High Thermoregulatory Strain During Competitive Paratriathlon Racing in the Heat
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
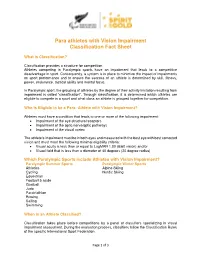
Para Athletes with Vision Impairment Classification Fact Sheet
Para athletes with Vision Impairment Classification Fact Sheet What is Classification? Classification provides a structure for competition. Athletes competing in Paralympic sports have an impairment that leads to a competitive disadvantage in sport. Consequently, a system is in place to minimize the impact of impairments on sport performance and to ensure the success of an athlete is determined by skill, fitness, power, endurance, tactical ability and mental focus. In Paralympic sport, the grouping of athletes by the degree of their activity limitation resulting from impairment is called “classification”. Through classification, it is determined which athletes are eligible to compete in a sport and what class an athlete is grouped together for competition. Who is Eligible to be a Para- Athlete with Vision Impairment? Athletes must have a condition that leads to one or more of the following impairment: • Impairment of the eye structure/receptors • Impairment of the optic nerve/optic pathways • Impairment of the visual cortex The athlete’s impairment must be in both eyes and measured with the best eye with best corrected vision and must meet the following minimal eligibility criteria: • Visual acuity is less than or equal to LogMAR 1.00 (6/60 vision) and/or • Visual field that is less than a diameter of 40 degrees (20 degree radius) Which Paralympic Sports include Athletes with Vision Impairment? Paralympic Summer Sports Paralympic Winter Sports Athletics Alpine Skiing Cycling Nordic Skiing Equestrian Football 5 aside Goalball Judo Paratriathlon Rowing Sailing Swimming When is an Athlete Classified? Classification takes place before competitions by a panel of classifiers specializing in visual impairment assessment. -

Tokyo 2020 Paralympic Games
TOKYO 2020 PARALYMPIC GAMES QUALIFICATION REGULATIONS REVISED EDITION, APRIL 2021 INTERNATIONAL PARALYMPIC COMMITTEE 2 CONTENTS 1. Introduction 2. Tokyo 2020 Paralympic Games Programme Overview 3. General IPC Regulations on Eligibility 4. IPC Redistribution Policy of Vacant Qualification Slots 5. Universality Wild Cards 6. Key Dates 7. Archery 8. Athletics 9. Badminton 10. Boccia 11. Canoe 12. Cycling (Track and Road) 13. Equestrian 14. Football 5-a-side 15. Goalball 16. Judo 17. Powerlifting 18. Rowing 19. Shooting 20. Swimming 21. Table Tennis 22. Taekwondo 23. Triathlon 24. Volleyball (Sitting) 25. Wheelchair Basketball 26. Wheelchair Fencing 27. Wheelchair Rugby 28. Wheelchair Tennis 29. Glossary 30. Register of Updates INTERNATIONAL PARALYMPIC COMMITTEE 3 INTRODUCTION These Qualification Regulations (Regulations) describe in detail how athletes and teams can qualify for the Tokyo 2020 Paralympic Games in each of the twenty- two (22) sports on the Tokyo 2020 Paralympic Games Programme (Games Programme). It provides to the National Paralympic Committees (NPCs), to National Federations (NFs), to sports administrators, coaches and to the athletes themselves the conditions that allow participation in the signature event of the Paralympic Movement. These Regulations present: • an overview of the Games Programme; • the general IPC regulations on eligibility; • the specific qualification criteria for each sport (in alphabetical order); and • a glossary of the terminology used throughout the Regulations. STRUCTURE OF SPORT-SPECIFIC QUALIFICATION -

