Navigating Pulmonary Fibrosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
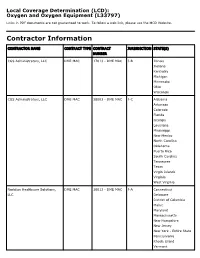
Oxygen and Oxygen Equipment Local Coverage Determination (LCD)
Local Coverage Determination (LCD): Oxygen and Oxygen Equipment (L33797) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER CGS Administrators, LLC DME MAC 17013 - DME MAC J-B Illinois Indiana Kentucky Michigan Minnesota Ohio Wisconsin CGS Administrators, LLC DME MAC 18003 - DME MAC J-C Alabama Arkansas Colorado Florida Georgia Louisiana Mississippi New Mexico North Carolina Oklahoma Puerto Rico South Carolina Tennessee Texas Virgin Islands Virginia West Virginia Noridian Healthcare Solutions, DME MAC 16013 - DME MAC J-A Connecticut LLC Delaware District of Columbia Maine Maryland Massachusetts New Hampshire New Jersey New York - Entire State Pennsylvania Rhode Island Vermont CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, DME MAC 19003 - DME MAC J-D Alaska LLC American Samoa Arizona California - Entire State Guam Hawaii Idaho Iowa Kansas Missouri - Entire State Montana Nebraska Nevada North Dakota Northern Mariana Islands Oregon South Dakota Utah Washington Wyoming LCD Information Document Information LCD ID Original Effective Date L33797 For services performed on or after 10/01/2015 LCD Title Revision Effective Date Oxygen and Oxygen Equipment For services performed on or after 08/02/2020 Proposed LCD in Comment Period Revision Ending Date N/A N/A Source Proposed LCD Retirement Date DL33797 N/A AMA CPT / ADA CDT / AHA NUBC Copyright Notice Period Start Date Statement 06/18/2020 CPT codes, descriptions and other data only are copyright 2019 American Medical Association. All Rights Notice Period End Date Reserved. -

Chronic Cough, Shortness of Breathe, Wheezing? What You Should
CHRONIC COUGH, SHORTNESS OF BREATH, WHEEZING? WHAT YOU SHOULD KNOW ABOUT COPD. A quick guide on Chronic Obstructive Pulmonary Disease COPD.nhlbi.nih.gov COPD, or chronic obstructive Most often, COPD occurs in people pulmonary disease, is a serious lung age 40 and over who… disease that over time makes it hard • Have a history of smoking to breathe. Other names for COPD include • Have had long-term exposure to lung irritants chronic bronchitis or emphysema. such as air pollution, chemical fumes, or dust from the environment or workplace COPD, a leading cause of death, • Have a rare genetic condition called alpha-1 affects millions of Americans and causes antitrypsin (AAT) deficiency long-term disability. • Have a combination of any of the above MAJOR COPD RISK FACTORS history of SMOKING AGE 40+ RARE GENETIC CONDITION alpha-1 antitrypsin (AAT) deficiency LONG-TERM exposure to lung irritants WHAT IS COPD? To understand what COPD is, we first The airways and air sacs are elastic (stretchy). need to understand how respiration When breathing in, each air sac fills up with air like and the lungs work: a small balloon. When breathing out, the air sacs deflate and the air goes out. When air is breathed in, it goes down the windpipe into tubes in the lungs called bronchial In COPD, less air flows in and out of tubes or airways. Within the lungs, bronchial the airways because of one or more tubes branch into thousands of smaller, thinner of the following: tubes called bronchioles. These tubes end in • The airways and air sacs lose bunches of tiny round air sacs called alveoli. -

