Envisioning the Future: the 2008 Presidential Candidates' Health Reform Proposals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Quotes from Co-Signers of Garrett's Iran Letter to President
QUOTES FROM CO-SIGNERS OF GARRETT’S IRAN LETTER TO PRESIDENT BUSH Walter Jones ● Authored A Letter With Democrat Rep. Keith Ellison Encouraging Negotiations With Iran In 2012, Jones Signed A Letter With Democrat Rep. Keith Ellison (D-MN) Encouraging Negotiations With Iran. “We strongly encourage your Administration to pursue bilateral and multilateral engagement with Iran. While we acknowledge that progress will be difficult, we believe that robust, sustained diplomacy is the best option to resolve our serious concerns about Iran's nuclear program, and to prevent a costly war that would be devastating for the United States and our allies in the region.” (Walter B. Jones and Keith Ellison, Letter, 3/2/12) ● Extreme Minority Of House Members To Vote Against Additional Sanctions On Iran In 2012, The House Passed Additional Sanctions Against Iran's Energy, Shipping, and Insurance Sectors. “Both houses of Congress approved legislation on Wednesday that would significantly tighten sanctions against Iran's energy, shipping and insurance sectors. The bill is the latest attempt by Congress to starve Iran of the hard currency it needs to fund what most members agree is Iran's ongoing attempt to develop a nuclear weapons program.” (Pete Kasperowicz, “House, Senate Approve Tougher Sanctions Against Iran, Syria,” The Hill's Floor Action, 8/1/12) One Of Only Six House Members To Vote Against The 2012 Sanctions Bill. “The sanctions bill was approved in the form of a resolution making changes to prior legislation, H.R. 1905, on which the House and Senate agreed — it passed in an 421-6 vote, and was opposed by just five Republicans and one Democrat. -
Picking the Vice President
Picking the Vice President Elaine C. Kamarck Brookings Institution Press Washington, D.C. Contents Introduction 4 1 The Balancing Model 6 The Vice Presidency as an “Arranged Marriage” 2 Breaking the Mold 14 From Arranged Marriages to Love Matches 3 The Partnership Model in Action 20 Al Gore Dick Cheney Joe Biden 4 Conclusion 33 Copyright 36 Introduction Throughout history, the vice president has been a pretty forlorn character, not unlike the fictional vice president Julia Louis-Dreyfus plays in the HBO seriesVEEP . In the first episode, Vice President Selina Meyer keeps asking her secretary whether the president has called. He hasn’t. She then walks into a U.S. senator’s office and asks of her old colleague, “What have I been missing here?” Without looking up from her computer, the senator responds, “Power.” Until recently, vice presidents were not very interesting nor was the relationship between presidents and their vice presidents very consequential—and for good reason. Historically, vice presidents have been understudies, have often been disliked or even despised by the president they served, and have been used by political parties, derided by journalists, and ridiculed by the public. The job of vice president has been so peripheral that VPs themselves have even made fun of the office. That’s because from the beginning of the nineteenth century until the last decade of the twentieth century, most vice presidents were chosen to “balance” the ticket. The balance in question could be geographic—a northern presidential candidate like John F. Kennedy of Massachusetts picked a southerner like Lyndon B. -