U.S. Department of Veterans Affairs (VA)
U.S. Department of Veterans Affairs (VA) Veteran Monthly Assistance Allowance for Disabled Veterans Training in Paralympic and Olympic Sports Program (VMAA) In partnership with the United States Olympic Committee and other Olympic and Paralympic entities within the United States, VA supports eligible service and non-service-connected military Veterans in their efforts to represent Team USA at the Paralympic Games, Olympic Games and other international sport competitions. The VA Office of National Veterans Sports Programs & Special Events provides a monthly assistance allowance for disabled Veterans training in Paralympic sports, as well as certain disabled Veterans selected for or competing with the national Olympic Team, as authorized by 38 U.S.C. 322(d) and Section 703 of the Veterans’ Benefits Improvement Act of 2008. Through the program, VA will pay a monthly allowance to a Veteran with either a service-connected or non-service-connected disability if the Veteran meets the minimum military standards or higher (i.e. Emerging Athlete or National Team) in his or her respective Paralympic sport at a recognized competition. In addition to making the VMAA standard, an athlete must also be nationally or internationally classified by his or her respective Paralympic sport federation as eligible for Paralympic competition. VA will also pay a monthly allowance to a Veteran with a service-connected disability rated 30 percent or greater by VA who is selected for a national Olympic Team for any month in which the Veteran is competing in any event sanctioned by the National Governing Bodies of the Olympic Sport in the United State, in accordance with P.L. -

Bridge II Sports Boccia Buzz December 2019
Bridge II Sports Boccia Buzz December 2019 A Brief History of Boccia Have you every wondered where Boccia came from and Play Boccia at home over the holidays! how it got started? Share the fun of Boccia with family and friends over the The game of Bocce (with an e) started a long time ago in break. Here are some tips. Italy and is now played all over the world. Boccia (with an ia) is the version of bocce developed for people with disabilities. It was introduced at the Paralympic Games in What Balls to use playing Boccia at home 1984. Boccia was originally presented as a sport for You can use different types of balls to play Boccia at people with cerebral palsy, but is now open to any one home such as tennis balls, whiffle balls, or softballs and with a disability that impairs motor function that wants baseballs. to play it. Boccia tests several of an athlete’s abilities. It tests concentration, coordination, accuracy and their ability to strategize. There are different groups around the state and country that play the game of Boccia and host practices and competitions. Individuals can play single matches, in pairs or they can play on a team. The object of Boccia is Boccia Court Layout to throw your ball closest to the jack ball. In Bocce A regulation court is 10 x 6 meters with 2.5 meter players use wooden balls as well as clay balls. In Boccia we use official boccia balls that are softer to play on a deep throwing boxes. -

Diversity & Paralympic Sports
Summus Sports Group REPORT DIVERSITY & PARALYMPIC SPORTS UNITED KINGDOM Main Reference: 1.BBC Sport, Rio Paralympics 2016: The Great Britain team 2.uksport.org.uk Summus Sports Group REPORT Overview This is a summary of our findings on the racial demographic of ParalympicsGB at the Rio 2016 Summer Paralympic Games. We looked at at: 1 The whole team 2 Individual sports 3 The funding model This report was pulled together in light of recent events in an attempt to help drive a conversation around diversity within Paralympic sports. This report does not seek to challenge the effectiveness of the system but the fairness of it. Summus Sports Group REPORT Context Based on a 2011 census the general population of England and Wales, Scotland and Northern Ireland is broken down as as follows: 82.3% White 17.7% Non-White Summus Sports Group REPORT ParalympicsGB In 2016 ParalympicsGB sent 260 athletes to Rio for the 2016 Summer Paralympic Games. The break down of that team was as follows: 93% White 7% Non-White This does not include competition partners in Boccia and accounts for the fact that Kadeena Cox represented the team in both athletics and cycling. Summus Sports Group REPORT Rio '16 The 260 athletes that went to Rio in 2016 representing ParalympicsGB made up 19 teams. Of the 19 non-white athletes, 12 of them came from 3 sports: 5 Athletics 4 Wheelchair Basketball 3 Wheelchair Rugby That equates to 7 non-white athletes out of a possible 169 across the remaining 16 sports, a representation of around 4%. -