Guía Práctica Clínica Bronquiolitis.Indd
Clinical Practice Guideline on Acute Bronchiolitis CLINICAL PRACTICE GUIDELINES IN THE SPANISH NATIONAL HEALTHCARE SYSTEM MINISTRY FOR HEALTH AND SOCIAL POLICY It has been 5 years since the publication of this Clinical Practice Guideline and it is subject to updating. Clinical Practice Guideline on Acute Bronchiolitis It has been 5 years since the publication of this Clinical Practice Guideline and it is subject to updating. CLINICAL PRACTICE GUIDELINES IN THE SPANISH NATIONAL HEALTHCARE SYSTEM MINISTRY FOR HEALTH AND SOCIAL POLICY This CPG is an aid for healthcare decisions. It is not binding, and does not replace the clinical judgement of healthcare staff. Published: 2010 It has beenPublished 5 years by: Ministry since for theScience publication and Innovation of this Clinical Practice Guideline and it is subject to updating. NIPO (Official Publication Identification No.): 477-09-055-4 ISBN: pending Legal depository: B-10297-2010 Printed by: Migraf Digital This CPG has been funded via an agreement entered into by the Carlos III Health Institute, an autonomous body within the Spanish Ministry for Science and Innovation, and the Catalan Agency for Health Technology Assessment, within the framework for cooperation established in the Quality Plan for the Spanish National Healthcare System of the Spanish Ministry for Health and Social Policy. This guideline must be cited: Working Group of the Clinical Practice Guideline on Acute Bronchiolitis; Sant Joan de Déu Foundation Fundació Sant Joan de Déu, coordinator; Clinical Practice Guideline on Acute Bronchiolitis; Quality Plan for the Spanish National Healthcare System of the Spanish Ministry for Health and Social Policy; Catalan Agency for Health Technology Assessment, 2010; Clinical Practice Guidelines in the Spanish National Healthcare System: CAHTA no. -

Bronchiolitis After Lung Transplantation Lymphoid Tissue In
The Role of Intrapulmonary De Novo Lymphoid Tissue in Obliterative Bronchiolitis after Lung Transplantation This information is current as Masaaki Sato, Shin Hirayama, David M. Hwang, Humberto of September 25, 2021. Lara-Guerra, Dirk Wagnetz, Thomas K. Waddell, Mingyao Liu and Shaf Keshavjee J Immunol 2009; 182:7307-7316; ; doi: 10.4049/jimmunol.0803606 http://www.jimmunol.org/content/182/11/7307 Downloaded from References This article cites 46 articles, 4 of which you can access for free at: http://www.jimmunol.org/content/182/11/7307.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 25, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2009 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology The Role of Intrapulmonary De Novo Lymphoid Tissue in Obliterative Bronchiolitis after Lung Transplantation1 Masaaki Sato,* Shin Hirayama,* David M. Hwang,*† Humberto Lara-Guerra,* Dirk Wagnetz,* Thomas K. Waddell,* Mingyao Liu,* and Shaf Keshavjee2* Chronic rejection after lung transplantation is manifested as obliterative bronchiolitis (OB). -

Management of Airway Obstruction and Stridor in Pediatric Patients
November 2017 Management of Airway Volume 14, Number 11 Obstruction and Stridor in Authors Ashley Marchese, MD Department of Pediatrics, Yale-New Haven Hospital, New Haven, CT Pediatric Patients Melissa L. Langhan, MD, MHS Associate Professor of Pediatrics and Emergency Medicine; Fellowship Director, Director of Education, Pediatric Emergency Abstract Medicine, Yale University School of Medicine, New Haven, CT Peer Reviewers Stridor is a result of turbulent air-flow through the trachea from Steven S. Bin, MD upper airway obstruction, and although in children it is often Associate Clinical Professor of Emergency Medicine and Pediatrics; Medical Director, Emergency Department, UCSF School of Medicine, due to croup, it can also be caused by noninfectious and/or con- Benioff Children’s Hospital, San Francisco, CA genital conditions as well as life-threatening etiologies. The his- Alexander Toledo, DO, PharmD, FAAEM, FAAP tory and physical examination guide initial management, which Chief, Section of Pediatric Emergency Medicine; Director, Pediatric Emergency Department, Arizona Children’s Center at Maricopa includes reduction of airway inflammation, treatment of bacterial Medical Center, Phoenix, AZ infection, and, less often, imaging, emergent airway stabilization, Prior to beginning this activity, see “Physician CME Information” or surgical management. This issue discusses the most common on the back page. as well as the life-threatening etiologies of acute and chronic stridor and its management in the emergency department. Editor-in-Chief -