Giuliani, 9/11 and the 2008 Race
ABC NEWS/WASHINGTON POST POLL: ‘08 ELECTION UPDATE EMBARGOED FOR RELEASE AFTER 11:35 p.m. Tuesday, Sept. 11, 2007 Giuliani, 9/11 and the 2008 Race Six years after the terrorist attacks that vaulted him to national prominence, it’s unclear whether 9/11 will lift Rudy Giuliani all the way to the presidency: He remains hamstrung in the Republican base, and his overall support for his party’s nomination has slipped in the latest ABC News/Washington Post poll. Giuliani does better with Republicans who are concerned about another major terrorist attack in this country, a legacy of his 9/11 performance. But among those less focused on terrorism, he’s in a dead heat against newcomer Fred Thompson. Thompson also challenges Giuliani among conservatives and evangelical white Protestants – base groups in the Republican constituency – while John McCain has stabilized after a decline in support. Giuliani still leads, but his support is down by nine points in this poll from his level in July. Indeed this is the first ABC/Post poll this cycle in which Giuliani had less than a double- digit lead over all his competitors: He now leads Thompson by nine points (and McCain by 10). Among Republicans and Republican-leaning independents, 28 percent support Giuliani, 19 percent Thompson, 18 percent McCain and 10 percent Mitt Romney. Other candidates remain in the low single digits. (There’s no significant difference among registered voters – and plenty of time to register.) ’08 Republican primary preferences Now July June April Feb Giuliani 28% 37 34 35 53 Thompson 19 15 13 10 NA McCain 18 16 20 22 23 Romney 10 8 10 10 5 The Democratic race, meanwhile, remains exceedingly stable; Hillary Clinton has led Barack Obama by 14 to 16 points in each ABC/Post poll since February, and still does. -

A History of Maryland's Electoral College Meetings 1789-2016
A History of Maryland’s Electoral College Meetings 1789-2016 A History of Maryland’s Electoral College Meetings 1789-2016 Published by: Maryland State Board of Elections Linda H. Lamone, Administrator Project Coordinator: Jared DeMarinis, Director Division of Candidacy and Campaign Finance Published: October 2016 Table of Contents Preface 5 The Electoral College – Introduction 7 Meeting of February 4, 1789 19 Meeting of December 5, 1792 22 Meeting of December 7, 1796 24 Meeting of December 3, 1800 27 Meeting of December 5, 1804 30 Meeting of December 7, 1808 31 Meeting of December 2, 1812 33 Meeting of December 4, 1816 35 Meeting of December 6, 1820 36 Meeting of December 1, 1824 39 Meeting of December 3, 1828 41 Meeting of December 5, 1832 43 Meeting of December 7, 1836 46 Meeting of December 2, 1840 49 Meeting of December 4, 1844 52 Meeting of December 6, 1848 53 Meeting of December 1, 1852 55 Meeting of December 3, 1856 57 Meeting of December 5, 1860 60 Meeting of December 7, 1864 62 Meeting of December 2, 1868 65 Meeting of December 4, 1872 66 Meeting of December 6, 1876 68 Meeting of December 1, 1880 70 Meeting of December 3, 1884 71 Page | 2 Meeting of January 14, 1889 74 Meeting of January 9, 1893 75 Meeting of January 11, 1897 77 Meeting of January 14, 1901 79 Meeting of January 9, 1905 80 Meeting of January 11, 1909 83 Meeting of January 13, 1913 85 Meeting of January 8, 1917 87 Meeting of January 10, 1921 88 Meeting of January 12, 1925 90 Meeting of January 2, 1929 91 Meeting of January 4, 1933 93 Meeting of December 14, 1936 -

