stein Research Officer Liz Sim Managing Editor of Alberta Hansard Transcript produced by Alberta Hansard September 29, 2008 Economy EC-41 10 a.m. -

Industry, Labour and Government Gather to Chart Alberta's Future Workforce Minister's Forum Supports Alberta's Competitiveness Strategy
October 27, 2010 Industry, labour and government gather to chart Alberta's future workforce Minister's forum supports Alberta's Competitiveness Strategy Edmonton... With Alberta’s competitiveness as a focus, more than 130 officials representing employers, industry associations, labour and professional organizations, educators and government are gathering October 27 in Edmonton to plan Alberta’s future workforce. “Alberta needs to be ready for the next stage of growth. Our province has an amazing future and we need to ensure we have a skilled, productive, innovative and creative workforce to compete globally,” said Employment and Immigration Minister Thomas Lukaszuk. “With the global financial crisis and recession essentially behind us, it’s now time to develop policies that will meet the needs of the next generation economy of Canada and Alberta,” said keynote speaker Glen Hodgson, senior vice-president and chief economist of the Conference Board of Canada. “Many of these policy issues are connected to the labour force such as the aging workforce, immigration and productivity.” Participants will review recent progress made in strengthening the workforce through various specific strategies, including review of two newly released reports: Alberta Industry Workforce Strategies Progress Update 2006-2010, an industry document highlighting some of the actions of eight different industry workforce strategies Building and Educating Tomorrow’s Workforce Performance Update 2009, an Alberta government report detailing progress on the implementation of 17 cross-government actions. The full reports are available at www.employment.alberta.ca/betw. During the forum, participants will take part in panel and group discussions which will identify ways to meet future workforce needs, taking other government initiatives into account such as the Alberta Competitiveness Council.