Analysis of Arterial Blood Gas Values Based on Storage Time Since Sampling: an Observational Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Disappearance of IPO in Myocardium of Diabetes Mellitus Rats Is Associated with the Increase of Succinate Dehydrogenase-Flav
Deng et al. BMC Cardiovasc Disord (2021) 21:142 https://doi.org/10.1186/s12872-021-01949-z RESEARCH ARTICLE Open Access The disappearance of IPO in myocardium of diabetes mellitus rats is associated with the increase of succinate dehydrogenase-favin protein Mengyuan Deng1†, Wei Chen1†, Haiying Wang1*, Yan Wang1, Wenjing Zhou2 and Tian Yu3 Abstract Background: The aim of the present study was to investigate whether the disappearance of ischemic post-process- ing (IPO) in the myocardium of diabetes mellitus (DM) is associated with the increase of succinate dehydrogenase- favin protein (SDHA). Methods: A total of 50 Sprague Dawley rats, weighing 300–400 g, were divided into 5 groups according to the ran- dom number table method, each with 10 rats. After DM rats were fed a high-fat and -sugar diet for 4 weeks, they were injected with Streptozotocin to establish the diabetic rat model. Normal rats were fed the same regular diet for the same number of weeks. Next, the above rats were taken to establish a cardiopulmonary bypass (CPB) model. Intraperi- toneal glucose tolerance test (IPGTT) and oral glucose tolerance test (OGTT) were used to detect whether the DM rat model was established successfully. Taking blood from the femoral artery to collect the blood-gas analysis indicators, and judged whether the CPB model is established. After perfusion was performed according to the experimental strategy, the area of myocardial infarction (MI), and serum creatine kinase isoenzyme (CK-MB) and cardiac troponin (CTnI) levels were measured. Finally, the relative mRNA and protein expression of SDHA was detected. Results: The OGTT and IPGTT suggested that the DM rat model was successfully established. -
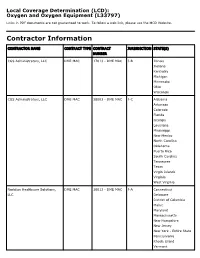
Oxygen and Oxygen Equipment Local Coverage Determination (LCD)
Local Coverage Determination (LCD): Oxygen and Oxygen Equipment (L33797) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER CGS Administrators, LLC DME MAC 17013 - DME MAC J-B Illinois Indiana Kentucky Michigan Minnesota Ohio Wisconsin CGS Administrators, LLC DME MAC 18003 - DME MAC J-C Alabama Arkansas Colorado Florida Georgia Louisiana Mississippi New Mexico North Carolina Oklahoma Puerto Rico South Carolina Tennessee Texas Virgin Islands Virginia West Virginia Noridian Healthcare Solutions, DME MAC 16013 - DME MAC J-A Connecticut LLC Delaware District of Columbia Maine Maryland Massachusetts New Hampshire New Jersey New York - Entire State Pennsylvania Rhode Island Vermont CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, DME MAC 19003 - DME MAC J-D Alaska LLC American Samoa Arizona California - Entire State Guam Hawaii Idaho Iowa Kansas Missouri - Entire State Montana Nebraska Nevada North Dakota Northern Mariana Islands Oregon South Dakota Utah Washington Wyoming LCD Information Document Information LCD ID Original Effective Date L33797 For services performed on or after 10/01/2015 LCD Title Revision Effective Date Oxygen and Oxygen Equipment For services performed on or after 08/02/2020 Proposed LCD in Comment Period Revision Ending Date N/A N/A Source Proposed LCD Retirement Date DL33797 N/A AMA CPT / ADA CDT / AHA NUBC Copyright Notice Period Start Date Statement 06/18/2020 CPT codes, descriptions and other data only are copyright 2019 American Medical Association. All Rights Notice Period End Date Reserved. -

Chronic Cough, Shortness of Breathe, Wheezing? What You Should
CHRONIC COUGH, SHORTNESS OF BREATH, WHEEZING? WHAT YOU SHOULD KNOW ABOUT COPD. A quick guide on Chronic Obstructive Pulmonary Disease COPD.nhlbi.nih.gov COPD, or chronic obstructive Most often, COPD occurs in people pulmonary disease, is a serious lung age 40 and over who… disease that over time makes it hard • Have a history of smoking to breathe. Other names for COPD include • Have had long-term exposure to lung irritants chronic bronchitis or emphysema. such as air pollution, chemical fumes, or dust from the environment or workplace COPD, a leading cause of death, • Have a rare genetic condition called alpha-1 affects millions of Americans and causes antitrypsin (AAT) deficiency long-term disability. • Have a combination of any of the above MAJOR COPD RISK FACTORS history of SMOKING AGE 40+ RARE GENETIC CONDITION alpha-1 antitrypsin (AAT) deficiency LONG-TERM exposure to lung irritants WHAT IS COPD? To understand what COPD is, we first The airways and air sacs are elastic (stretchy). need to understand how respiration When breathing in, each air sac fills up with air like and the lungs work: a small balloon. When breathing out, the air sacs deflate and the air goes out. When air is breathed in, it goes down the windpipe into tubes in the lungs called bronchial In COPD, less air flows in and out of tubes or airways. Within the lungs, bronchial the airways because of one or more tubes branch into thousands of smaller, thinner of the following: tubes called bronchioles. These tubes end in • The airways and air sacs lose bunches of tiny round air sacs called alveoli. -