NTS Total Election Reporting and Certification System - Condensed Recanvass Report
FRX2Any v.08.00.00 DEMO NTS Total Election Reporting and Certification System - Condensed Recanvass Report GREENE COUNTY BOARD OF ELECTIONS Primary Election 02/05/2008 OFFICIAL DEMOCRATIC PARTY County Wide - PRESIDENT OF THE UNITED STATES (DEMOCRATIC) Ashland - Page 1 Whole Number DEM DEM DEM DEM DEM DEM Blank Votes HILLARY BILL JOE BIDEN JOHN EDWARDS BARACK OBAMA DENNIS J CLINTON RICHARDSON KUCINICH 28 15 1 0 1 11 0 0 WARD TOTALS 28 15 1 0 1 11 0 0 Athens - Page 1 Whole Number DEM DEM DEM DEM DEM DEM Blank Votes HILLARY BILL JOE BIDEN JOHN EDWARDS BARACK OBAMA DENNIS J CLINTON RICHARDSON KUCINICH 184 109 0 0 3 70 1 1 W:000 D:002 63 39 0 0 2 22 0 0 WARD TOTALS 247 148 0 0 5 92 1 1 Cairo - Page 1 Whole Number DEM DEM DEM DEM DEM DEM Blank Votes HILLARY BILL JOE BIDEN JOHN EDWARDS BARACK OBAMA DENNIS J CLINTON RICHARDSON KUCINICH 97 66 2 0 2 26 0 1 W:000 D:004 184 115 3 0 5 59 2 0 WARD TOTALS 281 181 5 0 7 85 2 1 Catskill - Page 1 Whole Number DEM DEM DEM DEM DEM DEM Blank Votes HILLARY BILL JOE BIDEN JOHN EDWARDS BARACK OBAMA DENNIS J CLINTON RICHARDSON KUCINICH 142 70 1 0 1 70 0 0 W:000 D:005 154 80 0 1 2 61 2 8 W:000 D:008 10 4 0 0 0 6 0 0 02/26/2008 08:52:55 AM Page 1 FRX2Any v.08.00.00 DEMO NTS Total Election Reporting and Certification System - Condensed Recanvass Report GREENE COUNTY BOARD OF ELECTIONS Primary Election 02/05/2008 OFFICIAL DEMOCRATIC PARTY County Wide - PRESIDENT OF THE UNITED STATES (DEMOCRATIC) Catskill - Page 1 Whole Number DEM DEM DEM DEM DEM DEM Blank Votes HILLARY BILL JOE BIDEN JOHN EDWARDS BARACK OBAMA DENNIS -

Storm May Bring Snow to Valley Floor
Mendo women Rotarians plan ON THE MARKET fall to Solano Super Bowl bash Guide to local real estate .............Page A-6 ............Page A-3 ......................................Inside INSIDE Mendocino County’s Obituaries The Ukiah local newspaper ..........Page 2 Tomorrow: Rain High 45º Low 41º 7 58551 69301 0 FRIDAY Jan. 25, 2008 50 cents tax included DAILY JOURNAL ukiahdailyjournal.com 38 pages, Volume 149 Number 251 email: [email protected] Storm may bring snow to valley floor By ZACK SAMPSEL but with low pressure systems from and BEN BROWN Local agriculture not expected to sustain damage the Gulf of Alaska moving in one The Daily Journal after another the cycle remains the A second round of winter storms the valley floor, but the weather is not the county will experience scattered ing routine for some Mendocino same each day. lining up to hit Mendocino County expected to be a threat to agriculture. showers today with more mountain County residents. The previous low pressure system today is expected to bring more rain, According to reports from the snow to the north in higher eleva- Slight afternoon warmups have cold temperatures and snow as low as National Weather Service, most of tions, which has been the early-morn- helped to make midday travel easier, See STORM, Page A-12 GRACE HUDSON MUSEUM READIES NEW EXHIBIT Kucinich’s wife cancels planned stop in Hopland By ROB BURGESS The Daily Journal Hey, guess what? Kucinich quits Elizabeth Kucinich is coming to Mendocino campaign for County. Wait. Hold on. No, White House actually she isn’t. Associated In what should be a Press familiar tale to perennial- Democrat ly disappointed support- Dennis Kuci- ers of Democratic presi- nich is aban- dential aspirant Rep. -

