Communicable Disease Control in Emergencies: a Field Manual Edited by M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Review of the Evidence Base for WASH Interventions in Emergency Responses / Relief Operations
A Review of the Evidence Base for WASH interventions in Emergency Responses / Relief Operations A Review of the Evidence Base for WASH interventions in Emergency Responses Discussion document Submitted by Jonathan Parkinson January 2009 January 2009 Page 1 of 56 A Review of the Evidence Base for WASH interventions in Emergency Responses / Relief Operations Executive summary Inadequate sanitation, inadequate water supplies and poor hygiene are critical determinants for survival of victims of natural disasters and conflict situations, especially in the initial stages of a disaster. The most significant are diarrheal diseases and infectious diseases transmitted by the faeco-oral route nd a combination of these factors means that people affected by disasters are also generally much more susceptible to illness and death from disease The traditional response by relief agencies in emergency situations has been to install water supply points and latrines. But experiences have clearly demonstrated the limitations of this approach. More recently hygiene promotion has taken increasingly greater predominance as an integral part of relief agency operations. However, these experiences are diverse and this has led to questions about which type of hygiene promotion activity is most effective and how. Consequently, in the course of the extensive inter-agency consultation, it has emerged that much of the existing evidence base which underpins decision-making for WASH interventions in relief operations is extrapolated from the development sector. It is unclear to the extent to which it is appropriate and relevant in emergency contexts. The primary aim of this assignment was therefore to explore whether it is considered appropriate to apply the existing evidence base for WASH interventions to support emergency operations as it stands and, if not, to consider what activities may be required to improve the evidence base. -

A Sewer Catastrophe Companion
A SEWER CATASTROPHE COMPANION Dry Toilets for Wet Disasters EMERGENCY The year is 20__. The Juan de Fuca tectonic plate has shifted, causing an earthquake with a magnitude of 9.0, devastating the Pacific Northwest. Underground infrastructure has shaken. Sewers are broken and leaking into waterways. You have food and water, your house is still habitable, and your friends and fam- ily are all accounted for. Finally, you can slow down and take stock. You need to poop. Where will you go? RESPONSE This guide presents a toilet system that you can do yourself without relying on a co- ordinated and timely response by someone else. This system served after earthquakes destroyed sanitation systems in Haiti and New Zealand. This guide is for planning ahead and preparing kits, whether for yourself, your household, your apartment building, or your block. This flexible system is built around ubiquitous and freely available 5-gallon buckets. A solution for today that’s Urine itself is sterile, it can be applied to not a problem for tomor- land, dramatically reducing the amount of row. 1. Pee in Bucket material handling. After the earthquake in New Zealand, 2. Poop in Bucket people used separate toilets for poop and pee to reduces material handling, disease risks, and work. Washing hands is fundamental. We de- 3. Wash Hands signed a simple, efficient, and ergonomic portable sink using buckets. A solution for managing Store materials until they can be properly excreta that’s not excreting 1. Cap and processed and treated. This allows time for problems later. an official response and pickup, or to build Store your own compost processing area. -

EMERGENCY WATER SUPPLY GUIDEBOOK for Commercial, Industrial and Institutional Facilities
EMERGENCY WATER SUPPLY GUIDEBOOK For Commercial, Industrial and Institutional Facilities ©LANE PREPAREDNESS COALITION 2016 PAGE 0 ACKNOWLEDGMENTS SUBJECT MATTER EXPERTS This guidebook was written and Many thanks to these volunteers reviewed by Lane Preparedness and their agencies for their work Coalition (LPC) Members who are writing and reviewing this guide. experts in the fields of water supply and distribution, plumbing code, water Project Team Members quality and facility operations. Dr. Geoff Simmons, MD (retired) This guide touches on water supply considerations during a disaster and Harlan Coats, Eugene School District 4J recovery. The intent is to provide Jamie Porter PE, Rainbow Water District general information as a starting point for this important aspect of business Jill Hoyenga, LPC Convener continuity planning. This guide is not meant to replace staff expertise or Laura Farthing PE, Eugene Water & consultation with a professional Electric Board regarding the unique attributes of your Mark Walker, McKenzie Willamette agency or facility. Hospital EUGENE-SPRINGFIELD NATURAL Rob Hallett, City of Eugene HAZARD MITIGATION PLAN Sarah Puls, Lane County Public Health This guide has been produced under the care of the LPC Natural Hazard Steve Graham, City of Springfield Mitigation Plan Sub-Committee. In the 2015 plan, emergency water supply Teresa Kennedy, City of Eugene was called out as a critical need that Thomas Price, SHE had not yet been adequately addressed by our community. This Karen Edmonds, Food for Lane County guide was written to answer to the need for guidance about how Patrick Lowen, Market of Choice businesses can include emergency water supply into their business continuity plans. -
Communicable Disease Control in Emergencies: a Field Manual Edited by M
Communicable disease control in emergencies A field manual Communicable disease control in emergencies A field manual Edited by M.A. Connolly WHO Library Cataloguing-in-Publication Data Communicable disease control in emergencies: a field manual edited by M. A. Connolly. 1.Communicable disease control–methods 2.Emergencies 3.Disease outbreaks–prevention and control 4.Manuals I.Connolly, Máire A. ISBN 92 4 154616 6 (NLM Classification: WA 110) WHO/CDS/2005.27 © World Health Organization, 2005 All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the pert of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on map represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by WHO to verify he information contained in this publication. However, the published material is being distributed without warranty of any kind, either express or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising in its use. -

