Oocyte Warming and Insemination Consent Form
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Paternal Age on Aneuploidy Rates in First Trimester Pregnancy Loss
Journal of Medical Genetics and Genomics Vol. 2(3), pp. 38-43, August 2010 Available online at http://www.academicjournals.org/jmgg ©2010 Academic Journals Full Length Research Paper Effect of paternal age on aneuploidy rates in first trimester pregnancy loss Vitaly A. Kushnir, Richard T. Scott and John L. Frattarelli 1Department of Obstetrics, Gynecology and Women’s Health, New Jersey Medical School, MSB E-506, 185 South Orange Avenue, Newark, NJ, 07101-1709, USA. 2Department of Obstetrics, Gynecology and Reproductive Sciences, Robert Wood Johnson Medical School UMDNJ, Division of Reproductive Endocrinology and Infertility, New Brunswick, NJ. Reproductive Medicine Associates of New Jersey, Morristown NJ, USA. Accepted 16 July, 2010 A retrospective cohort analysis of patients undergoing IVF cycles at an academic IVF center was performed to test the hypothesis that male age may influence aneuploidy rates in first trimester pregnancy losses. All patients had a first trimester pregnancy loss followed by evacuation of the pregnancy and karyotyping of the abortus. Couples undergoing anonymous donor oocyte ART cycles (n = 50) and 23 couples with female age less than 30 years undergoing autologous oocyte ART cycles were included. The oocyte age was less than 30 in both groups; thereby allowing the focus to be on the reproductive potential of the aging male. The main outcome measure was the effect of paternal age on aneuploidy rate. No increase in aneuploidy rate was noted with increasing paternal age (<40 years = 25.0%; 40-50 years = 38.8%; >50 years = 25.0%). Although there was a significant difference in the male partner age between oocyte recipients and young patients using autologous oocytes (33.7 7.6 vs. -

Oocyte Cryopreservation for Fertility Preservation in Postpubertal Female Children at Risk for Premature Ovarian Failure Due To
Original Study Oocyte Cryopreservation for Fertility Preservation in Postpubertal Female Children at Risk for Premature Ovarian Failure Due to Accelerated Follicle Loss in Turner Syndrome or Cancer Treatments K. Oktay MD 1,2,*, G. Bedoschi MD 1,2 1 Innovation Institute for Fertility Preservation and IVF, New York, NY 2 Laboratory of Molecular Reproduction and Fertility Preservation, Obstetrics and Gynecology, New York Medical College, Valhalla, NY abstract Objective: To preliminarily study the feasibility of oocyte cryopreservation in postpubertal girls aged between 13 and 15 years who were at risk for premature ovarian failure due to the accelerated follicle loss associated with Turner syndrome or cancer treatments. Design: Retrospective cohort and review of literature. Setting: Academic fertility preservation unit. Participants: Three girls diagnosed with Turner syndrome, 1 girl diagnosed with germ-cell tumor. and 1 girl diagnosed with lymphoblastic leukemia. Interventions: Assessment of ovarian reserve, ovarian stimulation, oocyte retrieval, in vitro maturation, and mature oocyte cryopreservation. Main Outcome Measure: Response to ovarian stimulation, number of mature oocytes cryopreserved and complications, if any. Results: Mean anti-mullerian€ hormone, baseline follical stimulating hormone, estradiol, and antral follicle counts were 1.30 Æ 0.39, 6.08 Æ 2.63, 41.39 Æ 24.68, 8.0 Æ 3.2; respectively. In Turner girls the ovarian reserve assessment indicated already diminished ovarian reserve. Ovarian stimulation and oocyte cryopreservation was successfully performed in all female children referred for fertility preser- vation. A range of 4-11 mature oocytes (mean 8.1 Æ 3.4) was cryopreserved without any complications. All girls tolerated the procedure well. -
![Oogenesis [PDF]](https://docslib.b-cdn.net/cover/2902/oogenesis-pdf-452902.webp)
Oogenesis [PDF]
Oogenesis Dr Navneet Kumar Professor (Anatomy) K.G.M.U Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Development of ovum (oogenesis) • Maturation of follicle • Fate of ovum and follicle Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Site – ovary • Duration – 7th week of embryo –primordial germ cells • -3rd month of fetus –oogonium • - two million primary oocyte • -7th month of fetus primary oocyte +primary follicle • - at birth primary oocyte with prophase of • 1st meiotic division • - 40 thousand primary oocyte in adult ovary • - 500 primary oocyte attain maturity • - oogenesis completed after fertilization Dr Navneet Kumar Dr NavneetKumar Professor Professor (Anatomy) Anatomy KGMU Lko K.G.M.U Development of ovum Oogonium(44XX) -In fetal ovary Primary oocyte (44XX) arrest till puberty in prophase of 1st phase meiotic division Secondary oocyte(22X)+Polar body(22X) 1st phase meiotic division completed at ovulation &enter in 2nd phase Ovum(22X)+polarbody(22X) After fertilization Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Dr Navneet Kumar Dr ProfessorNavneetKumar (Anatomy) Professor K.G.M.UAnatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Primordial follicle -Follicular cells Primary follicle -Zona pallucida -Granulosa cells Secondary follicle Antrum developed Ovarian /Graafian follicle - Theca interna &externa -Membrana granulosa -Antrial -