06. Baransel Saygi
Turkish Journal of Trauma & Emergency Surgery Ulus Travma Acil Cerrahi Derg 2008;14(2):103-109 The effect of dehydration and irrigation on the healing of Achilles tendon: an experimental study Dehidrasyon (kuruluk) ve irigasyonun (y›kama) Aflil tendon iyileflmesi üzerine etkileri: Deneysel çalıflma Baransel SA Y G I,1 Yakup YI L D I R I M,2 Cengiz ÇA B U K O ⁄ L U,3 Hasan KA R A,3 Saime Sezgin RA M A D A N,4 Tanıl ES E M E N L ‹ 5 BACKGROUND AMAÇ Air exposure is a factor that inhibits in vitro cellular prolifer- Hava teması tendonlarda canl›-d›fl› (in vitro) ortamda matriks ation and matrix synthesis in tendons. Aim of this experimen- sentezini ve hücre ilerlemesini azaltabilir ve hatta önleyebilir. tal study was to evaluate effect of dehydration and irrigation Bu çalıflmanın amacı, dehidrasyon ve irigasyonun Aflil tendon on healing of Achilles tendon. iyileflmesi üzerine etkisinin canl›-içi (in vivo) hayvan modeli METHODS üzerinde gösterilmesidir. Achilles tenotomy was done in forty-five Sprague-Dawley GEREÇ VE YÖNTEM rats. In control group, tendon was sutured immediately. In the K›rk befl adet Sprague-Dawley cinsi s›çan›n Aflil tenotomisi remaining two groups, the Achilles tendons were allowed to yapıldı. Kontrol grubunda, tendon hemen dikildi. Di¤er iki direct exposure of air. Irrigation of Achilles tendon was per- grubun cilt ve cilt altı dokuları ekarte edilerek Aflil tendon- formed in one of exposed groups, while irrigation was not larının do¤rudan hava ile teması sa¤landı. Bu gruplardan biri- done in other group. -

Endotrophin Triggers Adipose Tissue Fibrosis and Metabolic Dysfunction
ARTICLE Received 12 Sep 2013 | Accepted 21 Feb 2014 | Published 19 Mar 2014 DOI: 10.1038/ncomms4485 Endotrophin triggers adipose tissue fibrosis and metabolic dysfunction Kai Sun1,*, Jiyoung Park1,2,*, Olga T. Gupta1, William L. Holland1, Pernille Auerbach3, Ningyan Zhang4, Roberta Goncalves Marangoni5, Sarah M. Nicoloro6, Michael P. Czech6, John Varga5, Thorkil Ploug3, Zhiqiang An4 & Philipp E. Scherer1,7 We recently identified endotrophin as an adipokine with potent tumour-promoting effects. However, the direct effects of local accumulation of endotrophin in adipose tissue have not yet been studied. Here we use a doxycycline-inducible adipocyte-specific endotrophin overexpression model to demonstrate that endotrophin plays a pivotal role in shaping a metabolically unfavourable microenvironment in adipose tissue during consumption of a high-fat diet (HFD). Endotrophin serves as a powerful co-stimulator of pathologically relevant pathways within the ‘unhealthy’ adipose tissue milieu, triggering fibrosis and inflammation and ultimately leading to enhanced insulin resistance. We further demonstrate that blocking endotrophin with a neutralizing antibody ameliorates metabolically adverse effects and effectively reverses metabolic dysfunction induced during HFD exposure. Collectively, our findings demonstrate that endotrophin exerts a major influence in adipose tissue, eventually resulting in systemic elevation of pro-inflammatory cytokines and insulin resistance, and the results establish endotrophin as a potential target in the context of metabolism and cancer. 1 Touchstone Diabetes Center, Department of Internal Medicine, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, Texas 75390, USA. 2 Department of Biological Sciences, School of Life Sciences, Ulsan National Institute of Science and Technology, 50 UNIST street, Ulsan 689-798, Korea. -

