ICF-Based CPG Presentation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -

The Painful Heel Comparative Study in Rheumatoid Arthritis, Ankylosing Spondylitis, Reiter's Syndrome, and Generalized Osteoarthrosis
Ann Rheum Dis: first published as 10.1136/ard.36.4.343 on 1 August 1977. Downloaded from Annals of the Rheumatic Diseases, 1977, 36, 343-348 The painful heel Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthrosis J. C. GERSTER, T. L. VISCHER, A. BENNANI, AND G. H. FALLET From the Department of Medicine, Division of Rheumatology, University Hospital, Geneva, Switzerland SUMMARY This study presents the frequency of severe and mild talalgias in unselected, consecutive patients with rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthosis. Achilles tendinitis and plantar fasciitis caused a severe talalgia and they were observed mainly in males with Reiter's syndrome or ankylosing spondylitis. On the other hand, sub-Achilles bursitis more frequently affected women with rheumatoid arthritis and rarely gave rise to severe talalgias. The simple calcaneal spur was associated with generalized osteoarthrosis and its frequency increased with age. This condition was not related to talalgias. Finally, clinical and radiological involvement of the subtalar and midtarsal joints were observed mainly in rheumatoid arthritis and occasionally caused apes valgoplanus. copyright. A 'painful heel' syndrome occurs at times in patients psoriasis, urethritis, conjunctivitis, or enterocolitis. with inflammatory rheumatic disease or osteo- The antigen HLA B27 was present in 29 patients arthrosis, causing significant clinical problems. Very (80%O). few studies have investigated the frequency and characteristics of this syndrome. Therefore we have RS 16 PATIENTS studied unselected groups of patients with rheuma- All of our patients had the complete triad (non- toid arthritis (RA), ankylosing spondylitis (AS), gonococcal urethritis, arthritis, and conjunctivitis). -

The Pathomechanics of Plantar Fasciitis
Sports Med 2006; 36 (7): 585-611 REVIEW ARTICLE 0112-1642/06/0007-0585/$39.95/0 2006 Adis Data Information BV. All rights reserved. The Pathomechanics of Plantar Fasciitis Scott C. Wearing,1 James E. Smeathers,1 Stephen R. Urry,1 Ewald M. Hennig2 and Andrew P. Hills1 1 Institute of Health and Biomedical Innovation, Queensland University of Technology, Kelvin Grove, Queensland, Australia 2 Biomechanik Labor, University Duisburg-Essen, Essen, Germany Contents Abstract ....................................................................................585 1. Anatomy of the Plantar Fascia ............................................................586 1.1 Gross Anatomy of the Plantar Fascia...................................................586 1.2 Histological Anatomy of the Plantar Fascia .............................................589 1.2.1 Neuroanatomy ................................................................590 1.2.2 Microcirculation ...............................................................590 1.2.3 The Enthesis ...................................................................590 2. Mechanical Properties of the Plantar Fascia ................................................592 2.1 Structural Properties ..................................................................593 2.2 Material Properties ...................................................................593 3. Mechanical Function of the Plantar Fascia .................................................594 3.1 Quasistatic Models of Plantar Fascial Function ..........................................594 -

Conditions Related to Inflammatory Arthritis
Conditions Related to Inflammatory Arthritis There are many conditions related to inflammatory arthritis. Some exhibit symptoms similar to those of inflammatory arthritis, some are autoimmune disorders that result from inflammatory arthritis, and some occur in conjunction with inflammatory arthritis. Related conditions are listed for information purposes only. • Adhesive capsulitis – also known as “frozen shoulder,” the connective tissue surrounding the joint becomes stiff and inflamed causing extreme pain and greatly restricting movement. • Adult onset Still’s disease – a form of arthritis characterized by high spiking fevers and a salmon- colored rash. Still’s disease is more common in children. • Caplan’s syndrome – an inflammation and scarring of the lungs in people with rheumatoid arthritis who have exposure to coal dust, as in a mine. • Celiac disease – an autoimmune disorder of the small intestine that causes malabsorption of nutrients and can eventually cause osteopenia or osteoporosis. • Dermatomyositis – a connective tissue disease characterized by inflammation of the muscles and the skin. The condition is believed to be caused either by viral infection or an autoimmune reaction. • Diabetic finger sclerosis – a complication of diabetes, causing a hardening of the skin and connective tissue in the fingers, thus causing stiffness. • Duchenne muscular dystrophy – one of the most prevalent types of muscular dystrophy, characterized by rapid muscle degeneration. • Dupuytren’s contracture – an abnormal thickening of tissues in the palm and fingers that can cause the fingers to curl. • Eosinophilic fasciitis (Shulman’s syndrome) – a condition in which the muscle tissue underneath the skin becomes swollen and thick. People with eosinophilic fasciitis have a buildup of eosinophils—a type of white blood cell—in the affected tissue. -