Progression from Meiosis I to Meiosis II in Xenopus Oocytes Requires De
Proc. Natl. Acad. Sci. USA Vol. 88, pp. 5794-5798, July 1991 Biochemistry Progression from meiosis I to meiosis II in Xenopus oocytes requires de novo translation of the mosxe protooncogene (cell cycle/protein kinase/maturation-promoting factor/germinal vesicle breakdown) JOHN P. KANKI* AND DANIEL J. DONOGHUEt Department of Chemistry, Division of Biochemistry and Center for Molecular Genetics, University of California at San Diego, La Jolla, CA 92093-0322 Communicated by Russell F. Doolittle, March 22, 1991 ABSTRACT The meiotic maturation of Xenopus oocytes controlling entry into and exit from M phase (for reviews, see exhibits an early requirement for expression of the mosxe refs. 17-19). protooncogene. The mosxc protein has also been shown to be a In Xenopus, protein synthesis is required for the initiation component of cytostatic factor (CSF), which is responsible for of meiosis I and also meiosis II (4, 20), even though stage VI arrest at metaphase ofmeiosis II. In this study, we have assayed oocytes already contain both p34cdc2 and cyclin (12, 21). the appearance of CSF activity in oocytes induced to mature These proteins are partially complexed in an inactive form of either by progesterone treatment or by overexpression ofmosxe. MPF (preMPF) that appears to be normally inhibited by a Progesterone-stimulated oocytes did not exhibit CSF activity protein phosphatase activity called "INH" (22, 23). These until 30-60 min after germinal vesicle breakdown (GVBD). observations indicate a translational requirement, both for Both the appearance of CSF activity and the progression from the initiation of maturation and for progression to meiosis II, meiosis I to meiosis II were inhibited by microinjection of mos"e for a regulatory factor(s) other than cyclin. -