Prilocaine Induced Methemoglobinemia Güzelliğin Bedeli; Prilokaine Bağlı Gelişen Methemoglobinemi Olgusu
CASE REPORT 185 Cost of Beauty; Prilocaine Induced Methemoglobinemia Güzelliğin Bedeli; Prilokaine Bağlı Gelişen Methemoglobinemi Olgusu Elif KILICLI, Gokhan AKSEL, Betul AKBUGA OZEL, Cemil KAVALCI, Dilek SUVEREN ARTUK Department of Emergency Medicine, Baskent University Faculty of Medicine, Ankara SUMMARY ÖZET Prilocaine induced methemoglobinemia is a rare entity. In the pres- Prilokaine bağlı gelişen methemoglobinemi nadir görülen bir du- ent paper, the authors aim to draw attention to the importance of rumdur. Bu yazıda epilasyon öncesi kullanılan prilokaine sekonder this rare condition by reporting this case. A 30-year-old female gelişen methemoglobinemi olgusunu sunarak nadir görülen bu presented to Emergency Department with headache, dispnea and durumun önemine işaret etmek istiyoruz. Otuz yaşında kadın acil cyanosis. The patient has a history of 1000-1200 mg of prilocaine servise baş ağrısı, dispne ve siyanoz şikayetleri ile başvurdu. Hasta- ya beş saat öncesinde bir güzellik merkezinde epilasyon öncesinde subcutaneous injection for hair removal at a beauty center, 5 hours yaklaşık 1000-1200 mg prilokain subkutan enjeksiyonu yapıldığı ago. Tension arterial: 130/73 mmHg, pulse: 103/minute, body tem- öğrenildi. Başvuruda kan basıncı 130/73 mmHg, nabız 103/dk, vü- perature: 37 °C and respiratory rate: 20/minute. The patient had ac- cut ısısı 37 °C ve solunum sayısı 20/dk olarak kaydedilmişti. Hasta- ral and perioral cyanosis. Methemoglobin was measured 14.1% in nın akral siyanozu belirgindi. Venöz kan gazında methemoglobin venous blood gas test. The patient treated with 3 gr ascorbic acid düzeyi %14.1 olarak ölçüldü. Hastaya 3 g intravenöz askorbik asit intravenously. The patient was discharged free of symptoms after uygulandı. -

Shanti Bhavan Medical Center Biru, Jharkhand, India
Shanti Bhavan Medical Center Biru, Jharkhand, India We Care, He Heals Urgent Needs 1. Boundary Wall around the hospital property Cost: $850,000 In India any land (even owned) can be taken by the government at any time if there is not boundary wall around it. Our organization owns property around the hospital that is intended for the Nursing school and other projects. We need a boundary wall built around the land so that the government can’t recover the land. 2. Magnetic Resonance Imaging Device Cost: $300,000 Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body in both health and disease. MRI scanners use strong magnetic fields, radio waves, and field gradients to generate images of the organs in the body. 3. Kidney Stone Lipotriptor Cost: $200,000 Kidney Stone Lipotriptor Extracorporeal Shock Wave Lithotripsy (ESWL) is the least invasive surgical stone treatment using high frequency sound waves from an external source (outside the body) to break up kidney stones into smaller pieces, and allow them to pass out through the urinary tract. 4. Central Patient Monitoring System Cost: $28,000 Central Patient Monitoring System- A full-featured system that provides comprehensive patient monitoring and review. Monitors up to 32 patients using two displays and is ideal for telemetry, critical care, OR, emergency room, and other monitoring environments. Provides data storage and review capabilities, and ensures a complete patient record by facilitating automated patient and data transfer between multiple departments. 5. ABG Machine Cost: $25,000 ABG machine- An arterial blood gas test (ABG) is a blood gas test of blood taken from an artery that measures the amounts of certain gases (such as oxygen and carbon diox- ide) dissolved in arterial blood. -

Fibrosis in Human Adipose Tissue
ORIGINAL ARTICLE Fibrosis in Human Adipose Tissue: Composition, Distribution, and Link With Lipid Metabolism and Fat Mass Loss Adeline Divoux,1 Joan Tordjman,1 Danie`le Lacasa,2 Nicolas Veyrie,1,3 Danielle Hugol,1,4 Abdelhalim Aissat,1,3 Arnaud Basdevant,1,2 Miche`le Guerre-Millo,1 Christine Poitou,1,2 Jean-Daniel Zucker,1 Pierre Bedossa,1,5 and Karine Cle´ment1,2 OBJECTIVE—Fibrosis is a newly appreciated hallmark of the pathological alteration of human white adipose tissue (WAT). We investigated the composition of subcutaneous (scWAT) and hite adipose tissue (WAT) is the main energy omental WAT (oWAT) fibrosis in obesity and its relationship with repository in the body. It stores and mobi- metabolic alterations and surgery-induced weight loss. lizes, according to body demand, fatty acids RESEARCH DESIGN AND METHODS—Surgical biopsies for Wthat have been implicated in the development scWAT and oWAT were obtained in 65 obese (BMI 48.2 Ϯ 0.8 of insulin resistance. In turns, the phenotype and the kg/m2) and 9 lean subjects (BMI 22.8 Ϯ 0.7 kg/m2). Obese biology of WAT cellular components are altered by two subjects who were candidates for bariatric surgery were major processes: adipose cell hypertrophy and immune clinically characterized before, 3, 6, and 12 months after cells accumulation. Inflammation, reticulum endoplasmic surgery, including fat mass evaluation by dual energy X-ray stress, and hypoxia are part of the biologic alterations that absorptiometry. WAT fibrosis was quantified and character- ized using quantitative PCR, microscopic observation, and attract and retain inflammatory cells in WAT (1). -