Plantar Fasciitis
Recent Advances in Orthotic Therapy for Plantar Fasciitis An Evidence Based Approach Lawrence Z. Huppin, D.P.M. Assistant Clinical Professor, Western University of Health Sciences, College of Podiatric Medicine Disclosures I disclose the following financial relationships with commercial entities that produce health care related products and services relevant to the content of this lecture: ◦ Employee (Medical Director) of ProLab Orthotics, manufacturer of foot orthoses Our Goals . Review Three Studies that Help Optimize Clinical Outcome of Custom Foot Orthoses Used to Treat Plantar Fasciitis • Cause of Plantar Fascial Tension • Forefoot Wedging Effect on Plantar Fascial Tension • Arch Contour Effect on Plantar Fascial Tension . Develop a “pathology specific” orthosis prescription to most effectively treat plantar fasciitis . Offloading Excessive Fascia Tension is Goal of Orthotic Therapy . What Causes Tension? Tissue Stress Theory McPoil, Hunt. Evaluation and Management of Foot and Ankle Disorders: Present Problems and Future Directions. Journal of Orthopaedic & Sports Physical Therapy, 1995 Effect of STJ Pronation on PF Strain . Cannot by itself cause strain of plantar fascia . Can only increase plantar fascia strain via the MTJ • (inversion of the forefoot on the rearfoot) Scherer. “Heel Pain Syndrome: Pathomechanics and Non-surgical Treatment. JAPMA 1991 Effect of Forefoot Inversion on Plantar Fascial Strain 73 patients with 118 painful heels 91% had foot deformity compensated by supination of long axis of MTJ Out of 118 painful heels 63 had forefoot valgus 33 had everted rearfoot 20 had plantarflexed first ray Scherer 1991 What foot types supinate the MTJ? . 47% forefoot valgus . 24% everted heel . 20% plantarflexed first ray Scherer 1991 What foot types supinate the MTJ? . -