Union Calendar No. 603
Union Calendar No. 603 110TH CONGRESS " ! REPORT 2d Session HOUSE OF REPRESENTATIVES 110–930 ACTIVITIES OF THE COMMITTEE ON OVERSIGHT AND GOVERNMENT REFORM ONE HUNDRED TENTH CONGRESS FIRST AND SECOND SESSIONS 2007–2008 Available via the World Wide Web: http://www.gpoaccess.gov/congress/ index.html http://www.house.gov/reform JANUARY 2, 2009.—Committed to the Committee of the Whole House on the State of the Union and ordered to be printed VerDate Aug 31 2005 01:57 Jan 03, 2009 Jkt 046108 PO 00000 Frm 00001 Fmt 6012 Sfmt 6012 E:\HR\OC\HR930.XXX HR930 smartinez on PROD1PC64 with REPORTS congress.#13 ACTIVITIES REPORT OF THE HOUSE COMMITTEE ON OVERSIGHT AND GOVERNMENT REFORM VerDate Aug 31 2005 01:57 Jan 03, 2009 Jkt 046108 PO 00000 Frm 00002 Fmt 6019 Sfmt 6019 E:\HR\OC\HR930.XXX HR930 smartinez on PROD1PC64 with REPORTS with PROD1PC64 on smartinez 1 Union Calendar No. 603 110TH CONGRESS " ! REPORT 2d Session HOUSE OF REPRESENTATIVES 110–930 ACTIVITIES OF THE COMMITTEE ON OVERSIGHT AND GOVERNMENT REFORM ONE HUNDRED TENTH CONGRESS FIRST AND SECOND SESSIONS 2007–2008 Available via the World Wide Web: http://www.gpoaccess.gov/congress/ index.html http://www.house.gov/reform JANUARY 2, 2009.—Committed to the Committee of the Whole House on the State of the Union and ordered to be printed U.S. GOVERNMENT PRINTING OFFICE 46–108 WASHINGTON : 2009 VerDate Aug 31 2005 01:57 Jan 03, 2009 Jkt 046108 PO 00000 Frm 00003 Fmt 4012 Sfmt 4012 E:\HR\OC\HR930.XXX HR930 smartinez on PROD1PC64 with REPORTS congress.#13 COMMITTEE ON OVERSIGHT AND GOVERNMENT REFORM HENRY A. -
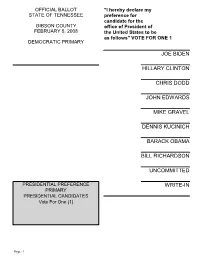
Joe Biden Hillary Clinton Chris Dodd John Edwards Mike Gravel Dennis Kucinich Barack Obama Bill Richardson Uncommitted Write-In
OFFICIAL BALLOT "I hereby declare my STATE OF TENNESSEE preference for candidate for the GIBSON COUNTY office of President of FEBRUARY 5, 2008 the United States to be as follows" VOTE FOR ONE 1 DEMOCRATIC PRIMARY JOE BIDEN HILLARY CLINTON CHRIS DODD JOHN EDWARDS MIKE GRAVEL DENNIS KUCINICH BARACK OBAMA BILL RICHARDSON UNCOMMITTED PRESIDENTIAL PREFERENCE WRITE-IN PRIMARY PRESIDENTIAL CANDIDATES Vote For One (1) Page: 1 PROPERTY ASSESSOR Vote For One (1) MARK CARLTON JOSEPH F. HAMMONDS JOHN MCCURDY GARY F. PASCHALL WRITE-IN Page: 2 OFFICIAL BALLOT "I hereby declare my STATE OF TENNESSEE preference for candidate for the GIBSON COUNTY office of President of FEBRUARY 5, 2008 the United States to be as follows" VOTE FOR ONE 1 REPUBLICAN PRIMARY RUDY GIULIANI MIKE HUCKABEE DUNCAN HUNTER ALAN KEYES JOHN MCCAIN RON PAUL MITT ROMNEY TOM TANCREDO FRED THOMPSON PRESIDENTIAL PREFERENCE UNCOMMITTED PRIMARY PRESIDENTIAL CANDIDATES Vote For One (1) WRITE-IN Page: 3 THE FOLLOWING OFFICE Edna Elaine Saltsman CONTINUES ON PAGES 2-5 John Bruce Saltsman, Sr. DELEGATES AT LARGE John "Chip" Saltsman, Jr. Committed and Uncommitted Vote For Twelve (12) Kari H. Smith MIKE HUCKABEE Michael L. Smith Emily G. Beaty Windy J. Smith Robert Arthur Bennett JOHN MCCAIN H.E. Bittle III Todd Gardenhire Beth G. Cox Justin D. Pitt Kenny D. Crenshaw Melissa B. Crenshaw Dan L. Hardin Cynthia H. Murphy Deana Persson Eric Ratcliff CONTINUED ON NEXT PAGE Page: 4 DELEGATES AT LARGE Matthew Rideout Committed and Uncommitted Vote For Twelve (12) Mahmood (Michael) Sabri RON PAUL Cheryl Scott William M. Coats Joanna C. -