Guía Práctica Clínica Bronquiolitis.Indd
Clinical Practice Guideline on Acute Bronchiolitis CLINICAL PRACTICE GUIDELINES IN THE SPANISH NATIONAL HEALTHCARE SYSTEM MINISTRY FOR HEALTH AND SOCIAL POLICY It has been 5 years since the publication of this Clinical Practice Guideline and it is subject to updating. Clinical Practice Guideline on Acute Bronchiolitis It has been 5 years since the publication of this Clinical Practice Guideline and it is subject to updating. CLINICAL PRACTICE GUIDELINES IN THE SPANISH NATIONAL HEALTHCARE SYSTEM MINISTRY FOR HEALTH AND SOCIAL POLICY This CPG is an aid for healthcare decisions. It is not binding, and does not replace the clinical judgement of healthcare staff. Published: 2010 It has beenPublished 5 years by: Ministry since for theScience publication and Innovation of this Clinical Practice Guideline and it is subject to updating. NIPO (Official Publication Identification No.): 477-09-055-4 ISBN: pending Legal depository: B-10297-2010 Printed by: Migraf Digital This CPG has been funded via an agreement entered into by the Carlos III Health Institute, an autonomous body within the Spanish Ministry for Science and Innovation, and the Catalan Agency for Health Technology Assessment, within the framework for cooperation established in the Quality Plan for the Spanish National Healthcare System of the Spanish Ministry for Health and Social Policy. This guideline must be cited: Working Group of the Clinical Practice Guideline on Acute Bronchiolitis; Sant Joan de Déu Foundation Fundació Sant Joan de Déu, coordinator; Clinical Practice Guideline on Acute Bronchiolitis; Quality Plan for the Spanish National Healthcare System of the Spanish Ministry for Health and Social Policy; Catalan Agency for Health Technology Assessment, 2010; Clinical Practice Guidelines in the Spanish National Healthcare System: CAHTA no. -

Management of Airway Obstruction and Stridor in Pediatric Patients
November 2017 Management of Airway Volume 14, Number 11 Obstruction and Stridor in Authors Ashley Marchese, MD Department of Pediatrics, Yale-New Haven Hospital, New Haven, CT Pediatric Patients Melissa L. Langhan, MD, MHS Associate Professor of Pediatrics and Emergency Medicine; Fellowship Director, Director of Education, Pediatric Emergency Abstract Medicine, Yale University School of Medicine, New Haven, CT Peer Reviewers Stridor is a result of turbulent air-flow through the trachea from Steven S. Bin, MD upper airway obstruction, and although in children it is often Associate Clinical Professor of Emergency Medicine and Pediatrics; Medical Director, Emergency Department, UCSF School of Medicine, due to croup, it can also be caused by noninfectious and/or con- Benioff Children’s Hospital, San Francisco, CA genital conditions as well as life-threatening etiologies. The his- Alexander Toledo, DO, PharmD, FAAEM, FAAP tory and physical examination guide initial management, which Chief, Section of Pediatric Emergency Medicine; Director, Pediatric Emergency Department, Arizona Children’s Center at Maricopa includes reduction of airway inflammation, treatment of bacterial Medical Center, Phoenix, AZ infection, and, less often, imaging, emergent airway stabilization, Prior to beginning this activity, see “Physician CME Information” or surgical management. This issue discusses the most common on the back page. as well as the life-threatening etiologies of acute and chronic stridor and its management in the emergency department. Editor-in-Chief -