Chronic Foot Pain
Revised 2020 American College of Radiology ACR Appropriateness Criteria® Chronic Foot Pain Variant 1: Chronic foot pain. Unknown etiology. Initial imaging. Procedure Appropriateness Category Relative Radiation Level Radiography foot Usually Appropriate ☢ US foot Usually Not Appropriate O MRI foot without and with IV contrast Usually Not Appropriate O MRI foot without IV contrast Usually Not Appropriate O CT foot with IV contrast Usually Not Appropriate ☢ CT foot without and with IV contrast Usually Not Appropriate ☢ CT foot without IV contrast Usually Not Appropriate ☢ Bone scan foot Usually Not Appropriate ☢☢☢ Variant 2: Persistent posttraumatic foot pain. Radiographs negative or equivocal. Clinical concern includes complex regional pain syndrome type I. Next imaging study. Procedure Appropriateness Category Relative Radiation Level MRI foot without IV contrast Usually Appropriate O 3-phase bone scan foot Usually Appropriate ☢☢☢ MRI foot without and with IV contrast May Be Appropriate O US foot Usually Not Appropriate O CT foot with IV contrast Usually Not Appropriate ☢ CT foot without and with IV contrast Usually Not Appropriate ☢ CT foot without IV contrast Usually Not Appropriate ☢ Variant 3: Chronic metatarsalgia including plantar great toe pain. Radiographs negative or equivocal. Clinical concern includes sesamoiditis, Morton’s neuroma, intermetatarsal bursitis, chronic plantar plate injury, or Freiberg’s infraction. Next imaging study. Procedure Appropriateness Category Relative Radiation Level MRI foot without IV contrast Usually Appropriate O US foot May Be Appropriate O MRI foot without and with IV contrast May Be Appropriate O CT foot without IV contrast May Be Appropriate ☢ Bone scan foot May Be Appropriate ☢☢☢ CT foot with IV contrast Usually Not Appropriate ☢ CT foot without and with IV contrast Usually Not Appropriate ☢ ACR Appropriateness Criteria® 1 Chronic Foot Pain Variant 4: Chronic plantar heel pain. -
Eosinophilic Fasciitis (Shulman Syndrome)
CONTINUING MEDICAL EDUCATION Eosinophilic Fasciitis (Shulman Syndrome) Sueli Carneiro, MD, PhD; Arles Brotas, MD; Fabrício Lamy, MD; Flávia Lisboa, MD; Eduardo Lago, MD; David Azulay, MD; Tulia Cuzzi, MD, PhD; Marcia Ramos-e-Silva, MD, PhD GOAL To understand eosinophilic fasciitis to better manage patients with the condition OBJECTIVES Upon completion of this activity, dermatologists and general practitioners should be able to: 1. Recognize the clinical presentation of eosinophilic fasciitis. 2. Discuss the histologic findings in patients with eosinophilic fasciitis. 3. Differentiate eosinophilic fasciitis from similarly presenting conditions. CME Test on page 215. This article has been peer reviewed and is accredited by the ACCME to provide continuing approved by Michael Fisher, MD, Professor of medical education for physicians. Medicine, Albert Einstein College of Medicine. Albert Einstein College of Medicine designates Review date: March 2005. this educational activity for a maximum of 1 This activity has been planned and implemented category 1 credit toward the AMA Physician’s in accordance with the Essential Areas and Policies Recognition Award. Each physician should of the Accreditation Council for Continuing Medical claim only that credit that he/she actually spent Education through the joint sponsorship of Albert in the activity. Einstein College of Medicine and Quadrant This activity has been planned and produced in HealthCom, Inc. Albert Einstein College of Medicine accordance with ACCME Essentials. Drs. Carneiro, Brotas, Lamy, Lisboa, Lago, Azulay, Cuzzi, and Ramos-e-Silva report no conflict of interest. The authors report no discussion of off-label use. Dr. Fisher reports no conflict of interest. We present a case of eosinophilic fasciitis, or Shulman syndrome apart from all other sclero- Shulman syndrome, in a 35-year-old man and dermiform states. -

Ruptured Popliteal Cyst Diagnosed by Ultrasound Before Evaluation for Deep Vein Thrombosis Joon Sung Kim, MD, Seong Hoon Lim, MD, Bo Young Hong, MD, So Young Park, MD
Case Report Ann Rehabil Med 2014;38(6):843-846 pISSN: 2234-0645 • eISSN: 2234-0653 http://dx.doi.org/10.5535/arm.2014.38.6.843 Annals of Rehabilitation Medicine Ruptured Popliteal Cyst Diagnosed by Ultrasound Before Evaluation for Deep Vein Thrombosis Joon Sung Kim, MD, Seong Hoon Lim, MD, Bo Young Hong, MD, So Young Park, MD Department of Rehabilitation Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea Most popliteal cysts are asymptomatic. However, cysts may rupture, resulting in pain and swelling of the leg that could also arise from other diseases, including deep vein thrombosis, lymphedema, cellulitis, and tear of a muscle or tendon. Therefore, it is difficult to diagnose a ruptured popliteal cyst based on only a patient’s history and physical examination. Musculoskeletal ultrasound has been regarded as a diagnostic tool for ruptured popliteal cyst. Here, we describe a patient who was rapidly diagnosed as ruptured popliteal cyst by ultrasonography. Therefore, ultrasound could be used to distinguish a ruptured popliteal cyst from other diseases in patients with painful swollen legs before evaluation for deep vein thrombosis. Keywords Calf pain, Complicated popliteal cyst, Ultrasonography INTRODUCTION or tendon (e.g., the medial head of the gastrocnemius [MHG] or Achilles tendon), neoplasm, and hemorrhage Popliteal cyst is a benign disease filled with fluid in the can cause similar symptoms. Some studies evaluated popliteal fossa. It occurs by distention of the semimem- nonspecific leg symptoms, such as swelling or pain, by branosus-gastrocnemius bursa communicating with the ultrasonography and ruptured popliteal cyst was easily knee joint [1]. -