Educational Objectives Current IVF Practice
2/23/2015 Update from the IVF Lab: Preimplantation Genetic Testing Janet McLaren Bouknight, MD Reproductive Endocrinology and Infertility Department of Obstetrics & Gynecology Educational Objectives • Gain familiarity with the procedures and pregnancy outcomes of current in vitro fertilization practices. • Understand the application of Preimplantation Genetic Diagnosis (PGD) for single‐gene disorders. • Appreciate the role of Preimplantation Genetic Screening (PGS) in maximizing IVF cycle efficiency and encouraging elective single embryo transfer. Current IVF Practice 1 2/23/2015 Current IVF Practice 150,000 cycles 65,000 livebirths Current IVF Practice Current IVF Practice All SART Clinics 2012 <35 35‐37 38‐40 41‐42 >42 Pregnancy Rate 47% 38% 30% 20% 9% Live Birth Rate 41% 31% 22% 12% 4% # embryos transfer 1.9 2.0 2.4 2.9 2.9 % Twins 30% 25% 20% 13% 9% • What are the advanced that have contributed to an increase in success in the IVF Lab? • Improved lab conditions • Extended embryo culture • Improvements in embryo cryopreservation 2 2/23/2015 Current IVF Practice: Improved Lab Conditions Current IVF Practice: Improved Lab Conditions Current IVF Practice: Improved Lab Conditions 3 2/23/2015 Current IVF Practice: Extended Embryo Culture Day 3: Cleavage Stage Day 5: Blastocyst Stage • 8‐cells • 200‐300 cells • 30% implantation rate • 50% implantation rate Increased live birth rates seen in “good prognosis” patients who undergo a Day 5 transfer Current IVF Practice: Extended Embryo Culture Current IVF Practice: Extended Embryo Culture • Supports blastocyst transfer for “good prognosis” patients • Opportunity to consider single embryo transfer • May be associated with a small increased risk of monozygotic twinning 4 2/23/2015 Current IVF Practice: Embryo Cryopreservation Cycles • Improvements in freezing techniques (vitrification) have increased success of cryopreserved embryos. -

Oocyte Or Embryo Donation to Women of Advanced Reproductive Age: an Ethics Committee Opinion
ASRM PAGES Oocyte or embryo donation to women of advanced reproductive age: an Ethics Committee opinion Ethics Committee of the American Society for Reproductive Medicine American Society for Reproductive Medicine, Birmingham, Alabama Advanced reproductive age (ARA) is a risk factor for female infertility, pregnancy loss, fetal anomalies, stillbirth, and obstetric com- plications. Oocyte donation reverses the age-related decline in implantation and birth rates of women in their 40s and 50s and restores pregnancy potential beyond menopause. However, obstetrical complications in older patients remain high, particularly related to oper- ative delivery and hypertensive and cardiovascular risks. Physicians should perform a thorough medical evaluation designed to assess the physical fitness of a patient for pregnancy before deciding to attempt transfer of embryos to any woman of advanced reproductive age (>45 years). Embryo transfer should be strongly discouraged or denied to women of ARA with underlying conditions that increase or exacerbate obstetrical risks. Because of concerns related to the high-risk nature of pregnancy, as well as longevity, treatment of women over the age of 55 should generally be discouraged. This statement replaces the earlier ASRM Ethics Committee document of the same name, last published in 2013 (Fertil Steril 2013;100:337–40). (Fertil SterilÒ 2016;106:e3–7. Ó2016 by American Society for Reproductive Medicine.) Key Words: Ethics, third-party reproduction, complications, pregnancy, parenting Discuss: You can discuss -
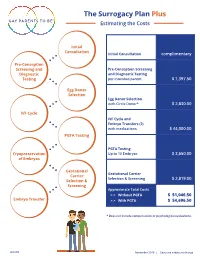
The Surrogacy Plan Plus Estimating the Costs
The Surrogacy Plan Plus Estimating the Costs Initial Consultation Initial Consultation complimentary Pre-Conception Screening and Pre-Conception Screening Diagnostic and Diagnostic Testing Testing per intended parent $ 1,397.50 Egg Donor Selection Egg Donor Selection with Circle Donor* $ 2,830.00 IVF Cycle IVF Cycle and Embryo Transfers (2) with medications $ 44,000.00 PGTA Testing PGTA Testing Cryopreservation Up to 10 Embryos $ 3,650.00 of Embryos Gestational Gestational Carrier Carrier Selection & Screening $ 2,819.00 Selection & Screening Approximate Total Costs > > Without PGTA $ 51,046.50 Embryo Transfer > > With PGTA $ 54,696.50 * Does not include compensation or psychological evaluations. SPP/CD November 2019 | Costs are subject to change The Surrogacy Plan Plus The Surrogacy Plan Plus is available to individuals and couples who want to build a family using a gestational carrrier. In this process, eggs from an egg donor are retrieved and combined with sperm to create embryos. One or two embryos are then transferred into the uterus of the gestational carrier to achieve a pregnancy. How the Surrogacy Plan Plus Works The Surrogacy Plan Plus includes: cycle medication for the oocyte donor and gestational carrier, anesthesia for the retrieval of oocytes, oocyte donor cycle monitoring completed at RMACT, oocyte retrieval, embryology laboratory charges, A simpler approach cryopreservation of embryos, cycle monitoring for the last ultrasound and blood tests to treatment that prior to embryo transfer, embryo transfer into the gestational carrier, and the first year of embryo and specimen storage. If the donor cycle is cancelled prior to retrieval, helps you control the Surrogacy Plan Plus covers the cancellation cost, as well as the cost to rescreen costs with the the same or alternate donor. -

Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal
Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal intimately part of the endocrine responsibility of the ovary. Introduction If there are no gametes, then hormone production is drastically curtailed. Depletion of oocytes implies depletion of the major Oogenesis is an area that has long been of interest in medicine, hormones of the ovary. In the male this is not the case. as well as biology, economics, sociology, and public policy. Androgen production will proceed normally without a single Almost four centuries ago, the English physician William spermatozoa in the testes. Harvey (1578–1657) wrote ex ovo omnia —“all that is alive This chapter presents basic aspects of human ovarian comes from the egg.” follicle growth, oogenesis, and some of the regulatory mech- During a women’s reproductive life span only 300–400 of anisms involved [ 1 ] , as well as some of the basic structural the nearly 1–2 million oocytes present in her ovaries at birth morphology of the testes and the process of development to are ovulated. The process of oogenesis begins with migra- obtain mature spermatozoa. tory primordial germ cells (PGCs). It results in the produc- tion of meiotically competent oocytes containing the correct genetic material, proteins, mRNA transcripts, and organ- Structure of the Ovary elles that are necessary to create a viable embryo. This is a tightly controlled process involving not only ovarian para- The ovary, which contains the germ cells, is the main repro- crine factors but also signaling from gonadotropins secreted ductive organ in the female. -

Infertility Services
Medical Policy Assisted Reproductive Services/Infertility Services Document Number: 002 *Commercial and Qualified Health Plans MassHealth Authorization required X No notification or authorization Not covered X *Not all commercial plans cover this service, please check plan’s benefit package to verify coverage. Contents Overview ....................................................................................................................................................... 2 Coverage Guidelines ..................................................................................................................................... 2 MassHealth, and Certain Custom Plans ........................................................................................................ 2 Covered Services/Procedures ....................................................................................................................... 3 General Eligibility Coverage Criteria ............................................................................................................. 3 SERVICE -SPECIFIC INFERTILITY COVERAGE FOR MEMBERS WITH UTERI and OVARIES ............................... 5 Artificial Insemination (AI)/Intrauterine Insemination (IUI) ......................................................................... 5 Conversion from IUI to In Vitro Fertilization (IVF) ........................................................................................ 6 In Vitro Fertilization (IVF) for Infertility ....................................................................................................... -

Cryopreserved Oocyte Versus Fresh Oocyte Assisted Reproductive Technology Cycles, United States, 2013
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Fertil Steril Manuscript Author . Author manuscript; Manuscript Author available in PMC 2018 January 01. Published in final edited form as: Fertil Steril. 2017 January ; 107(1): 110–118. doi:10.1016/j.fertnstert.2016.10.002. Cryopreserved oocyte versus fresh oocyte assisted reproductive technology cycles, United States, 2013 Sara Crawford, Ph.D.a, Sheree L. Boulet, Dr.P.H., M.P.H.a, Jennifer F. Kawwass, M.D.a,b, Denise J. Jamieson, M.D., M.P.H.a, and Dmitry M. Kissin, M.D., M.P.H.a aDivision of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Emory University, Atlanta, Georgia bDivision of Reproductive Endocrinology and Infertility, Department of Gynecology and Obstetrics, Emory University, Atlanta, Georgia Abstract Objective—To compare characteristics, explore predictors, and compare assisted reproductive technology (ART) cycle, transfer, and pregnancy outcomes of autologous and donor cryopreserved oocyte cycles with fresh oocyte cycles. Design—Retrospective cohort study from the National ART Surveillance System. Setting—Fertility treatment centers. Patient(s)—Fresh embryo cycles initiated in 2013 utilizing embryos created with fresh and cryopreserved, autologous and donor oocytes. Intervention(s)—Cryopreservation of oocytes versus fresh. Main Outcomes Measure(s)—Cancellation, implantation, pregnancy, miscarriage, and live birth rates per cycle, transfer, and/or pregnancy. -

