Cosmetic Dermatology Pricing and Procedures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
July 2020 Goal the Goal of the Residency Program Is to Develop Future Leaders in Both Research and Clinical Medicine
Residency Training Program July 2020 Goal The goal of the Residency Program is to develop future leaders in both research and clinical medicine. Flexibility within the program allows for the acquisition of fundamental working knowledge in all subspecialties of dermatology. All residents are taught a scholarly approach to patient care, aimed at integrating clinicopathologic observation with an understanding of the basic pathophysiologic processes of normal and abnormal skin. Penn’s Residency Program consists of conferences, seminars, clinical rotations, research, and an opportunity to participate in the teaching of medical students. An extensive introduction into the department and the William D. James, M.D. Director of Residency Program clinic/patient care service is given to first-year residents. A distinguished clinical faculty and research faculty, coupled with the clinical and laboratory facilities, provides residents with comprehensive training. An appreciation of and participation in the investigative process is an integral part of our residency. Graduates frequently earn clinical or basic science fellowship appointments at universities across the country. Examples of these include: pediatric dermatology, dermatopathology, dermatologic surgery, dermatoepidemiology, postdoctoral and Clinical Educator fellowships. Additional post graduate training has occurred at the NIH and CDC. Graduates of our program populate the faculty at Harvard, Penn, Johns Hopkins, MD Anderson, Dartmouth, Penn State, Washington University, and the Universities of Washington, Pittsburgh, Vermont, South Carolina, Massachusetts, Wisconsin, and the University of California San Francisco. Additionally, some enter private practice to become pillars of community medicine. Misha A. Rosenbach, M.D. Associate Director of Residency Program History The first medical school in America, founded in 1765, was named the College of Philadelphia. -

Wound Healing: a Paradigm for Regeneration
SYMPOSIUM ON REGENERATIVE MEDICINE Wound Healing: A Paradigm for Regeneration Victor W. Wong, MD; Geoffrey C. Gurtner, MD; and Michael T. Longaker, MD, MBA From the Hagey Laboratory for Pediatric Regenerative Medi- CME Activity cine, Department of Surgery, Stanford University, Stanford, Target Audience: The target audience for Mayo Clinic Proceedings is primar- relationships with any commercial interest related to the subject matter ily internal medicine physicians and other clinicians who wish to advance of the educational activity. Safeguards against commercial bias have been CA. their current knowledge of clinical medicine and who wish to stay abreast put in place. Faculty also will disclose any off-label and/or investigational of advances in medical research. use of pharmaceuticals or instruments discussed in their presentation. Statement of Need: General internists and primary care physicians must Disclosure of this information will be published in course materials so maintain an extensive knowledge base on a wide variety of topics covering that those participants in the activity may formulate their own judgments all body systems as well as common and uncommon disorders. Mayo Clinic regarding the presentation. Proceedings aims to leverage the expertise of its authors to help physicians In their editorial and administrative roles, William L. Lanier, Jr, MD, Terry L. understand best practices in diagnosis and management of conditions Jopke, Kimberly D. Sankey, and Nicki M. Smith, MPA, have control of the encountered in the clinical setting. content of this program but have no relevant financial relationship(s) with Accreditation: College of Medicine, Mayo Clinic is accredited by the Accred- industry. itation Council for Continuing Medical Education to provide continuing med- The authors report no competing interests. -

General Dermatology Practice Brochure
Appointments Our Providers David A. Cowan, MD, FAAD We are currently accepting • Fellow, American Academy of Dermatology new patients. • Associate, American College of Call today to schedule your appointment Mohs Micrographic Surgery Monday - Friday, 8:00am to 4:30pm Rebecca G. Pomerantz, MD 1-877-661-3376 • Board Certified, American Academy of Cancellations & “No Show” Policy Dermatology If you are unable to keep your scheduled Lisa L. Ellis, MPAS, PA-C appointment, please call the office and we will • Member, American Academy of Physician be more than happy to reschedule for you. Assistants Failure to notify us at least 48 hours prior to your • Member, PA Society of Physician Assistants Medical and appointment may result in a cancellation fee. • Member, Society of Dermatology Physician Prescription Refills Assistants Surgical Refill requests are handled during normal office Sheri L. Rolewski, MSN, CRNP-BC hours when our staff has full access to medical • National Board Certification, Family Nurse Dermatology records. Refills cannot be called in on holidays, Practitioner Specialty weekends or more than twelve months after your • Member, Dermatology Nurse Association last exam. Please have your pharmacy contact our office directly. Test Results SMy Dermatology Appointment You will be notified when we receive your Date/Day _____________________________________ pathology or other test results, usually within two weeks from the date of your procedure. If you Time _________________________________________ do not hear from us within three -