Plantar Fasciitis Thomas Trojian, MD, MMB, and Alicia K
Plantar Fasciitis Thomas Trojian, MD, MMB, and Alicia K. Tucker, MD, Drexel University College of Medicine, Philadelphia, Pennsylvania Plantar fasciitis is a common problem that one in 10 people will experience in their lifetime. Plantar fasciopathy is an appro- priate descriptor because the condition is not inflammatory. Risk factors include limited ankle dorsiflexion, increased body mass index, and standing for prolonged periods of time. Plantar fasciitis is common in runners but can also affect sedentary people. With proper treatment, 80% of patients with plantar fasciitis improve within 12 months. Plantar fasciitis is predominantly a clinical diagnosis. Symp- toms are stabbing, nonradiating pain first thing in the morning in the proximal medioplantar surface of the foot; the pain becomes worse at the end of the day. Physical examination findings are often limited to tenderness to palpation of the proximal plantar fascial insertion at the anteromedial calcaneus. Ultrasonogra- phy is a reasonable and inexpensive diagnostic tool for patients with pain that persists beyond three months despite treatment. Treatment should start with stretching of the plantar fascia, ice massage, and nonsteroidal anti-inflamma- tory drugs. Many standard treatments such as night splints and orthoses have not shown benefit over placebo. Recalcitrant plantar fasciitis can be treated with injections, extracorporeal shock wave therapy, or surgical procedures, although evidence is lacking. Endoscopic fasciotomy may be required in patients who continue to have pain that limits activity and function despite exhausting nonoperative treatment options. (Am Fam Physician. 2019; 99(12):744-750. Copyright © 2019 American Academy of Family Physicians.) Illustration by Todd Buck Plantar fasciitis (also called plantar fasciopathy, reflect- than 27 kg per m2 (odds ratio = 3.7), and spending most ing the absence of inflammation) is a common problem of the workday on one’s feet 4,5 (Table 1 6). -

Calcium Pyrophosphate Dihydrate and Hydroxyapatite Crystals in a Patient with Rheumatoid Arthritis: a Case Report Shereen R
Case report 91 Calcium pyrophosphate dihydrate and hydroxyapatite crystals in a patient with rheumatoid arthritis: a case report Shereen R. Kamel Department of Rheumatology and The association between rheumatoid arthritis (RA) and calcium pyrophosphate Rehabilitation, Minia University, Egypt dihydrate (CPPD) crystal deposits can now be easily identified by MSUS, which is a Correspondence to Shereen R Kamel, MD, noninvasive technique that can be applied to patients with painful joints and Department of Rheumatology and enthesis that are unexplained by rheumatoid activity. In this paper, we report an Rehabilitation, Minia University, Minia 6111, Egyptian case of a 51-year-old man who had rheumatoid arthritis since 7 years and Egypt ’ Tel: +20 106 580 0025; developed bilateral knee and heel pain of 1.5 months duration with gradual onset e-mail: [email protected] and progressive course. Radiography revealed features of RA in both hands, as well as features of severe osteoarthritis in both knees with no signs of Received 2 October 2016 Accepted 7 February 2017 chondrocalcinosis. Ultrasonography of the joints, Achilles tendon, and plantar fascia detected knee, Achilles tendon, and plantar fascia calcifications, which Egyptian Rheumatology & Rehabilitation 2017, 44:91–94 are characteristic of CPPD, and supraspinatus calcification, which is characteristic of hydroxyapatite (HA) deposition. Further investigations revealed no evidence of metabolic disorders. CPPD and HA crystals were identified in his synovial fluid. Subclinical affection with CPPD and HA crystals in RA can be easily detected by ultrasonography, which allows early management to prevent future attacks in RA patients that could lead to exacerbation of joint symptoms that may be missed as rheumatoid disease activity. -