John D. Edwards
John D. Edwards Clive City Council Member John Edwards was first elected in 1995 and has been re-elected for six additional consecutive terms. From 1998 to 2005 and since 2009 he has filled the role of mayor pro- tempore. He has chaired the Personnel Committee since 2018 and its predecessor committees for years prior to that. Before being elected to the City Council he served on the Clive Library Committee and the Clive Active Park Task Force. He twice was elected Chair of the Board of Trustees of the Des Moines Metropolitan Transit Authority, serving in 1997-98 and 2003-04, with tenure on the MTA Board for more than a decade. From 2007 to 2018 he served on the Des Moines Area Metropolitan Planning Organization (MPO) and is on the MPO Surface Transportation Program (STP) Funding Subcommittee. He has been a representative to the Metro Advisory Council (MAC) since 2005, was elected chair in 2018, and has been re-elected three times since then. John is Professor of Law, Associate Dean for Information Resources and Technology, and Director of the Law Library at Drake University Law School. He has lived in Clive since 1984, when his position at Drake brought him here. John and his wife Beth Ann have three adult children and four grandchildren. His community activities include: Des Moines Presbytery Pulpit Supply, since 2012. St. John's Lutheran Church, Audio Visual Technician, since 2015. Boy Scouts Troop 208, Committee Chair, 1994-98. Iowa Supreme Court Commission on Planning for the 21st Century, 1995-96. State Law Library Advisory Committee, 1991-92. -

January 15 2008 Tally Sheets
CITY OF KALAMAZOO PRESIDENTIAL PRIMARY ELECTION January 15, 2008 SUMMARY OF VOTES PRECINCT 123456 7 8910 REGISTERED VOTERS 1,788 1,557 1,987 1,794 1,975 2,015 2,362 3,186 2,441 2,418 PRECINCT VOTERS 156 105 125 98 151 342 208 145 100 265 REPBULICAN VOTERS 62 41 50 58 67 200 75 37 6 136 DEMOCRATIC VOTERS 94 64 75 40 84 142 133 108 94 128 AV VOTERS 34 20 17 25 41 88 38 40 23 154 PRECINCT TURNOUT 8.7% 6.7% 6.3% 5.5% 7.6% 17.0% 8.8% 4.6% 4.1% 11.0% TOTAL TURNOUT 10.6% 8.0% 7.1% 6.9% 9.7% 21.3% 10.4% 5.8% 5.0% 17.3% PRECINCT 11 12 13 14 15 16 17 18 19 20 REGISTERED VOTERS 1,799 1,929 2,724 2,367 2,018 1,859 2,109 2,219 2,121 PRECINCT VOTERS 121 342 204 0 207 262 236 273 215 488 REPBULICAN VOTERS 33 173 93 89 134 130 158 120 263 DEMOCRATIC VOTERS 88 169 111 118 128 106 115 95 225 AV VOTERS 22 82 33 47 97 55 69 51 107 PRECINCT TURNOUT 6.7% 17.7% 7.5% ##### 8.7% 13.0% 12.7% 12.9% 9.7% 23.0% TOTAL TURNOUT 7.9% 22.0% 8.7% ##### 10.7% 17.8% 15.7% 16.2% 12.0% 28.1% PRECINCT 21 22 23 24 25 26 TOTAL REGISTERED VOTERS 1,283 2,100 2,195 1,190 1,384 1,788 50,608 PRECINCT VOTERS 317 337 218 172 320 339 5,746 REPBULICAN VOTERS 144 209 106 64 187 184 2,819 663 AV VOTERS DEMOCRATIC VOTERS 173 128 112 108 133 155 2,926 828 AV VOTERS AV VOTERS 104 91 94 51 118 152 1,653 7,399 TOTAL VOTER PRECINCT TURNOUT 24.7% 16.0% 9.9% 14.5% 23.1% 19.0% 11.35% TOTAL TURNOUT 32.8% 20.4% 14.2% 18.7% 31.6% 27.5% 14.6% CITY OF KALAMAZOO PRESIDENTIAL PRIMARY ELECTION January 15, 2008 SUMMARY OF VOTES (PCTS 1-26) PRECINCT 1 23456 7 8 9 10 REPUBLICAN - PRESIDENT OF THE UNITED STATES -

