Pulmonary Hypertension a Rare but Important Cause of Dyspnoea
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Oxygen and Oxygen Equipment Local Coverage Determination (LCD)
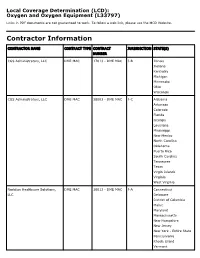
Local Coverage Determination (LCD): Oxygen and Oxygen Equipment (L33797) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER CGS Administrators, LLC DME MAC 17013 - DME MAC J-B Illinois Indiana Kentucky Michigan Minnesota Ohio Wisconsin CGS Administrators, LLC DME MAC 18003 - DME MAC J-C Alabama Arkansas Colorado Florida Georgia Louisiana Mississippi New Mexico North Carolina Oklahoma Puerto Rico South Carolina Tennessee Texas Virgin Islands Virginia West Virginia Noridian Healthcare Solutions, DME MAC 16013 - DME MAC J-A Connecticut LLC Delaware District of Columbia Maine Maryland Massachusetts New Hampshire New Jersey New York - Entire State Pennsylvania Rhode Island Vermont CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, DME MAC 19003 - DME MAC J-D Alaska LLC American Samoa Arizona California - Entire State Guam Hawaii Idaho Iowa Kansas Missouri - Entire State Montana Nebraska Nevada North Dakota Northern Mariana Islands Oregon South Dakota Utah Washington Wyoming LCD Information Document Information LCD ID Original Effective Date L33797 For services performed on or after 10/01/2015 LCD Title Revision Effective Date Oxygen and Oxygen Equipment For services performed on or after 08/02/2020 Proposed LCD in Comment Period Revision Ending Date N/A N/A Source Proposed LCD Retirement Date DL33797 N/A AMA CPT / ADA CDT / AHA NUBC Copyright Notice Period Start Date Statement 06/18/2020 CPT codes, descriptions and other data only are copyright 2019 American Medical Association. All Rights Notice Period End Date Reserved. -

Chronic Cough, Shortness of Breathe, Wheezing? What You Should
CHRONIC COUGH, SHORTNESS OF BREATH, WHEEZING? WHAT YOU SHOULD KNOW ABOUT COPD. A quick guide on Chronic Obstructive Pulmonary Disease COPD.nhlbi.nih.gov COPD, or chronic obstructive Most often, COPD occurs in people pulmonary disease, is a serious lung age 40 and over who… disease that over time makes it hard • Have a history of smoking to breathe. Other names for COPD include • Have had long-term exposure to lung irritants chronic bronchitis or emphysema. such as air pollution, chemical fumes, or dust from the environment or workplace COPD, a leading cause of death, • Have a rare genetic condition called alpha-1 affects millions of Americans and causes antitrypsin (AAT) deficiency long-term disability. • Have a combination of any of the above MAJOR COPD RISK FACTORS history of SMOKING AGE 40+ RARE GENETIC CONDITION alpha-1 antitrypsin (AAT) deficiency LONG-TERM exposure to lung irritants WHAT IS COPD? To understand what COPD is, we first The airways and air sacs are elastic (stretchy). need to understand how respiration When breathing in, each air sac fills up with air like and the lungs work: a small balloon. When breathing out, the air sacs deflate and the air goes out. When air is breathed in, it goes down the windpipe into tubes in the lungs called bronchial In COPD, less air flows in and out of tubes or airways. Within the lungs, bronchial the airways because of one or more tubes branch into thousands of smaller, thinner of the following: tubes called bronchioles. These tubes end in • The airways and air sacs lose bunches of tiny round air sacs called alveoli. -