Empowering Collagen Targeting for Diagnosis and Treatment of Human Conditions
EmpoweringEmpowering collagen collagen targetingtargeting for for diagnosis prognosis of fibrotic and treatment of Manka,SW. 2012 conditions.human conditions. 1 3Helix as a platform diagnostic company 2020 2022 2030 Innovative research reagent for Clinic histopathology providing Platform fibrotic prognostic detection of collagen damage best in class prognostic ability in within multi-disease states liver fibrosis (NAFLD, NASH) Strengthening IP portfolio with market Clinical histopathology AND Non-Invasive approaches serum testing and medical disrupting products while subsequently Analytic specific reagent to allow for fast imaging developing strong partnerships with world market access leading companies for commercialization Targeting impactful markets of IPF, kidney Focused on paired biopsy research and fibrosis, AMD, Keloids and cardiac fibrosis collaboration with clinical laboratories. in addition to fibrotic liver diseases. 2 Liver Fibrosis market is GROWING Fatty Liver Fibrotic Liver Healthy Liver Cirrhosis NAFLD NASH USA Epidemiology 328 Million 83 Million 16 Million 1.5 Million (2015) Predicted USA Epidemiology 360 Million 101 Million 27 Million 3.4 Million (2030) Estes,C. 2018 3 NASH Therapeutics are finishing clinical trials and are coming to market. • VK2809 Phase II • OCALIVA (OCA) • NDA Filed • $78,000/year current cost • $20,000 predicted • Resmetirom Phase III • 23% respond to treatment 16 Million NASH patients in the USA * $20,000 • $320 Billion Annual Cost for treatable market Aramchol Phase III/IV 4 Stratification of patient population is needed to reduce unnecessary therapeutic intervention. • Progression of NAFL and 100% NASH is variable patient to NAFLD patient. 33% • Prediction of the progression can modify the Fibrosis Progression 20% disease intervention and treatment. Rapid Fibrosis • No product on the market Progression (stage 0 to stage today is equipped for 3/4 over 5.9 years) prognosis of liver fibrosis Singh, S. -

Skeletal Muscle – Fibrosis
Skeletal Muscle – Fibrosis Figure Legend: Figure 1 Skeletal muscle - Fibrosis in a male Harlan Sprague-Dawley rat from a subchronic study. Early change consists of increased perimysial deposits of pale eosinophilic material (immature collagen). Figure 2 Skeletal muscle - Fibrosis in a male Harlan Sprague-Dawley rat from a subchronic study. Note the perimysial proliferation of fibroblasts and early collagen deposition. Figure 3 Skeletal muscle - Fibrosis in a male Harlan Sprague-Dawley rat from a subchronic study (higher magnification of Figure 2). There is deposition of perimysial connective tissue and attenuation of several muscle fibers. Figure 4 Skeletal muscle - Fibrosis in a male F344/N rat from a chronic study. There is marked fibrosis with attenuation and loss of muscle bundles. 1 Skeletal Muscle – Fibrosis Comment: In skeletal muscle, the predominant histologic features of fibrosis are increased numbers of plump reactive fibroblasts with prominent vesiculated nuclei, and increased amounts of pale eosinophilic fibrillar material (collagen deposition) separating and surrounding adjacent myofibers (Figure 1, Figure 2, Figure 3, and Figure 4). Affected myofibers may or may not exhibit histologic features of atrophy, degeneration, necrosis, or regeneration. Fibrosis is the end result of a cascade of events that begins with tissue injury and inflammation and ends in permanent scar formation. When tissue is damaged, profibrotic cytokines, such as transforming growth factor beta, are released by the infiltrating inflammatory cells. These cytokines signal the fibroblasts to migrate into the affected region and to begin producing and remodeling the extracellular matrix. The stromal fibroblasts then begin producing cytokines, growth factors, and proteases that further trigger and uphold the inflammatory/profibrotic conditions.