Dermatology at the Berkeley Outpatient Center
Dermatology Berkeley Outpatient Center Overview Encompassing both medical and cosmetic dermatology, our experts at the Berkeley Outpatient Center offer a full range of diagnostic, treatment and surgical services for patients with cutaneous conditions. Surgical Dermatology • Fellowship-trained expertise in • Close coordination with Plastic Surgery Mohs micrographic surgery for at the Berkeley Outpatient Center, treatment of skin cancers including allowing for streamlined treatment for basal cell carcinomas and squamous related procedures in one location cell carcinomas, as well as treatment of • Outpatient surgery for removal of melanoma in situ with MART-1 staining benign skin growths and skin cancers Medical Dermatology - Conditions Treated/Services Offered • Acne, rosacea and related conditions • Mole/Atypical nevus/Melanoma • Sun-damaged skin surveillance • Aesthetic/Cosmetic dermatology • Non-melanoma skin cancers • Eczema and atopic dermatitis • Pigmentation disorders • HIV/AIDS-related skin conditions • Psoriasis • Lumps under the skin • Rashes • Infections of the skin (bacterial, viral, • Skin checks for patients with fungal and other) concerning lesions • Melanoma • Warts When to see a Dermatologist For more information, please call Dermatology Services at (510) 985-5200. Dermatology Services Providing integrated care in the community. Our Dermatology Team Erin Amerson, MD Drew Saylor, MD, MPH UCSF Health UCSF Health Dermatologist Dermatologic surgeon To learn more about our doctors, visit ucsfhealth.org/find_a_doctor. Office location: Berkeley Outpatient Center 3100 San Pablo Avenue Berkeley, CA 94702 (510) 985-5200 To learn more about our Berkeley Outpatient Center, Adeline St visit johnmuirhealth.com/ September 2020 berkeleyopc.. -