Beijing 2022 Paralympic Winter Games
BEIJING 2022 PARALYMPIC WINTER GAMES QUALIFICATION REGULATIONS December 2020 2 CONTENTS INTRODUCTION 3 BEIJING 2022 PARALYMPIC PROGRAMME OVERVIEW 5 GENERAL IPC REGULATIONS ON ELIGIBILITY 6 BIPARTITE INVITATIONS 7 REDISTRIBUTION OF UNUSED QUALIFICATION SLOTS 8 KEY DATES 9 PARA ALPINE SKIING 10 PARA ICE HOCKEY 15 PARA NORDIC SKIING 18 PARA SNOWBOARD 23 WHEELCHAIR CURLING 27 GLOSSARY 31 REGISTER OF UPDATES 33 3 INTRODUCTION This publication describes in detail how athletes can qualify for the Beijing 2022 Paralympic Winter Games in each of the five sports on the Games programme. It provides to National Paralympic Committees, National Sport Federations, sports administrators, coaches and to the athletes themselves the conditions that allow participation in the winter sports signature event of the Paralympic Movement. Presented here are: • An overview of the Beijing 2022 Paralympic Programme, • the general IPC regulations on eligibility, • the specific qualification criteria for each sport (in alphabetical order), • a glossary of the terminology used throughout the document. STRUCTURE OF SPORT-SPECIFIC QUALIFICATION CRITERIA Each sport-specific section in this publication follows a standardized format. Readers can quickly locate information or cross-reference it between sports. The standard structure of each sport-specific qualification criteria is as follows: • Events • Athlete Quotas • Allocation of Qualification Slots • Maximum Quota Allocation per NPC • Athlete Eligibility • Maximum Entries per NPC • Qualification System • Timeline • Confirmation -
Good Practice Guidance
GOOD PRACTICE GUIDANCE BOCCIA – Enhancing the quality of life of people with disabilities and their environment through Paralympic sport Boccia Dedicated to Erasmus + applicants and beneficiaries and for all whose purpose is to empow- er people with disabilities to enjoy the opportunity to practice sports. This publication reflects only the author’s views, and the Commission cannot be held respon- sible for any use which may be made of the information contained therein Substantive consultant PhD Piotr Urbański, University of Physical Education, Poznań Boccia Good Practice Guidance Table of contents PART I Introduction p. 3 1. Idea of the Project p. 4 2. Design of the Project p. 6 2.1. Main goals of the Project p. 6 2.2. Target group selection p. 7 2.3. Age and gender group selection p. 7 2.4. Partner selection p. 8 2.5. Staff selection p. 9 2.6. Project Main Activities p. 10 3. Project Participants and Results p. 11 3.1 Bulgaria p. 11 3.2 Greece p. 15 3.3 Georgia p. 18 3.4 FYR of Macedonia p. 21 3.5 Turkey p. 25 3.6 Poland p. 28 4. General results p. 32 4.1. Main activities of the Project p. 32 4.2. Outputs of the Project p. 34 5. Quality control during Project implementation p. 35 6. Dissemination and summary p. 36 7. Good Practice Recommendation p. 37 8. Links p. 40 PART II BOCCIA – description of the game p. 41 Boccia Good Practice Guidance Introduction This guidance was prepared on base of our experience gained during implementation of Erasmus+ Sport Project: BOCCIA – Enhancing the quality of life of people with disabilities and their environment through paralympic sport Boccia (2015-2017). -