Guía Práctica Clínica Bronquiolitis.Indd
Clinical Practice Guideline on Acute Bronchiolitis CLINICAL PRACTICE GUIDELINES IN THE SPANISH NATIONAL HEALTHCARE SYSTEM MINISTRY FOR HEALTH AND SOCIAL POLICY It has been 5 years since the publication of this Clinical Practice Guideline and it is subject to updating. Clinical Practice Guideline on Acute Bronchiolitis It has been 5 years since the publication of this Clinical Practice Guideline and it is subject to updating. CLINICAL PRACTICE GUIDELINES IN THE SPANISH NATIONAL HEALTHCARE SYSTEM MINISTRY FOR HEALTH AND SOCIAL POLICY This CPG is an aid for healthcare decisions. It is not binding, and does not replace the clinical judgement of healthcare staff. Published: 2010 It has beenPublished 5 years by: Ministry since for theScience publication and Innovation of this Clinical Practice Guideline and it is subject to updating. NIPO (Official Publication Identification No.): 477-09-055-4 ISBN: pending Legal depository: B-10297-2010 Printed by: Migraf Digital This CPG has been funded via an agreement entered into by the Carlos III Health Institute, an autonomous body within the Spanish Ministry for Science and Innovation, and the Catalan Agency for Health Technology Assessment, within the framework for cooperation established in the Quality Plan for the Spanish National Healthcare System of the Spanish Ministry for Health and Social Policy. This guideline must be cited: Working Group of the Clinical Practice Guideline on Acute Bronchiolitis; Sant Joan de Déu Foundation Fundació Sant Joan de Déu, coordinator; Clinical Practice Guideline on Acute Bronchiolitis; Quality Plan for the Spanish National Healthcare System of the Spanish Ministry for Health and Social Policy; Catalan Agency for Health Technology Assessment, 2010; Clinical Practice Guidelines in the Spanish National Healthcare System: CAHTA no. -

Management of Airway Obstruction and Stridor in Pediatric Patients
November 2017 Management of Airway Volume 14, Number 11 Obstruction and Stridor in Authors Ashley Marchese, MD Department of Pediatrics, Yale-New Haven Hospital, New Haven, CT Pediatric Patients Melissa L. Langhan, MD, MHS Associate Professor of Pediatrics and Emergency Medicine; Fellowship Director, Director of Education, Pediatric Emergency Abstract Medicine, Yale University School of Medicine, New Haven, CT Peer Reviewers Stridor is a result of turbulent air-flow through the trachea from Steven S. Bin, MD upper airway obstruction, and although in children it is often Associate Clinical Professor of Emergency Medicine and Pediatrics; Medical Director, Emergency Department, UCSF School of Medicine, due to croup, it can also be caused by noninfectious and/or con- Benioff Children’s Hospital, San Francisco, CA genital conditions as well as life-threatening etiologies. The his- Alexander Toledo, DO, PharmD, FAAEM, FAAP tory and physical examination guide initial management, which Chief, Section of Pediatric Emergency Medicine; Director, Pediatric Emergency Department, Arizona Children’s Center at Maricopa includes reduction of airway inflammation, treatment of bacterial Medical Center, Phoenix, AZ infection, and, less often, imaging, emergent airway stabilization, Prior to beginning this activity, see “Physician CME Information” or surgical management. This issue discusses the most common on the back page. as well as the life-threatening etiologies of acute and chronic stridor and its management in the emergency department. Editor-in-Chief -

Prilocaine Induced Methemoglobinemia Güzelliğin Bedeli; Prilokaine Bağlı Gelişen Methemoglobinemi Olgusu
CASE REPORT 185 Cost of Beauty; Prilocaine Induced Methemoglobinemia Güzelliğin Bedeli; Prilokaine Bağlı Gelişen Methemoglobinemi Olgusu Elif KILICLI, Gokhan AKSEL, Betul AKBUGA OZEL, Cemil KAVALCI, Dilek SUVEREN ARTUK Department of Emergency Medicine, Baskent University Faculty of Medicine, Ankara SUMMARY ÖZET Prilocaine induced methemoglobinemia is a rare entity. In the pres- Prilokaine bağlı gelişen methemoglobinemi nadir görülen bir du- ent paper, the authors aim to draw attention to the importance of rumdur. Bu yazıda epilasyon öncesi kullanılan prilokaine sekonder this rare condition by reporting this case. A 30-year-old female gelişen methemoglobinemi olgusunu sunarak nadir görülen bu presented to Emergency Department with headache, dispnea and durumun önemine işaret etmek istiyoruz. Otuz yaşında kadın acil cyanosis. The patient has a history of 1000-1200 mg of prilocaine servise baş ağrısı, dispne ve siyanoz şikayetleri ile başvurdu. Hasta- ya beş saat öncesinde bir güzellik merkezinde epilasyon öncesinde subcutaneous injection for hair removal at a beauty center, 5 hours yaklaşık 1000-1200 mg prilokain subkutan enjeksiyonu yapıldığı ago. Tension arterial: 130/73 mmHg, pulse: 103/minute, body tem- öğrenildi. Başvuruda kan basıncı 130/73 mmHg, nabız 103/dk, vü- perature: 37 °C and respiratory rate: 20/minute. The patient had ac- cut ısısı 37 °C ve solunum sayısı 20/dk olarak kaydedilmişti. Hasta- ral and perioral cyanosis. Methemoglobin was measured 14.1% in nın akral siyanozu belirgindi. Venöz kan gazında methemoglobin venous blood gas test. The patient treated with 3 gr ascorbic acid düzeyi %14.1 olarak ölçüldü. Hastaya 3 g intravenöz askorbik asit intravenously. The patient was discharged free of symptoms after uygulandı. -