The Sunday Fix for Even More of the Fix Go to Washingtonpost.Com/Thefix
2BLACK A2 DAILY 01-20-08 MD RE A2 BLACK A2 Sunday, January 20, 2008 R The Washington Post ON WASHINGTONPOST.COM The Sunday Fix For even more of the Fix go to washingtonpost.com/thefix CHRIS CILLIZZA AND SHAILAGH MURRAY It’s Never Too Early to Think About No. 2 Here at the Sunday Fix, we’re already looking beyond the nomination fi ghts to the always entertaining vice presidential speculation game. We queried some party strategists for their thoughts on the early front-runners. Here’s their consensus: DEMOCRATS John Edwards Tim Kaine Wesley Clark Tom Daschle Evan Bayh Kathleen Sebelius Tom Vilsack The former senator from The popular Virginia Clark, who ran for presi- He and his political in- The senator from Indiana The two-term Kansas Going into the Iowa cau- North Carolina has done governor was one of the dent in 2004, has been ner circle are extremely is clearly angling for the governor is a rising star cuses, Vilsack was the it once, so most peo- first to endorse Sen. one of the most valu- close to Obama. Daschle No. 2 slot, with his early nationally and is coming leader in the clubhouse ple think he won’t do it Barack Obama (Ill.). able surrogates of Sen. would help Obama ad- endorsement and strong off a successful stint as for vice president if Clin- again. If Edwards stays Kaine comes from a Hillary Rodham Clinton dress questions about advocacy for Clinton. He chairman of the Demo- ton were to win the nom- in through the conven- swing state, is term- (N.Y.). -
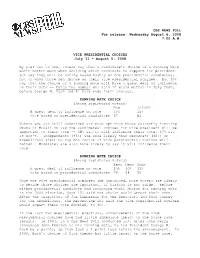
The Choice of Running Mate
CBS NEWS POLL For release: Wednesday August 6, 2008 7:00 A.M. VICE PRESIDENTIAL CHOICES July 31 - August 5, 2008 By over two to one, voters say that a candidate’s choice of a running mate won’t matter much when deciding which candidate to support for president. 67% say they will be voting based mostly on the presidential candidates, not on whom those men choose as their vice presidential nominee. But 30% say that the choice of a running mate will have a great deal of influence on their vote -- twice the number who said it would matter in July 2000, before George W. Bush and Al Gore made their choices. RUNNING MATE CHOICE (Among registered voters) Now 7/2000 A great deal of influence on vote 30% 15% Vote based on presidential candidates 67 81 Voters who are still undecided are more apt than those currently favoring Obama or McCain to say the candidates’ choices for vice president will be important to their vote -- 48% say it will influence their vote, 47% say it won’t. Independents (35%) are more likely than Democrats (30%) or Republicans (24%) to say the choice of vice presidential nominee will matter. Moderates are also more likely to say it will influence their vote. RUNNING MATE CHOICE (Among registered voters) Reps Dems Inds A great deal of influence on vote 24% 30% 35% Vote based on presidential candidates 74 68 60 Once the vice presidential nominees are announced, more voters are likely to decide those choices are important, if history is any guide.