Oxygenation and Oxygen Therapy
Rules on Oxygen Therapy: Physiology: 1. PO2, SaO2, CaO2 are all related but different. 2. PaO2 is a sensitive and non-specific indicator of the lungs’ ability to exchange gases with the atmosphere. 3. FIO2 is the same at all altitudes 4. Normal PaO2 decreases with age 5. The body does not store oxygen Therapy & Diagnosis: 1. Supplemental O2 is an FIO2 > 21% and is a drug. 2. A reduced PaO2 is a non-specific finding. 3. A normal PaO2 and alveolar-arterial PO2 difference (A-a gradient) do NOT rule out pulmonary embolism. 4. High FIO2 doesn’t affect COPD hypoxic drive 5. A given liter flow rate of nasal O2 does not equal any specific FIO2. 6. Face masks cannot deliver 100% oxygen unless there is a tight seal. 7. No need to humidify if flow of 4 LPM or less Indications for Oxygen Therapy: 1. Hypoxemia 2. Increased work of breathing 3. Increased myocardial work 4. Pulmonary hypertension Delivery Devices: 1. Nasal Cannula a. 1 – 6 LPM b. FIO2 0.24 – 0.44 (approx 4% per liter flow) c. FIO2 decreases as Ve increases 2. Simple Mask a. 5 – 8 LPM b. FIO2 0.35 – 0.55 (approx 4% per liter flow) c. Minimum flow 5 LPM to flush CO2 from mask 3. Venturi Mask a. Variable LPM b. FIO2 0.24 – 0.50 c. Flow and corresponding FIO2 varies by manufacturer 4. Partial Rebreather a. 6 – 10 LPM b. FIO2 0.50 – 0.70 c. Flow must be sufficient to keep reservoir bag from deflating upon inspiration 5. -

Prilocaine Induced Methemoglobinemia Güzelliğin Bedeli; Prilokaine Bağlı Gelişen Methemoglobinemi Olgusu
CASE REPORT 185 Cost of Beauty; Prilocaine Induced Methemoglobinemia Güzelliğin Bedeli; Prilokaine Bağlı Gelişen Methemoglobinemi Olgusu Elif KILICLI, Gokhan AKSEL, Betul AKBUGA OZEL, Cemil KAVALCI, Dilek SUVEREN ARTUK Department of Emergency Medicine, Baskent University Faculty of Medicine, Ankara SUMMARY ÖZET Prilocaine induced methemoglobinemia is a rare entity. In the pres- Prilokaine bağlı gelişen methemoglobinemi nadir görülen bir du- ent paper, the authors aim to draw attention to the importance of rumdur. Bu yazıda epilasyon öncesi kullanılan prilokaine sekonder this rare condition by reporting this case. A 30-year-old female gelişen methemoglobinemi olgusunu sunarak nadir görülen bu presented to Emergency Department with headache, dispnea and durumun önemine işaret etmek istiyoruz. Otuz yaşında kadın acil cyanosis. The patient has a history of 1000-1200 mg of prilocaine servise baş ağrısı, dispne ve siyanoz şikayetleri ile başvurdu. Hasta- ya beş saat öncesinde bir güzellik merkezinde epilasyon öncesinde subcutaneous injection for hair removal at a beauty center, 5 hours yaklaşık 1000-1200 mg prilokain subkutan enjeksiyonu yapıldığı ago. Tension arterial: 130/73 mmHg, pulse: 103/minute, body tem- öğrenildi. Başvuruda kan basıncı 130/73 mmHg, nabız 103/dk, vü- perature: 37 °C and respiratory rate: 20/minute. The patient had ac- cut ısısı 37 °C ve solunum sayısı 20/dk olarak kaydedilmişti. Hasta- ral and perioral cyanosis. Methemoglobin was measured 14.1% in nın akral siyanozu belirgindi. Venöz kan gazında methemoglobin venous blood gas test. The patient treated with 3 gr ascorbic acid düzeyi %14.1 olarak ölçüldü. Hastaya 3 g intravenöz askorbik asit intravenously. The patient was discharged free of symptoms after uygulandı. -

Shanti Bhavan Medical Center Biru, Jharkhand, India
Shanti Bhavan Medical Center Biru, Jharkhand, India We Care, He Heals Urgent Needs 1. Boundary Wall around the hospital property Cost: $850,000 In India any land (even owned) can be taken by the government at any time if there is not boundary wall around it. Our organization owns property around the hospital that is intended for the Nursing school and other projects. We need a boundary wall built around the land so that the government can’t recover the land. 2. Magnetic Resonance Imaging Device Cost: $300,000 Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body in both health and disease. MRI scanners use strong magnetic fields, radio waves, and field gradients to generate images of the organs in the body. 3. Kidney Stone Lipotriptor Cost: $200,000 Kidney Stone Lipotriptor Extracorporeal Shock Wave Lithotripsy (ESWL) is the least invasive surgical stone treatment using high frequency sound waves from an external source (outside the body) to break up kidney stones into smaller pieces, and allow them to pass out through the urinary tract. 4. Central Patient Monitoring System Cost: $28,000 Central Patient Monitoring System- A full-featured system that provides comprehensive patient monitoring and review. Monitors up to 32 patients using two displays and is ideal for telemetry, critical care, OR, emergency room, and other monitoring environments. Provides data storage and review capabilities, and ensures a complete patient record by facilitating automated patient and data transfer between multiple departments. 5. ABG Machine Cost: $25,000 ABG machine- An arterial blood gas test (ABG) is a blood gas test of blood taken from an artery that measures the amounts of certain gases (such as oxygen and carbon diox- ide) dissolved in arterial blood. -