Eye Disease 1 Eye Disease
Eye disease 1 Eye disease Eye disease Classification and external resources [1] MeSH D005128 This is a partial list of human eye diseases and disorders. The World Health Organisation publishes a classification of known diseases and injuries called the International Statistical Classification of Diseases and Related Health Problems or ICD-10. This list uses that classification. H00-H59 Diseases of the eye and adnexa H00-H06 Disorders of eyelid, lacrimal system and orbit • (H00.0) Hordeolum ("stye" or "sty") — a bacterial infection of sebaceous glands of eyelashes • (H00.1) Chalazion — a cyst in the eyelid (usually upper eyelid) • (H01.0) Blepharitis — inflammation of eyelids and eyelashes; characterized by white flaky skin near the eyelashes • (H02.0) Entropion and trichiasis • (H02.1) Ectropion • (H02.2) Lagophthalmos • (H02.3) Blepharochalasis • (H02.4) Ptosis • (H02.6) Xanthelasma of eyelid • (H03.0*) Parasitic infestation of eyelid in diseases classified elsewhere • Dermatitis of eyelid due to Demodex species ( B88.0+ ) • Parasitic infestation of eyelid in: • leishmaniasis ( B55.-+ ) • loiasis ( B74.3+ ) • onchocerciasis ( B73+ ) • phthiriasis ( B85.3+ ) • (H03.1*) Involvement of eyelid in other infectious diseases classified elsewhere • Involvement of eyelid in: • herpesviral (herpes simplex) infection ( B00.5+ ) • leprosy ( A30.-+ ) • molluscum contagiosum ( B08.1+ ) • tuberculosis ( A18.4+ ) • yaws ( A66.-+ ) • zoster ( B02.3+ ) • (H03.8*) Involvement of eyelid in other diseases classified elsewhere • Involvement of eyelid in impetigo -
In the Prevention of Occupational Diseases 94 7.1 Introduction
Report on the current situation in relation to occupational diseases' systems in EU Member States and EFTA/EEA countries, in particular relative to Commission Recommendation 2003/670/EC concerning the European Schedule of Occupational Diseases and gathering of data on relevant related aspects ‘Report on the current situation in relation to occupational diseases’ systems in EU Member States and EFTA/EEA countries, in particular relative to Commission Recommendation 2003/670/EC concerning the European Schedule of Occupational Diseases and gathering of data on relevant related aspects’ Table of Contents 1 Introduction 4 1.1 Foreword .................................................................................................... 4 1.2 The burden of occupational diseases ......................................................... 4 1.3 Recommendation 2003/670/EC .................................................................. 6 1.4 The EU context .......................................................................................... 9 1.5 Information notices on occupational diseases, a guide to diagnosis .................................................................................................. 11 1.6 Objectives of the project ........................................................................... 11 1.7 Methodology and sources ........................................................................ 12 1.8 Structure of the report .............................................................................. 15 2 Developments -

