Caring for Yourself and Your New Baby
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WSHA Member Hospitals
WSHA Member Hospitals www.wsha.org WHATCOM BELLINGHAM REPUBLIC TONASKET Ferry County Memorial Hospital SAN JUAN PeaceHealth St. Joseph Medical Center OKANOGAN North Valley Hospital STEVENS SEDRO-WOOLLEY PEND SKAGIT PeaceHealth United General Medical Center OMAK OREILLE FRIDAY HARBOR MT. VERNON Mid-Valley Hospital F ERRY COLVILLE PeaceHealth Peace ANACORTES Skagit Valley Hospital Providence Mount Carmel Hospital Island Medical Center Island Hospital CHEWELAH ISLAND Providence St. Joseph’s Hospital COUPEVILLE ARLINGTON WhidbeyHealth Cascade Valley Hospital & Clinics BREWSTER MARYSVILLE Three Rivers Hospital NEWPORT Newport Hospital & Health Services CLALLAM PORT ANGELES Smokey Point Behavioral Health Olympic Medical Center PORT TOWNSEND EVERETT SNOHOMISH CHELAN FORKS Jefferson Healthcare Providence Regional Medical Center Everett SPOKANE Forks Community Hospital CHELAN GRAND COULEE BURIEN Lake Chelan Community Coulee Medical Center SEATTLE EDMONDS MONROE Hospital & Clinics SPOKANE VALLEY Highline Swedish Edmonds EvergreenHealth Monroe MultiCare Valley Hospital Kindred Hospital Seattle – Medical Center JEFFERSON KIRKLAND DAVENPORT Northgate & First Hill Regional Fairfax Behavioral Health DOUGLAS Lincoln Hospital u Navos Hospital for uSEATTLE EvergreenHealth LEAVENWORTH SPOKANE & MEDICAL LAKE Seattle Cancer Care Alliance Respiratory & See list BELLEVUE Cascade Medical Center See list Seattle Children’s Complex Care KITSAP Overlake Medical Center KING ISSAQUAH — Swedish/Issaquah MultiCare Deaconess Hospital Swedish Ballard BREMERTON BURIEN -

Participating Organization Locations UMP Plus – PSHVN Hospitals, Emergency Departments And/Or Trauma Centers and Clinics, Including Urgent Care
Network Organizations: Edmonds Family Medicine EvergreenHealth Partners MultiCare Connected Care Overlake Medical Center Rockwood Health System Seattle Children’s SignalHealth Virginia Mason Participating Organization Locations UMP Plus – PSHVN hospitals, emergency departments and/or trauma centers and clinics, including urgent care: Grays Harbor County ° EvergreenHealth Neuropsychological Services EvergreenHealth Orthopedic and Sports Care Grays Harbor Community Hospital and Harbor ° Medical Group (Part of MultiCare Connected Care) ° EvergreenHealth Orthopedic and Sports Care Monroe EvergreenHealth Orthpedics and Sports Medicine-Coral •• 915 Anderson Dr., Aberdeen, WA 98520 ° ° EvergreenHealth Pain Care ° 1006 North H St., Aberdeen, WA 98520 (East Campus) ° EvergreenHealth Parkinson’s Services EvergreenHealth Primary Care, Canyon Park King County ° ° EvergreenHealth Primary Care, Duvall EvergreenHealth Partners ° EvergreenHealth Primary Care, Kenmore ° Advanced Dermatology Northwest ° EvergreenHealth Primary Care, Monroe ° Advanced Family Medicine, PLLC •• EvergreenHealth Primary Care, Emergency Care & ° Aria Endocrinology, LLC Urgent Care Redmond ° Associated Gastroenterology of Northwest ° EvergreenHealth Primary Care, Sammamish ° Bellevue Bone & Joint Physicians, PLLC ° EvergreenHealth Primary Care, Sultan ° Bellevue Endocrine Consultants • EvergreenHealth Primary Care and Urgent Care Woodinville ° Bellevue Family Medicine ° EvergreenHealth Pulmonary Care ° Bellevue Lasik & Cataract ° EvergreenHealth Radiation Oncology ° Bel-Red Internal -
Quality Counts: Choose the Right Hospital and Doctor for You in The: Seattle Area
Quality Counts: Choose the right hospital and doctor for you in the: Seattle area WHAT IS TRANSPARENCY? Transparency in healthcare means having facts about cost and quality. As costs rise and provider networks narrow, it’s crucial that consumers have access to transparent information to make informed decisions when selecting the right hospital and the right doctor for their care. When presented with objective information about physician experience and related hospital quality, % OF PATIENTS 8would select5 a different physician than they did before doing their homework.* IN THE U.S. Consumers need to research the hospitals where physicians practice. Getting the right care means selecting the right doctor and the highest quality hospital for their care needs. MORE THAN 222,392 OUT LIVES POTENTIALLY OF COULD HAVE patients1 received care6 in 1-star BEEN SAVED hospitals with higher if all hospitals performed than expected mortality rates similarly to hospitals receiving or complication rates.** 5-stars.*** IN THE SEATTLE AREA Fortunately only By doing their homework, % consumers can select the of10.6 patients receive care right doctor and right in hospitals with higher than hospital for their care expected mortality rates or complication rates.** needs in the Seattle area. The Top Performers Before beginning their care journey, consumers should start their research at Healthgrades.com, where they can find the right hospital and the right doctor based on information physicians say matters most. By doing their homework, consumers can actively -