Post-Summer Skin Repair
36 RIVIERA WELLNESS POST-SUMMER SKIN REPAIR Healthy, radiant skin begins from within season of summer indulgences, whe- Niacin (B3) is found in avocado and turkey and ther it be swimming in chlorinated pools, helps to speed up skin cell regeneration - essen- A several weeks of rosé wine, or too much tial for repairing sun damage, acne hyperpigmen- sun bathing, our skin can look a little worse for tation, and reduces the symptoms of rosacea. wear. Once the summer holidays are over, we Niacin also helps your skin to retain moisture, so can be left with dehydrated and perhaps wrinkly make sure you are properly hydrated! Turkey has skin, sun damage, blocked pores and chapped 30 x more niacin than avocado. lips. So what´s the best remedy? Good nutrition Green Tea - Epigallocatechin gallate (EGCG), the can help protect the skin not just pre-holiday antioxidant found in green tea has been shown season, but also post-holiday to help the skin re- prevent genetic damage in skin cells exposed to pair. UV radiation. A large mug of green tea (250ml) The skin can be thought of as the window to ove- with a squeeze of fresh lemon juice to add the rall health of the body. It is the largest elimination vitamin C may help achieve that post-summer route for toxins, so an overworked liver from a glow! long summer of excesses can show up on the skin. The simplest step to a fresher complexion DON´T FORGET is to address water intake. Well-hydrated skin LIFESTYLE FACTORS! looks plump and less wrinkled. -
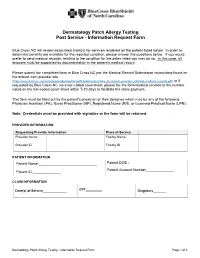
Dermatology Patch Allergy Testing Post Service - Information Request Form
Dermatology Patch Allergy Testing Post Service - Information Request Form Blue Cross NC will review associated claim(s) for services rendered on the patient listed below. In order to determine benefits are available for the reported condition, please answer the questions below. If you would prefer to send medical records, relating to the condition for the dates listed you may do so. In this case, all answers must be supported by documentation in the patient's medical record. Please submit the completed form to Blue Cross NC per the Medical Record Submission instructions found on the bcbsnc.com provider site (https://www.bcbsnc.com/assets/providers/public/pdfs/submissions/how_to_submit_provider_initiated_medical_records.pdf) or if requested by Blue Cross NC via a bar-coded coversheet, please fax the form/medical records to the number noted on the bar-coded cover sheet within 7-10 days to facilitate the claim payment. This form must be filled out by the patient's physician or their designee which may be any of the following: Physician Assistant (PA), Nurse Practitioner (NP), Registered Nurse (RN), or Licensed Practical Nurse (LPN). Note: Credentials must be provided with signature or the form will be returned. PROVIDER INFORMATION Requesting Provider Information Place of Service Provider Name Facility Name Provider ID Facility ID PATIENT INFORMATION Patient Name:_____________________________ Patient DOB :_____________ Patient Account Number______________ Patient ID:______________ CLAIM INFORMATION Date(s) of Service_____________ CPT_________ Diagnosis_______ Dermatology Patch Allergy Testing - Information Request Form Page 1 of 3 CLINICAL INFORMATION Did the patient have direct skin testing (for immediate hypersensitivity) by: Percutaneous or epicutaneous (scratch, prick, or puncture)? ________________ Intradermal testing? ___________________________________ Inhalant allergy evaluation? _________________ Did the patient have patch (application) testing (most commonly used: T.R.U.E. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous, -
Concepts of Sliding and Lifting Tissue Movement in Flap Reconstruction
HOW I DO IT/BACK TO BASICS This new feature will emphasize innovative and better ways to perform dermatologic surgery procedures. This ar- ticle should be based on some evidence-based literature, but may describe the author’s experience with a particular procedure without being a typical clinical research article. The Editor will consider ideas for topics. Any author who is considering writing an article should submit the title to Ronald L. Moy, MD, Editor-in-Chief, 100 UCLA Medical Plaza, Suite 590, Los Angeles, CA 90024. Concepts of Sliding and Lifting Tissue Movement in Flap Reconstruction Timothy M. Johnson, MD,*†‡ Neil Swanson, MD,§ and Shan R. Baker, MD† Departments of *Dermatology, †Otorhinolaryngology, and ‡Surgery, University of Michigan Medical Center, Ann Arbor, Michigan, and §Department of Dermatology and Otolaryngology, Oregon Health Sciences, Portland Oregon background. The optimal design of a skin flap requires an the answer to three predictable events that result from tissue understanding of the concepts of tissue movement. transfer: Where is the tension? Where are the final incision objective. The purpose of this manuscript was to demon- lines? Where is the redundant tissue? strate concepts of sliding and lifting tissue movement for flap conclusion. A mental exercise assessing all available recon- reconstruction. struction options should be performed for each individual pa- methods. Six similar defects located in the forehead–temple– tient and defect. Both patient and defect considerations need to eyebrow region were repaired using a different skin flap. be assessed. A thorough understanding of both anatomy and tis- results. The specific flap design for a given defect is based on sue movement is necessary for optimal skin flap reconstruction. -

Surgical Treatment Options for Lower Eyelid Aging Joe Niamtu III, DMD
COSMETIC TECHNIQUE Surgical Treatment Options for Lower Eyelid Aging Joe Niamtu III, DMD The lower eyelid and associated anatomy represent a complex structure that is key in facial aging and rejuvenation. There are numerous ways to address this region and some of the more common treat- ment options are discussed in this article. A review is presented of the diagnosis and popular treatment options to address the most common aspects of eyelid aging. The author has performed cosmetic lower eyelid surgery using transconjunctival blepharoplasty with skin resurfacing for the past 12 years, with pleasing results and low complications. Lower eyelid rejuvenation is one of the most commonly requested procedures in a cosmetic surgery practice. A firm understanding of the complex anatomy of this region is paramount to successful treatment. Although many methods exist for addressing this region, some techniques are more prone to postoperative complications. The author has had continued success with hundreds of patients by performing transconjunctival lower eyelid blepharoplasty with CO2 laser resurfacing, chemicalCOS peels, or skin-pinch DERM procedures. These procedures are safe, predictable, and have a place in theDo armamentarium Not of contemporary Copy cosmetic surgeons. ermatochalasis is the crepey, wrinkled, The basis of this article concerns skin aging and its loose, and sun damaged skin of the eye- surgical correction, but discussion of the periorbital fat is lids. Because age-associated changes to germane to the understanding of the aging process and its the upper face often present earlier than correction. The periorbital fat is an essential evolutionary age-associated changes to the lower face, system that serves in part to cushion the globe within its itD is not uncommon for the cosmetic surgery practitioner bony orbit. -