A Review Study on Paralympic Games
International Journal of Sports and Physical Education (IJSPE) Volume 4, Issue 1, 2018, PP 19-24 ISSN 2454-6380 http://dx.doi.org/10.20431/2454-6380.0401005 www.arcjournals.org A Review Study on Paralympic Games Dr. SandipSankarGhosh1, Miss. SampaBhowmick2 Assistant Professors, University of Kalyani, Kalyani, Nadia-741235, West Bengal, India. M.P.Ed student, University of Kalyani, Kalyani, Nadia-741235, West Bengal, India. *Corresponding Author: Dr. SandipSankarGhosh, Assistant Professors, University of Kalyani, Kalyani, Nadia-741235, West Bengal, India Abstract: The word “Paralympic” derives from the Greek preposition “para” (beside or alongside) and the word “Olympic”. Its meaning is that Paralympics are the parallel Games to the Olympics and illustrates how the two movements exist side-by-side (https://www.paralympic.org). The Paralympic Games is a major international multi sports event involving athletes with a range of disabilities, including impaired muscle power, impaired passive range of movement, limb deficiency, leg length difference, short stature, hypertonia, ataxia, athetosis, vision impairment and intellectual impairment. The first Paralympic Games took place in Rome, Italy in 1960 featuring 400 athletes from 23 countries. Since then they have taken place every four years. As of 2016 summer Paralympic games was included 22 sports and 526 medal events. The IPC has established ten disability categories, including physical, visual, and intellectual impairment. Last Paralympic was held in Rio de Janeiro and upcoming Paralympic -

Tokyo 2020 Paralympic Games Qualification Regulations
Tokyo 2020 Paralympic Games Qualification Regulations August 2019 International Paralympic Committee Adenauerallee 212-214 Tel. +49 228 2097-200 www.paralympic.org 53113 Bonn, Germany Fax +49 228 2097-209 [email protected] CONTENTS 1. Introduction 2. Tokyo 2020 Paralympic Games Programme Overview 3. General IPC Regulations on Eligibility 4. IPC Redistribution Policy of Vacant Qualification Slots 5. Universality Wild Cards 6. Key Dates 7. Archery 8. Athletics 9. Badminton 10. Boccia 11. Canoe 12. Cycling (Track and Road) 13. Equestrian 14. Football 5-a-side 15. Goalball 16. Judo 17. Powerlifting 18. Rowing 19. Shooting 20. Swimming 21. Table Tennis 22. Taekwondo 23. Triathlon 24. Volleyball (Sitting) 25. Wheelchair Basketball 26. Wheelchair Fencing 27. Wheelchair Rugby 28. Wheelchair Tennis 29. Glossary 30. Register of Updates Tokyo 2020 Paralympic Games – Qualification Regulations 2 INTRODUCTION These Qualification Regulations (Regulations) describe in detail how athletes and teams can qualify for the Tokyo 2020 Paralympic Games in each of the twenty-two (22) sports on the Tokyo 2020 Paralympic Games Programme (Games Programme). It provides to the National Paralympic Committees (NPCs), to National Federations (NFs), to sports administrators, coaches and to the athletes themselves the conditions that allow participation in the signature event of the Paralympic Movement. These Regulations present: . an overview of the Games Programme; . the general IPC regulations on eligibility; . the specific qualification criteria for each sport (in alphabetical order); and . a glossary of the terminology used throughout the Regulations. Structure of sport-specific qualification criteria Each sport-specific section in these Regulations follows a standardised format. Readers can quickly locate information or cross-reference it between sports. -
The Paralympic Athlete Dedicated to the Memory of Trevor Williams Who Inspired the Editors in 1997 to Write This Book
This page intentionally left blank Handbook of Sports Medicine and Science The Paralympic Athlete Dedicated to the memory of Trevor Williams who inspired the editors in 1997 to write this book. Handbook of Sports Medicine and Science The Paralympic Athlete AN IOC MEDICAL COMMISSION PUBLICATION EDITED BY Yves C. Vanlandewijck PhD, PT Full professor at the Katholieke Universiteit Leuven Faculty of Kinesiology and Rehabilitation Sciences Department of Rehabilitation Sciences Leuven, Belgium Walter R. Thompson PhD Regents Professor Kinesiology and Health (College of Education) Nutrition (College of Health and Human Sciences) Georgia State University Atlanta, GA USA This edition fi rst published 2011 © 2011 International Olympic Committee Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -

Tokyo 2020 Paralympic Games
TOKYO 2020 PARALYMPIC GAMES QUALIFICATION REGULATIONS REVISED EDITION, APRIL 2021 INTERNATIONAL PARALYMPIC COMMITTEE 2 CONTENTS 1. Introduction 2. Tokyo 2020 Paralympic Games Programme Overview 3. General IPC Regulations on Eligibility 4. IPC Redistribution Policy of Vacant Qualification Slots 5. Universality Wild Cards 6. Key Dates 7. Archery 8. Athletics 9. Badminton 10. Boccia 11. Canoe 12. Cycling (Track and Road) 13. Equestrian 14. Football 5-a-side 15. Goalball 16. Judo 17. Powerlifting 18. Rowing 19. Shooting 20. Swimming 21. Table Tennis 22. Taekwondo 23. Triathlon 24. Volleyball (Sitting) 25. Wheelchair Basketball 26. Wheelchair Fencing 27. Wheelchair Rugby 28. Wheelchair Tennis 29. Glossary 30. Register of Updates INTERNATIONAL PARALYMPIC COMMITTEE 3 INTRODUCTION These Qualification Regulations (Regulations) describe in detail how athletes and teams can qualify for the Tokyo 2020 Paralympic Games in each of the twenty- two (22) sports on the Tokyo 2020 Paralympic Games Programme (Games Programme). It provides to the National Paralympic Committees (NPCs), to National Federations (NFs), to sports administrators, coaches and to the athletes themselves the conditions that allow participation in the signature event of the Paralympic Movement. These Regulations present: • an overview of the Games Programme; • the general IPC regulations on eligibility; • the specific qualification criteria for each sport (in alphabetical order); and • a glossary of the terminology used throughout the Regulations. STRUCTURE OF SPORT-SPECIFIC QUALIFICATION -

Snow Australia Paraalpine
SNOW AUSTRALIA PARA!ALPINE ATHLETE PATHWAY A PATHWAY FOR ALL nowsports is a sport for all, whether Each stage of the Snow Australia Athlete it’s participating recreationally with Pathway provides an overview of athlete Sfamily and friends, or competitively preparation, programs, on and off-snow in snowsports event. With approximately 1.2 development, equipment, competition, million Australians participating in various leadership and support. It is designed to forms of skiing and snowboarding, it is one inform our community about the Pathways of Australia’s largest and most popular to High Performance, and to support our participation sports. Program Providers to deliver long-term athlete development opportunities. Whatever the motivation for participating in Snowsports, Snow Australia is committed This document supports materials available to providing a clear “Pathways to High on the Snow Australia website which is an Performance” strategy, to educate and inform important conduit for the latest information the Snowsports Community as to the stages on the Snow Australia Athlete Pathway. of athletic development I encourage anyone interested in the To assist with this important initiative, Snow snowsports athlete journey to read and Australia has developed discipline specific become familiar with this important resource. Snow Australia Pathway ‘blueprints’, informed by the Australian Institute of Sport’s (AIS) Michael Kennedy FTEM (Foundation, Talent, Elite and Mastery) Snow Australia CEO Athlete framework. The blueprint provides an evidence-based and practicable approach for supporting the ‘whole of sport’ pathway continuum and the three key outcomes of sport being: • Active Lifestyle, • Sports Participation; • Sporting Excellence. SNOW AUSTRALIA PARA!ALPINE ATHLETE PATHWAY WHAT IS WHY DO WE NEED FTEM? THE FTEM MODEL? ports development begins early in THE ATHLETE PATHWAY IS AN life with the acquisition of movement THE SNOW AUSTRALIA skills through to lifelong engagement INCLUSIVE AND PROGRESSIVE S ATHLETE PATHWAY into senior levels.