Swedish Seattle Community Health Needs Assessment First Hill Campus and Cherry Hill Campus 2016- 2018
Swedish Seattle Community Health Needs Assessment First Hill Campus and Cherry Hill Campus 2016- 2018 Table of contents 2016 Community Health Needs Assessment Executive summary……………………...... 3 Acknowledgements……………………...... 5 Introduction………………………………..... 6 Creating healthier communities, together serving King and Snohomish counties. About Swedish……………………………… 12 Description of community………………….. 14 Population and age demographics Ethnicity Income levels and housing Health care and coverage Process, participants and health indicators… 17 Assessment process Participants Data collection and analysis Health indicators and trends Identified priority health needs………………. 19 Leading health issues and baseline data Prioritization process and criteria 2016-2018 CHNA approval ………………….. 23 Appendices…………………………………….. 24 2 | P a g e Executive Summary Swedish Medical Center is a member of King County Hospitals for a Healthier Community (HHC) a collaborative of all 12 hospitals and health systems in King County and Public Health-Seattle & King County. For this report, HHC members joined forces to identify the most important health needs in the communities they serve and to develop strategies that address those needs. HHC members have also worked together to increase access to healthy foods and beverages in their facilities and to address access-to-care issues by assisting with enrollment of residents in free or low-cost health insurance. Using the HHC Assessment as a foundation, each of Swedish hospitals developed its own CHNA and implementation strategy reflecting the findings from the collaborative. These Community Health Needs Assessments (CHNA) are a collaborative product that fulfills Section 9007 of the Affordable Care Act. Each CHNA presents data on: Description of the Community Life Expectancy and Leading Causes of Death Chronic Illness We invited community coalitions and organizations to tell us about the assets and resources that help their communities thrive. -