A Novel Treatment for Refractory Plantar Fasciitis
Orthopedic Technologies & Techniques A Novel Treatment for Refractory Plantar Fasciitis Mihir M. Patel, MD graphic imaging allow accurate localization of the pathologic Abstract process,1-3 and this localization in turn provides an oppor- Chronic plantar fasciitis is a major health care problem tunity to deliver a more reliable and focused intervention, worldwide and affects nearly 10% of the US popula- as in needle-guided therapy.4 Surgical procedures for plantar tion. Although most cases resolve with conservative fasciitis have included open or endoscopically assisted plantar care, the numerous treatments for refractory plantar fasciectomies with or without gastrocnemius recession; these fasciitis attest to the lack of consensus regarding these procedures have had varying results. The emerging goals for cases. The emerging goals for this condition are a mini- this condition are a minimally invasive percutaneous interven- mally invasive percutaneous intervention that is safe, tion that is safe, effective, and well-tolerated and has minimal effective, and well-tolerated and has minimal morbidity morbidity and a low complication rate. and a low complication rate. We conducted a prospective study in which patients were We conducted a prospective study in which pa- allowed either to continue with noninvasive treatment or to tients were allowed either to continue with noninvasive undergo focal aspiration and partial fasciotomy with an ul- treatment or to undergo focal aspiration and partial trasonic probe. Study inclusion criteria were plantar fasciitis fasciotomy with an ultrasonic probe. symptoms lasting 12 months or longer. Exclusion criteria were This is the first report of a plantar fascia partial re- unwillingness to participate in the study. -
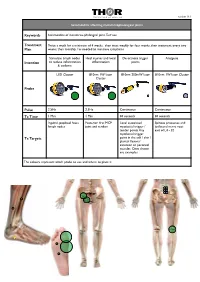
Sesamoiditis MTP Version 16.1.Pages
THOR logo 450 WIDE.pdf 26/9/07 22:55:23 C M Y CM MY CY CMY K version 16.1 Sesamoiditis affecting metatarsophalangeal joints Keywords Sesamoiditis of metatarso-phalangeal joint, Turf toe Treatment Twice a week for a minimum of 4 weeks, then treat weekly for four weeks, then treatment every two Plan weeks, then monthly / as needed to minimise symptoms Stimulate lymph nodes Heal injuries and local De-activate trigger Analgesia Intention to reduce inflammation inflammation points & oedema LED Cluster 810nm 1W laser 810nm 200mW laser 810nm 1W laser Cluster Cluster Probe Pulse 2.5Hz 2.5Hz Continuous Continuous Tx Time 1 Min 1 Min 30 seconds 30 seconds Inguinal, popliteal fossa Posterior first MCP Local associated Spinous processes and lymph nodes joint and tendon myofascial trigger / ipsilateral nerve root tender points Any exit of L4 - S2 myofascial trigger Tx Targets point in the calf / shin / plantar flexors/ extensor or peroneal muscles. Ones shown are examples The colours represent which probe to use and where to place it THOR logo 450 WIDE.pdf 26/9/07 22:55:23 C M Y CM MY CY CMY K Specific Evidence: A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Bjordal JM, Couppe C, Chow RT, Tuner J, Ljunggren EA Aust J Physiother 2003 49(2) 107-16 http://www.ncbi.nlm.nih.gov/entrez/query.fcgi? cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12775206 General evidence across disease category: Inflammation - tendons, fascia, soft tissue injuries Kiritsi O, Tsitas K, Malliaropoulos N, Mikroulis G.