Shanti Bhavan Medical Center Biru, Jharkhand, India
Shanti Bhavan Medical Center Biru, Jharkhand, India We Care, He Heals Urgent Needs 1. Boundary Wall around the hospital property Cost: $850,000 In India any land (even owned) can be taken by the government at any time if there is not boundary wall around it. Our organization owns property around the hospital that is intended for the Nursing school and other projects. We need a boundary wall built around the land so that the government can’t recover the land. 2. Magnetic Resonance Imaging Device Cost: $300,000 Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body in both health and disease. MRI scanners use strong magnetic fields, radio waves, and field gradients to generate images of the organs in the body. 3. Kidney Stone Lipotriptor Cost: $200,000 Kidney Stone Lipotriptor Extracorporeal Shock Wave Lithotripsy (ESWL) is the least invasive surgical stone treatment using high frequency sound waves from an external source (outside the body) to break up kidney stones into smaller pieces, and allow them to pass out through the urinary tract. 4. Central Patient Monitoring System Cost: $28,000 Central Patient Monitoring System- A full-featured system that provides comprehensive patient monitoring and review. Monitors up to 32 patients using two displays and is ideal for telemetry, critical care, OR, emergency room, and other monitoring environments. Provides data storage and review capabilities, and ensures a complete patient record by facilitating automated patient and data transfer between multiple departments. 5. ABG Machine Cost: $25,000 ABG machine- An arterial blood gas test (ABG) is a blood gas test of blood taken from an artery that measures the amounts of certain gases (such as oxygen and carbon diox- ide) dissolved in arterial blood. -

How Is Pulmonary Fibrosis Diagnosed?
How Is Pulmonary Fibrosis Diagnosed? Pulmonary fibrosis (PF) may be difficult to diagnose as the symptoms of PF are similar to other lung diseases. There are many different types of PF. If your doctor suspects you might have PF, it is important to see a specialist to confirm your diagnosis. This will help ensure you are treated for the exact disease you have. Health History and Exam Your doctor will perform a physical exam and listen to your lungs. • If your doctor hears a crackling sound when listening to your lungs, that is a sign you might have PF. • It is also important for your doctor to gather detailed information about your health. ⚪ This includes any family history of lung disease, any hazardous materials you may have been exposed to in your lifetime and any diseases you’ve been treated for in the past. Imaging Tests Tests like chest X-rays and CT scans can help your doctor look at your lungs to see if there is any scarring. • Many people with PF actually have normal chest X-rays in the early stages of the disease. • A high-resolution computed tomography scan, or HRCT scan, is an X-ray that provides sharper and more detailed pictures than a standard chest X-ray and is an important component of diagnosing PF. • Your doctor may also perform an echocardiogram (ECHO). ⚪ This test uses sound waves to look at your heart function. ⚪ Doctors use this test to detect pulmonary hypertension, a condition that can accompany PF, or abnormal heart function. Lung Function Tests There are several ways to test how well your lungs are working. -