Trauma Designated
Washington State Department of Health Trauma Services Region Trauma Designation Facility City Adult Pediatric Rehab Central I I P IR Harborview Medical Center Seattle III Multicare Auburn Medical Center Auburn III EvergreenHealth Medical Center Kirkland III Overlake Hospital Medical Center Bellevue III Valley Medical Center Renton IV St. Anne Medical Center (Formerly Highline Medical Center) Burien University of Washington Medical Center – Northwest Campus IV Seattle (Formerly NW Hospital) IV St. Francis Hospital Federal Way V St. Elizabeth Hospital Enumclaw V Snoqualmie Valley Hospital Snoqualmie I PR Seattle Children’s Hospital Seattle East II II P Providence Sacred Heart Medical Center & Children’s Hospital Spokane III Deaconess Hospital / MULTICARE HEALTH SYSTEM Spokane III Providence Holy Family Hospital Spokane III St. Joseph Regional Medical Center Lewiston, ID III Valley Hospital / MULTICARE HEALTH SYSTEM Spokane Valley IV Newport Hospital & Health Services Newport IV Providence Mount Carmel Hospital Colville IV Providence St. Joseph’s Hospital Chewelah IV Pullman Regional Hospital Pullman IV Tri-State Memorial Hospital Clarkston V East Adams Rural Healthcare Ritzville V Ferry County Memorial Hospital Republic V Garfield County Memorial Hospital Pomeroy V Lincoln Hospital Davenport V Odessa Memorial Healthcare Center Odessa V Othello Community Hospital Othello V Whitman Hospital & Medical Center Colfax I PR-I R St. Luke’s Rehabilitation Institute Spokane North III Island Hospital Anacortes II PeaceHealth St. Joseph Medical Center -
WA ER Physicians Group Directory Listing.Xlsx
City In-Network Hospital ER Physician group serving the hospital ER Physician Group Network Status Tacoma Allenmore Hospital Tacoma Emergency Care Physicians Out of Network Olympia Capital Medical Center Thurston Emergency Group In-Network Leavenworth Cascade Medical Center Cascade Medical Center In-Network Arlington Cascade Valley Hospital Northwest Emergency Physicians In-Network Wenatchee Central Washington Hospital Central Washington Hospital In-Network Ephrata Columbia Basin Hospital Beezley Springs Inpatient Services Out of Network Grand Coulee Coulee Medical Center Coulee Medical Center In-Network Dayton Dayton General Hospital Dayton General Hospital In-Network Spokane Deaconess Medical Center Spokane Emergency Group In-Network Ritzville East Adams Rural Hospital East Adams Rural Hospital In-Network Kirkland EvergreenHealth Medical Center Evergreen Emergency Services In-Network Monroe EvergreenHealth Monroe Evergreen Emergency Services In-Network Republic Ferry County Memorial Hospital Barton Out of Network Republic Ferry County Memorial Hospital CompHealth Out of Network Republic Ferry County Memorial Hospital Staff Care Inc. Out of Network Forks Forks Community Hospital Forks Community Hospital In-Network Pomeroy Garfield County Memorial Hospital Garfield County Memorial Hospital In-Network Puyallup Good Samaritan Hospital Mt. Rainier Emergency Physicians Out of Network Aberdeen Grays Harbor Community Hospital Grays Harbor Emergency Physicians In-Network Seattle Harborview Medical Center Emergency Department at Harborview and -

WA ER Physicians Group Directory Listing 12312019.Xlsx
ER Physician group serving the ER Physician Group City In-Network Hospital hospital Network Status Olympia Capital Medical Center Thurston Emergency Group In-Network Leavenwort Cascade Medical Center Cascade Medical Center In-Network Arlington Cascade Valley Hospital Northwest Emergency Physicians In-Network Wenatchee Central Washington Hospital Central Washington Hospital In-Network Ephrata Columbia Basin Hospital Beezley Springs Inpatient Services Out of Network Grand Coulee Medical Center Coulee Medical Center In-Network Dayton Dayton General Hospital Dayton General Hospital In-Network Ritzville East Adams Rural Hospital East Adams Rural Hospital In-Network Kirkland EvergreenHealth Medical Center Evergreen Emergency Services In-Network Monroe EvergreenHealth Monroe Evergreen Emergency Services In-Network Republic Ferry County Memorial Hospital Barton Out of Network Republic Ferry County Memorial Hospital CompHealth Out of Network Republic Ferry County Memorial Hospital Staff Care Inc. Out of Network Forks Forks Community Hospital Forks Community Hospital In-Network Pomeroy Garfield County Memorial Hospital Garfield County Memorial Hospital In-Network Aberdeen Grays Harbor Community Hospital Grays Harbor Emergency Physicians In-Network Emergency Department at Harborview and Harborview Medical Seattle Harborview Medical Center Center Emergency Medicine In-Network Bremerton Harrison Medical Center West Sound Emergency Physicians Out of Network Silverdale Harrison Medical Center West Sound Emergency Physicians Out of Network Burien Highline -