Sweat Glands • Oil Glands • Mammary Glands
Chapter 4 The Integumentary System Lecture Presentation by Steven Bassett Southeast Community College © 2015 Pearson Education, Inc. Introduction • The integumentary system is composed of: • Skin • Hair • Nails • Sweat glands • Oil glands • Mammary glands © 2015 Pearson Education, Inc. Introduction • The skin is the most visible organ of the body • Clinicians can tell a lot about the overall health of the body by examining the skin • Skin helps protect from the environment • Skin helps to regulate body temperature © 2015 Pearson Education, Inc. Integumentary Structure and Function • Cutaneous Membrane • Epidermis • Dermis • Accessory Structures • Hair follicles • Exocrine glands • Nails © 2015 Pearson Education, Inc. Figure 4.1 Functional Organization of the Integumentary System Integumentary System FUNCTIONS • Physical protection from • Synthesis and storage • Coordination of immune • Sensory information • Excretion environmental hazards of lipid reserves response to pathogens • Synthesis of vitamin D3 • Thermoregulation and cancers in skin Cutaneous Membrane Accessory Structures Epidermis Dermis Hair Follicles Exocrine Glands Nails • Protects dermis from Papillary Layer Reticular Layer • Produce hairs that • Assist in • Protect and trauma, chemicals protect skull thermoregulation support tips • Nourishes and • Restricts spread of • Controls skin permeability, • Produce hairs that • Excrete wastes of fingers and supports pathogens prevents water loss provide delicate • Lubricate toes epidermis penetrating epidermis • Prevents entry of -

Genetics of Hair and Skin Color
11 Sep 2003 14:51 AR AR201-GE37-04.tex AR201-GE37-04.sgm LaTeX2e(2002/01/18) P1: GCE 10.1146/annurev.genet.37.110801.143233 Annu. Rev. Genet. 2003. 37:67–90 doi: 10.1146/annurev.genet.37.110801.143233 Copyright c 2003 by Annual Reviews. All rights reserved First published online as a Review in Advance on June 17, 2003 GENETICS OF HAIR AND SKIN COLOR Jonathan L. Rees Systems Group, Dermatology, University of Edinburgh, Lauriston Buildings, Lauriston Place, Edinburgh, EH3 9YW, United Kingdom; email: [email protected] Key Words melanin, melanocortin 1 receptor (MC1R), eumelanin, pheomelanin, red hair ■ Abstract Differences in skin and hair color are principally genetically deter- mined and are due to variation in the amount, type, and packaging of melanin polymers produced by melanocytes secreted into keratinocytes. Pigmentary phenotype is genet- ically complex and at a physiological level complicated. Genes determining a number of rare Mendelian disorders of pigmentation such as albinism have been identified, but only one gene, the melanocortin 1 receptor (MCR1), has so far been identified to explain variation in the normal population such as that leading to red hair, freckling, and sun-sensitivity. Genotype-phenotype relations of the MC1R are reviewed, as well as methods to improve the phenotypic assessment of human pigmentary status. It is argued that given advances in model systems, increases in technical facility, and the lower cost of genotype assessment, the lack of standardized phenotype assessment is now a major limit on advance. CONTENTS INTRODUCTION ..................................................... 68 BIOLOGY OF HUMAN PIGMENTATION ................................ 69 by San Jose State University on 10/05/10. -

Skin 1. Describe the Basic Histological Structure of the Skin, Identifying The
Skin lecture notes 1 Lecture objectives: skin 1. Describe the basic histological structure of the skin, identifying the layers of the skin and their embryologic origin. 2. Identify the cell layers that constitute the epidermis and the differences between thick and thin skin. 3. Describe the cellular components of the epidermis and their function: keratinocytes, melanocytes, Langerhans cells and Merkel cells: 4. Describe the structural organization of the dermis and the components of the papillary and reticular layers. 5. Identify other structures present in the skin: vessels, skin sensorial receptors, hair follicles and hairs, nails and glands. 6. Understand the mechanism of skin repair 7. Describe histological findings in common skin diseases. Skin lecture notes 2 HISTOLOGY OF THE SKIN The skin is the heaviest, largest single organ of the body. It protects the body against physical, chemical and biological agents. The skin participates in the maintenance of body temperature and hydration, and in the excretion of metabolites. It also contributes to homeostasis through the production of hormones, cytokines and growth factors. 1. Describe the basic histological structure of the skin, identifying the layers of the skin and their embryologic origin. The skin is composed of the epidermis, an epithelial layer of ectodermal origin and the dermis, a layer of connective tissue of mesodermal origin. The hypodermis or subcutaneous tissue, which is not considered part of the skin proper, lies deep to the dermis and is formed by loose connective tissue that typically contains adipose cells. Skin layers 2. Identify the cell layers that constitute the epidermis and the differences between thick and thin skin.