Gap Analysis in Emergency Water, Sanitation and Hygiene Promotion
Gap Analysis in Emergency Water, Sanitation and Hygiene Promotion Andy Bastable and Lucy Russell, Oxfam GB July 2013 The HIF is supported by The HIF is managed by Contents i Acronyms ii Executive Summary 1 Background 2 Methodology 3 Literature Review Consultation Findings 5 Focus Group Discussions with Beneficiaries 5 Workshops and Discussions at Country or Sub-Country Level 6 Online Practitioner Survey 8 Global WASH Cluster 9 Donor responses to the Questionnaire 10 Consultation findings and discussion 12 of priority gaps Annex 1: Terms of Reference 15 Annex 2: Timeline 16 Annex 3: List of issues raised by each stakeholder group in order of priority 17 Annex 4: Detailed Results from the Literature Review 19 Annex 5: Literature Review References 20 Annex 6: Profile of Online Practitioner Survey Respondents 21 Annex 7: Online Gap Analysis Survey for WASH Practitioners 22 Annex 8: Summary of ‘Other’ Issues raised 25 Annex 9: Detailed Results from Donor Questionnaire 28 Gap Analysis in Emergency Water, Sanitation and Hygiene Promotion Acronyms ACF Action Contre la Faim ALNAP Active Learning Network for Accountability and Performance CARE Cooperative for Assistance and Relief Everywhere CHAST Children’s Hygiene and Sanitation Training CLTS Community Led Total Sanitation CRS Catholic Relief Services DRR Disaster Risk Reduction DFID Department for International Development (UK) DRC Democratic Republic of Congo DWS Drinking Water Supply ECHO Humanitarian Aid and Civil Protection department of the European Commission ELRHA Enhancing Learning and -
Level I Syllabus
LEVEL I SYLLABUS 1 ACDT Course Learning Objectives Upon Completion, Those Enrolled Will Be MODULE Prepared To... The Language of Dermatology 1. Define and spell the following cutaneous lesions/descriptors: a. Macule b. Patch c. Papule d. Nodule e. Cyst f. Plaque g. Wheal h. Vesicle i. Bulla j. Pustule k. Erosion l. Ulcer m. Atrophy n. Scaling o. Crusting p. Excoriations q. Fissures r. Lichenification s. Erythematous t. Violaceous u. Purpuric v. Hypo/Hyperpigmented w. Linear x. Annular y. Nummular/Discoid z. Blaschkoid aa. Morbilliform bb. Polycyclic cc. Arcuate dd. Reticular Collecting & Documenting Patient History Part I 1. Describe the importance of documentation and chart review, while properly collecting dermatologyspecific medical history components, including: a. Chief Complaint b. Past Medical History c. Family History d. Medications e. Allergies Collecting & Documenting Patient History Part II 1. Demonstrate the proper collection of dermatologyspecific medical history and explain the significance of the following: a. Social History b. Review of Systems c. History of Present Illness Anatomy 1. Spell and document the following directional indicators while applying them to the appropriate anatomical landmarks: a. Proximal/Distal b. Superior/Mid/Inferior c. Anterior/Posterior d. Medial/Lateral e. Dorsal/Ventral 2. Spell and identify specific anatomical locations involving the: a. Scalp b. Forehead c. Ears d. Eyes e. Nose f. Cheeks g. Lips h. Chin i. Neck j. Back k. Upper extremity l. Hands m. Nails n. Chest o. Abdomen p. Buttocks q. Hips r. Lower extremity s. Feet Skin Structure and Function 1. Identify and spell the three primary layers of skin: a. -

European Conference on Rare Diseases
EUROPEAN CONFERENCE ON RARE DISEASES Luxembourg 21-22 June 2005 EUROPEAN CONFERENCE ON RARE DISEASES Copyright 2005 © Eurordis For more information: www.eurordis.org Webcast of the conference and abstracts: www.rare-luxembourg2005.org TABLE OF CONTENT_3 ------------------------------------------------- ACKNOWLEDGEMENTS AND CREDITS A specialised clinic for Rare Diseases : the RD TABLE OF CONTENTS Outpatient’s Clinic (RDOC) in Italy …………… 48 ------------------------------------------------- ------------------------------------------------- 4 / RARE, BUT EXISTING The organisers particularly wish to thank ACKNOWLEDGEMENTS AND CREDITS 4.1 No code, no name, no existence …………… 49 ------------------------------------------------- the following persons/organisations/companies 4.2 Why do we need to code rare diseases? … 50 PROGRAMME COMMITTEE for their role : ------------------------------------------------- Members of the Programme Committee ……… 6 5 / RESEARCH AND CARE Conference Programme …………………………… 7 …… HER ROYAL HIGHNESS THE GRAND DUCHESS OF LUXEMBOURG Key features of the conference …………………… 12 5.1 Research for Rare Diseases in the EU 54 • Participants ……………………………………… 12 5.2 Fighting the fragmentation of research …… 55 A multi-disciplinary approach ………………… 55 THE EUROPEAN COMMISSION Funding of the conference ……………………… 14 Transfer of academic research towards • ------------------------------------------------- industrial development ………………………… 60 THE GOVERNEMENT OF LUXEMBOURG Speakers ……………………………………………… 16 Strengthening cooperation between academia -
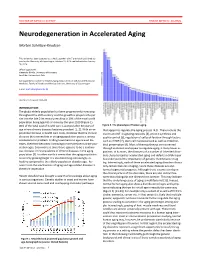
Neurodegeneration in Accelerated Aging
DOCTOR OF MEDICAL SCIENCE DANISH MEDICAL JOURNAL Neurodegeneration in Accelerated Aging Morten Scheibye-Knudsen This review has been accepted as a thesis together with 7 previously published pa- pers by the University of Copenhagen, October 16, 2014 and defended on January 14, 2016 Official opponents: Alexander Bürkle, University of Konstanz Lars Eide, University of Oslo Correspondence: Center for Healthy Aging, Department of Cellular and Molecular Medicine, Faculty of Health and Medical Sciences, University of Copenhagen E-mail: [email protected] Dan Med J 2016;63(11):B5308 INTRODUCTION The global elderly population has been progressively increasing throughout the 20th century and this growth is projected to per- sist into the late 21st century resulting in 20% of the total world population being aged 65 or more by the year 2100 (Figure 1). 80% of the total cost of health care is accrued after 40 years of Figure 2. The phenotype of human aging. age where chronic diseases become prevalent [1, 2]. With an ex- that appear to regulate the aging process [4,5]. These include the ponential increase in health care costs, it follows that the chronic insulin and IGF-1 signaling cascades [4], protein synthesis and diseases that accumulate in an aging population poses a serious quality control [6], regulation of cell proliferation through factors socioeconomic problem. Finding treatments to age related dis- such as mTOR [7], stem cell maintenance 8 as well as mitochon- eases, therefore becomes increasingly more pertinent as the pop- drial preservation [9]. Most of these pathways are conserved ulation ages. Even more so since there appears to be a continu- through evolution and appear to regulate aging in many lower or- ous increase in the prevalence of chronic diseases in the aging ganisms. -