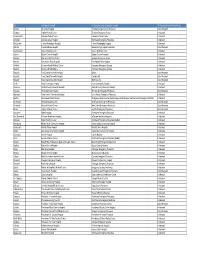
WA Hospitals Accreditation and Health Grades
WA Hospitals Accreditation And Health Grades Washington Hospital Street Address City State Zip Code Phone Contact WA County Quality Data Link Accreditation Link https://www.qualitycheck.org/quality- https://www.healthgrades.com/hospital-directory/washington-wa/capital-medical-center- Capital Medical Center 3900 Capitol Mall Dr SW Olympia WA 98502-8654 (360)956-2550 Thurston report/?keyword=Capital%20Medical%20Center&sitestate=WA&ajax=1&json=1&callback=jQuery110207711982 hgstcdea6bc6500139?autosuggest=true 552875212_1475254399557&_=1475254399558&bsnid=9604 https://www.healthgrades.com/hospital-directory/washington-wa/cascade-medical-center- Cascade Medical Center 817 Commercial St Leavenworth WA 98826-1316 (509)548-5815 Chelan hgst5334700f501313 https://www.healthgrades.com/hospital-directory/washington-wa/cascade-valley-hospital- http://dnvglhealthcare.com/hospitals?search_type=and&q=cascade+valley+hospital&c=&c=&c=19215&prSubmi Cascade Valley Hospital 330 S Stillaguamish Ave Arlington WA 98223-1642 (360)435-2133 Snohomish hgsta9ea6bc6500060 t=Search https://www.qualitycheck.org/quality- https://www.healthgrades.com/hospital-directory/washington-wa/central-washington-hospital-and-clinics- Central Washington Hospital 1201 S Miller St Wenatchee WA 98801-3201 (509)662-1511 Chelan report/?keyword=Central%20Washington%20Hospital&sitestate=WA&ajax=1&json=1&callback=jQuery1102015 hgstc8fcc8b6500016 7774803620993_1475254329796&_=1475254329797&bsnid=9656 https://www.healthgrades.com/hospital-directory/washington-wa/columbia-basin-hospital- Columbia -

WSHA Member Hospitals
WSHA Member Hospitals www.wsha.org WHATCOM BELLINGHAM REPUBLIC TONASKET Ferry County Memorial Hospital SAN JUAN PeaceHealth St. Joseph Medical Center OKANOGAN North Valley Hospital STEVENS SEDRO-WOOLLEY PEND SKAGIT PeaceHealth United General Medical Center OMAK OREILLE FRIDAY HARBOR MT. VERNON Mid-Valley Hospital F ERRY COLVILLE PeaceHealth Peace ANACORTES Skagit Valley Hospital Providence Mount Carmel Hospital Island Medical Center Island Hospital CHEWELAH ISLAND Providence St. Joseph’s Hospital COUPEVILLE ARLINGTON WhidbeyHealth Cascade Valley Hospital & Clinics BREWSTER MARYSVILLE Three Rivers Hospital NEWPORT Newport Hospital & Health Services CLALLAM PORT ANGELES Smokey Point Behavioral Health Olympic Medical Center PORT TOWNSEND EVERETT SNOHOMISH CHELAN FORKS Jefferson Healthcare Providence Regional Medical Center Everett SPOKANE Forks Community Hospital CHELAN GRAND COULEE BURIEN Lake Chelan Community Coulee Medical Center SEATTLE EDMONDS MONROE Hospital & Clinics SPOKANE VALLEY Highline Swedish Edmonds EvergreenHealth Monroe MultiCare Valley Hospital Kindred Hospital Seattle – Medical Center JEFFERSON KIRKLAND DAVENPORT Northgate & First Hill Regional Fairfax Behavioral Health DOUGLAS Lincoln Hospital u Navos Hospital for uSEATTLE EvergreenHealth LEAVENWORTH SPOKANE & MEDICAL LAKE Seattle Cancer Care Alliance Respiratory & See list BELLEVUE Cascade Medical Center See list Seattle Children’s Complex Care KITSAP Overlake Medical Center KING ISSAQUAH — Swedish/Issaquah MultiCare Deaconess Hospital Swedish Ballard BREMERTON BURIEN -