Fertilization: a Sperm's Journey to and Interaction with the Oocyte
Fertilization: a sperm’s journey to and interaction with the oocyte Masahito Ikawa, … , Adam M. Benham, Masaru Okabe J Clin Invest. 2010;120(4):984-994. https://doi.org/10.1172/JCI41585. Review Series Mammalian fertilization comprises sperm migration through the female reproductive tract, biochemical and morphological changes to sperm, and sperm-egg interaction in the oviduct. Recent gene knockout approaches in mice have revealed that many factors previously considered important for fertilization are largely dispensable, or if they are essential, they have an unexpected function. These results indicate that what has been observed in in vitro fertilization (IVF) differs significantly from what occurs during “physiological” fertilization. This Review focuses on the advantages of studying fertilization using gene-manipulated animals and highlights an emerging molecular mechanism of mammalian fertilization. Find the latest version: http://jci.me/41585-pdf Review series Fertilization: a sperm’s journey to and interaction with the oocyte Masahito Ikawa,1 Naokazu Inoue,1 Adam M. Benham,1,2 and Masaru Okabe1 1Research Institute for Microbial Diseases, Osaka University, Osaka, Japan. 2School of Biological and Biomedical Sciences, Durham University, United Kingdom. Mammalian fertilization comprises sperm migration through the female reproductive tract, biochemical and mor- phological changes to sperm, and sperm-egg interaction in the oviduct. Recent gene knockout approaches in mice have revealed that many factors previously considered important for fertilization are largely dispensable, or if they are essential, they have an unexpected function. These results indicate that what has been observed in in vitro fer- tilization (IVF) differs significantly from what occurs during “physiological” fertilization. This Review focuses on the advantages of studying fertilization using gene-manipulated animals and highlights an emerging molecular mechanism of mammalian fertilization. -

Social Freezing: Pressing Pause on Fertility
International Journal of Environmental Research and Public Health Review Social Freezing: Pressing Pause on Fertility Valentin Nicolae Varlas 1,2 , Roxana Georgiana Bors 1,2, Dragos Albu 1,2, Ovidiu Nicolae Penes 3,*, Bogdana Adriana Nasui 4,* , Claudia Mehedintu 5 and Anca Lucia Pop 6 1 Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital, 011171 Bucharest, Romania; [email protected] (V.N.V.); [email protected] (R.G.B.); [email protected] (D.A.) 2 Department of Obstetrics and Gynaecology, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu St., 020021 Bucharest, Romania 3 Department of Intensive Care, University Clinical Hospital, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu St., 020021 Bucharest, Romania 4 Department of Community Health, “Iuliu Hat, ieganu” University of Medicine and Pharmacy, 6 Louis Pasteur Street, 400349 Cluj-Napoca, Romania 5 Department of Obstetrics and Gynaecology, Nicolae Malaxa Clinical Hospital, 020346 Bucharest, Romania; [email protected] 6 Department of Clinical Laboratory, Food Safety, “Carol Davila” University of Medicine and Pharmacy, 6 Traian Vuia Street, 020945 Bucharest, Romania; [email protected] * Correspondence: [email protected] (O.N.P.); [email protected] (B.A.N.) Abstract: Increasing numbers of women are undergoing oocyte or tissue cryopreservation for medical or social reasons to increase their chances of having genetic children. Social egg freezing (SEF) allows women to preserve their fertility in anticipation of age-related fertility decline and ineffective fertility treatments at older ages. The purpose of this study was to summarize recent findings focusing on the challenges of elective egg freezing.