Practical Paper Esos® – Emergency Sanitation Operation System D
156 Practical Paper © IWA Publishing 2015 Journal of Water, Sanitation and Hygiene for Development | 05.1 | 2015 Practical Paper eSOS® – emergency Sanitation Operation System D. Brdjanovic, F. Zakaria, P. M. Mawioo, H. A. Garcia, C. M. Hooijmans, J. C´ urko, Y. P. Thye and T. Setiadi ABSTRACT This paper presents the innovative emergency Sanitation Operation System (eSOS) concept created D. Brdjanovic (corresponding author) F. Zakaria to improve the entire emergency sanitation chain and provide decent sanitation to people in need. P. M. Mawioo H. A. Garcia The eSOS kit is described including its components: eSOS smart toilets, an intelligent excreta C. M. Hooijmans Environmental Engineering and Water Technology collection vehicle-tracking system, a decentralized excreta treatment facility, an emergency Department, UNESCO-IHE, sanitation coordination center, and an integrated eSOS communication and management system. P.O. Box 3015, 2601 DA Delft, The Netherlands The paper further deals with costs and the eSOS business model, its challenges, applicability and E-mail: [email protected]; [email protected] relevance. The first application, currently taking place in the Philippines will bring valuable insights on D. Brdjanovic the future of the eSOS smart toilet. It is expected that eSOS will bring changes to traditional disaster Faculty of Applied Sciences, Department of Biotechnology, relief management. Delft University of Technology, Key words | emergency, feces, sanitation, technology, toilet, urine Julianalaan 67, 2628 BC Delft, The Netherlands J. Curko Faculty of Food Technology and Biotechnology, University of Zagreb, Pierottijeva 6, 10000 Zagreb, Croatia Y. P. Thye T. Setiadi Department of Chemical Engineering, Faculty of Industrial Technology, Institut Teknologi Bandung, Jl. -

Managing Communicable Diseases in Child Care Settings
MANAGING COMMUNICABLE DISEASES IN CHILD CARE SETTINGS Prepared jointly by: Child Care Licensing Division Michigan Department of Licensing and Regulatory Affairs and Divisions of Communicable Disease & Immunization Michigan Department of Health and Human Services Ways to Keep Children and Adults Healthy It is very common for children and adults to become ill in a child care setting. There are a number of steps child care providers and staff can take to prevent or reduce the incidents of illness among children and adults in the child care setting. You can also refer to the publication Let’s Keep It Healthy – Policies and Procedures for a Safe and Healthy Environment. Hand Washing Hand washing is one of the most effective way to prevent the spread of illness. Hands should be washed frequently including after diapering, toileting, caring for an ill child, and coming into contact with bodily fluids (such as nose wiping), before feeding, eating and handling food, and at any time hands are soiled. Note: The use of disposable gloves during diapering does not eliminate the need for hand washing. The use of gloves is not required during diapering. However, if gloves are used, caregivers must still wash their hands after each diaper change. Instructions for effective hand washing are: 1. Wet hands under warm, running water. 2. Apply liquid soap. Antibacterial soap is not recommended. 3. Vigorously rub hands together for at least 20 seconds to lather all surfaces of the hands. Pay special attention to cleaning under fingernails and thumbs. 4. Thoroughly rinse hands under warm, running water. 5.