Obesity and Its Respiratory Effects Detected Through Levels of Partial Pressure of Carbon Dioxide in the Supine Position
Gaceta Médica de México. 2016;152 Contents available at PubMed www.anmm.org.mx PERMANYER Gac Med Mex. 2016;152:542-8 www.permanyer.com GACETA MÉDICA DE MÉXICO ORIGINAL ARTICLE Obesity and its respiratory effects detected through levels of partial pressure of carbon dioxide in the supine position América Sánchez-Medina1*, Marcela Ma. Sánchez-Medina2, María Dolores Ochoa Vázquez3, Simón Barquera Cervera1 and Luis Gerardo Ochoa Jiménez1 1Pulmonology Department, Centro Médico Nacional La Raza, IMSS, Morelia, Mich., Mexico; 2Health Science, 3Jefe del servicio de Neumología, Centro Médico Nacional La Raza, IMSS, Morelia, Mich., Mexico Abstract Introduction: Obesity is a disease that is closely associated with deleterious respiratory effects such as the Obesity Hy- poventilation Syndrome which conventionally includes awake hypercapnia. There are studies addressing the detection of daytime hypercapnia with the patient either in sitting or standing position. However, there are no studies in obese subjects with a normal daytime PaCO2 in whom the detection of hypercapnia is made in the supine position. It is feasible that the physiopathological changes that occur in obese patients when they adopt the supine position lead to increased PaCO2 levels or hypercapnia. Objective: To determine the levels of PaCO2 in obese patients with a normal daytime PaCO2 in the supine position using arterial blood gas test. Methods: Fifty patients with BMI > 30 Kg/m², with a normal daytime PaCO2 were included. Daytime arterial blood gas test was performed first with the patient in a standing position along with pulmonary function test. A second arterial blood gas test was made 15 minutes after the patient adopted the supine position. -

Virtual Autopsy in Legal Medicine: Literature Review and Example of Application on the Mummified Remains
MEDICINE, LAW & SOCIETY Vol. 11, No. 2, pp. 67-90 , October 2018 Virtual Autopsy in Legal Medicine: Literature Review and Example of Application on the Mummified Remains IVANA KRUŽIĆ, IVAN JERKOVIĆ, FRANE MIHANOVIĆ, ANA MARUŠIĆ, ŠIMUN ANĐELINOVIĆ & ŽELJANA BAŠIĆ Abstract The virtual autopsy and post-mortem imaging methods are relatively novel methods used in medicine to determine cause and manner of death. They can also be exceptionally useful in the process of identification. Although they have numerous advantages, they are still not implemented in practice to a sufficient extent because the methodology has not yet been validated, and studies that deal with legal and practical implications of those methods are relatively scarce. In this article we describe basic principles and advantages of the methodology, explore related legal and practical issues, and present a case of virtual autopsy in practice on the mummified remains of St. Ivan Olini from Church of St. Blaise in Vodnjan (Croatia). Keywords: • Virtual Examination • Autopsy • MSCT • Paleopathology • Mummy • Sacral Remains • CORRESPONDENCE ADDRESS: . Ivan Jerković, ML, University of Split, University Department of Forensic Sciences, Ruđera Boškovića 33, 21000 Split, Croatia, e-mail: [email protected]. Ivana Kružić, PhD, Assistant Professor, University of Split, University Department of Forensic Sciences, Ruđera Boškovića 33, 21000 Split, Croatia, e-mail: [email protected]. Frane Mihanović, PhD, Assistant Professor, University of Split, University Department of Health Studies, Ruđera Boškovića 33, 21000 Split, Croatia, e-mail: [email protected]. Ana Marušić, PhD, Full Professor, University of Split, Split School of Medicine, Department of Research in Bioimedicine and Health, Šoltanska 2, 21000 Split, Croatia, e-mail: [email protected]. -

Chapter 6: Clinical Presentation of Venous Thrombosis “Clots”
CHAPTER 6 CLINICAL PRESENTATION OF VENOUS THROMBOSIS “CLOTS”: DEEP VENOUS THROMBOSIS AND PULMONARY EMBOLUS Original authors: Daniel Kim, Kellie Krallman, Joan Lohr, and Mark H. Meissner Abstracted by Kellie R. Brown Introduction The body has normal processes that balance between clot formation and clot breakdown. This allows clot to form when necessary to stop bleeding, but allows the clot formation to be limited to the injured area. Unbalancing these systems can lead to abnormal clot formation. When this happens clot can form in the deep veins usually, but not always, in the legs, forming a deep vein thrombosis (DVT). In some cases, this clot can dislodge from the vein in which it was formed and travel through the bloodstream into the lungs, where it gets stuck as the size of the vessels get too small to allow the clot to go any further. This is called a pulmonary embolus (PE). This limits the amount of blood that can get oxygen from the lungs, which then limits the amount of oxygen that can be delivered to the rest of the body. How severe the PE is for the patient has to do with the size of the clot that gets to the lungs. Small clots can cause no symptoms at all. Very large clots can cause death very quickly. This chapter will describe the symptoms that are caused by DVT and PE, and discuss the means by which these conditions are diagnosed. What are the most common signs and symptoms of a DVT? The symptoms that are caused by DVT depend on the location and extent of the clot. -