In Network ER Hospital List
Emergency Room Provider Directory Premera Blue Cross Member Plans Last updated March 4, 2021 To make sure your benefits cover ER services at their highest level, use the following list to see if the ER physicians group serving our participating hospitals is in-network. The cost to you for receiving ER services from an out-of-network ER physicians group may be higher even when received at an in-network hospital. Table of Contents: Section 1: Heritage and Heritage and Dental Choice Networks Section 2: Heritage Prime Network Section 3: Heritage Signature and Dental Choice, and Individual Signature Networks Section 4: Tahoma and Tahoma and Dental Choice Networks Section 1: Heritage and Heritage and Dental Choice ER Physician Group City State In-Network Hospital ER Physician Group Servicing the Hospital Network Status Olympia WA Capital Medical Center Thurston Emergency Group In-Network Leavenworth WA Cascade Medical Center Cascade Medical Center In-Network Arlington WA Cascade Valley Hospital Northwest Emergency Physicians In-Network Wenatchee WA Central Washington Hospital Central Washington Hospital In-Network Ephrata WA Columbia Basin Hospital Beezley Springs Inpatient Services In-Network Astoria OR Columbia Memorial Hospital Oregon Health & Science University (OHSU) Out-of-Network Grand Coulee WA Coulee Medical Center Coulee Medical Center In-Network Dayton WA Dayton General Hospital Dayton General Hospital In-Network Ritzville WA East Adams Rural Hospital East Adams Rural Hospital In-Network Premera Blue Cross is an Independent Licensee -

Heritage Signature Brochure for Employers
FOR EMPLOYERS Heritage Signature Network This provider network is available to groups with 1–50 employees Premera’s Heritage Signature Key benefits network is ideal if you want to offer your employees a high- There are 37,442 in-network providers across Washington state, including Providence Health & benefit, low-cost plan with easy Good Access Services hospitals, physicians, and other providers. access to a large provider network Includes access to the BlueCard Program for care outside of Washington. within Washington state. Your employees can even get care Providers in the Heritage Signature network have when they work or travel contracted with Premera to keep the total cost of outside of Washington through care low. Lower Costs the benefits of having a Your company could save up to 5% on premiums.* Premera Blue Cross health plan. Your employees could save up to 5% on out-of- pocket costs.* Providers in the Heritage Signature network Quality Care commit to providing customers with the care they need, when they need it, and in the right way. Your employees will pay less whenever they use in-network providers. The Find a Doctor tool on Easy Search premera.com makes it easy to search for in- network doctors, hospitals, and other providers. Help your employees use the Find a Doctor tool by visiting B’link, Premera’s online resource center for employers. B’link provides a customizable flyer, copy-and-share messages, and other simple tools. Visit the B’link website at blink.premera.com. *Cost savings are based on a comparison with Heritage, Premera’s largest provider network. -

Blue Distinction Centers of Care by Designation
Blue Distinction Centers of Care by Designation This document provides comparative quality information on selected specialties as well as high level comparative pricing information. BDC+ designated facilities offer patients the greatest value as specialty procedures at these facilities are both cost efficient and high quality. BDC designated facilities are high-quality but do not meet the specialty specific threshold for cost. Designation Designation BDC+ BDC BDC+ BDC Bariatric Maternity EvergreenHealth Medical Center Kirkland ✔ EvergreenHealth Medical Center Kirkland ✔ Multicare Deaconess Hospital Spokane ✔ Highline Medical Center Burien ✔ Overlake Hospital Medical Center Bellevue ✔ Kadlec Regional Medical Center Richland ✔ Providence Regional Medical Center Everett ✔ Multicare Deaconess Hospital Spokane ✔ Northwest Weight Loss, Sound Surgeons Everett ✔ Multicare Valley Hospital Spokane ✔ Swedish Medical Center First Hill Seattle ✔ Northwest Hospital & Medical Center Seattle ✔ University of Washington Medical Center Seattle ✔ Providence Sacred Heart Medical Center & Children's Hospital Spokane ✔ Virginia Mason Medical Center Seattle ✔ Skagit Valley Hospital Mount Vernon ✔ St Francis Community Hospital Federal Way ✔ Trios Women's and Children's Hospital Kennewick ✔ Tacoma General Allenmore Tacoma ✔ Valley Medical Center Renton ✔ Cancer Care Peacehealth St. Joseph Medical Center Bellingham ✔ Northwest Medical Specialties Tacoma ✔ Providence Regional Medical Center Everett ✔ Cardiac Care St Elizabeth Enumclaw ✔ Kadlec Regional Medical Center