Clinical Utility of Arterial Blood Gas Test in an Intensive Care Unit: an Observational Study Jagadish Chandran1 , Carol D’Silva2 , Sampath Sriram3 , Bhuvana Krishna4
ORIGINAL ARTICLE Clinical Utility of Arterial Blood Gas Test in an Intensive Care Unit: An Observational Study Jagadish Chandran1 , Carol D’Silva2 , Sampath Sriram3 , Bhuvana Krishna4 ABSTRACT Background: Arterial blood gas (ABG) analysis is a common test ordered in critically ill patients. Often, it is performed very frequently without influencing patient care. Hence, we decided to check the utility of the ABG test in our intensive care unit (ICU). Materials and methods: The data of the previous day ABGs were captured by reviewing the chart in an online pro forma which was filled by the authors. Data relating to patient’s details, who ordered ABGs, reason for ordering ABGs, and did the ABG influence patient’s management were entered. A total of 985 ABGs were performed in 173 patients for 2 months which was analyzed. Results: Out of 985 ABGs, in 259 instances (26.29%), interventions were done after reviewing an ABG. The major interventions among these ABGs were ventilator settings adjustment in 134 ABGs (13.6%). A total of 790 ABGs were done routinely with no specific indication (80.20%), while doctors ordered one following an event for 195 ABGs (19.80%). Conclusion: Our data suggest that 80% of ABG tests were ordered as part of a routine test. Keywords: Arterial blood gas, Arterial cannula, Clinical utility. Indian Journal of Critical Care Medicine (2021): 10.5005/jp-journals-10071-23719 INTRODUCTION 1–4Department of Critical Care Medicine, St. John’s Medical College and Arterial blood gas (ABG) analysis is one of the most common tests Hospital, Bengaluru, Karnataka, India ordered in the ICU. -

Virtual Autopsy Using Imaging: Bridging Radiologic And
Eur Radiol (2008) 18: 273–282 DOI 10.1007/s00330-007-0737-4 FORENSIC MEDICINE Stephan A. Bolliger Virtual autopsy using imaging: bridging Michael J. Thali Steffen Ross radiologic and forensic sciences. A review Ursula Buck Silvio Naether of the Virtopsy and similar projects Peter Vock Abstract The transdisciplinary re- addition, is also well suited to the Received: 26 March 2007 Revised: 25 June 2007 search project Virtopsy is dedicated to examination of surviving victims of Accepted: 16 July 2007 implementing modern imaging tech- assault, especially choking, and helps Published online: 18 August 2007 niques into forensic medicine and visualise internal injuries not seen at # Springer-Verlag 2007 pathology in order to augment current external examination of the victim. examination techniques or even to Apart from the accuracy and three- offer alternative methods. Our dimensionality that conventional project relies on three pillars: three- documentations lack, these techniques dimensional (3D) surface scanning for allow for the re-examination of the . S. A. Bolliger (*) M. J. Thali the documentation of body surfaces, corpse and the crime scene even S. Ross . U. Buck . S. Naether Centre for Forensic Imaging and and both multislice computed tomog- decades later, after burial of the corpse Virtopsy, Institute of Forensic raphy (MSCT) and magnetic reso- and liberation of the crime scene. We Medicine, University of Bern, nance imaging (MRI) to visualise the believe that this virtual, non-invasive Buehlstrasse 20, internal body. Three-dimensional or minimally invasive approach will 3012 Bern, Switzerland e-mail: [email protected] surface scanning has delivered re- improve forensic medicine in the Tel.: +41-31-6318411 markable results in the past in the 3D near future.