How Is Pulmonary Fibrosis Diagnosed?
How Is Pulmonary Fibrosis Diagnosed? Pulmonary fibrosis (PF) may be difficult to diagnose as the symptoms of PF are similar to other lung diseases. There are many different types of PF. If your doctor suspects you might have PF, it is important to see a specialist to confirm your diagnosis. This will help ensure you are treated for the exact disease you have. Health History and Exam Your doctor will perform a physical exam and listen to your lungs. • If your doctor hears a crackling sound when listening to your lungs, that is a sign you might have PF. • It is also important for your doctor to gather detailed information about your health. ⚪ This includes any family history of lung disease, any hazardous materials you may have been exposed to in your lifetime and any diseases you’ve been treated for in the past. Imaging Tests Tests like chest X-rays and CT scans can help your doctor look at your lungs to see if there is any scarring. • Many people with PF actually have normal chest X-rays in the early stages of the disease. • A high-resolution computed tomography scan, or HRCT scan, is an X-ray that provides sharper and more detailed pictures than a standard chest X-ray and is an important component of diagnosing PF. • Your doctor may also perform an echocardiogram (ECHO). ⚪ This test uses sound waves to look at your heart function. ⚪ Doctors use this test to detect pulmonary hypertension, a condition that can accompany PF, or abnormal heart function. Lung Function Tests There are several ways to test how well your lungs are working. -

Rapid Diagnosis of Ethylene Glycol Poisoning by Urine Microscopy
University of Southern Denmark Rapid diagnosis of ethylene glycol poisoning by urine microscopy Sheta, Hussam Mahmoud; Al-Najami, Issam; Christensen, Heidi Dahl; Madsen, Jonna Skov Published in: American Journal of Case Reports DOI: 10.12659/AJCR.908569 Publication date: 2018 Document version: Final published version Document license: CC BY-NC-ND Citation for pulished version (APA): Sheta, H. M., Al-Najami, I., Christensen, H. D., & Madsen, J. S. (2018). Rapid diagnosis of ethylene glycol poisoning by urine microscopy. American Journal of Case Reports, 19, 689-693. https://doi.org/10.12659/AJCR.908569 Go to publication entry in University of Southern Denmark's Research Portal Terms of use This work is brought to you by the University of Southern Denmark. Unless otherwise specified it has been shared according to the terms for self-archiving. If no other license is stated, these terms apply: • You may download this work for personal use only. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying this open access version If you believe that this document breaches copyright please contact us providing details and we will investigate your claim. Please direct all enquiries to [email protected] Download date: 28. Sep. 2021 e-ISSN 1941-5923 © Am J Case Rep, 2018; 19: 689-693 DOI: 10.12659/AJCR.908569 Received: 2017.12.17 Accepted: 2018.03.21 Rapid Diagnosis of Ethylene Glycol Poisoning by Published: 2018.06.14 Urine Microscopy Authors’ Contribution: -
ILD Nursing and Allied Health Guide
ILD Nursing and Allied Health Guide 230 East Ohio Street, Suite 500 Chicago, Illinois 60611 844.TalkPFF (844.825.5733) pulmonaryfibrosis.org The Pulmonary Fibrosis Foundation mobilizes people and resources to provide access to high quality care and leads research for a cure so people with pulmonary fibrosis will live longer, healthier lives. © 2020 Pulmonary Fibrosis Foundation. All rights reserved. Table of Contents Dear Nurses and Allied Health Professionals ........................................................................ 2 Introduction ................................................................................................................................ 3 PART ONE: IDENTIFYING THE DISEASE ....................................................................... 4 Recognition of ILD ................................................................................................................... 4 The Diagnostic Process ............................................................................................................. 4 Idiopathic Interstitial Pneumonias .......................................................................................... 6 PART TWO: INTERPRETING TEST RESULTS ................................................................ 6 High-resolution computerized tomography scans (HRCT) ................................................. 6 Pulmonary Function Tests (PFTs) .......................................................................................... 8 Pulmonary Function Test (PFT) Report -

Diagnostic Performance of Initial Serum Albumin Level for Predicting In-Hospital Mortality Among Necrotizing Fasciitis Patients
Article Diagnostic Performance of Initial Serum Albumin Level for Predicting In-Hospital Mortality among Necrotizing Fasciitis Patients Chia-Peng Chang 1, Wen-Chih Fann 1,2, Shu-Ruei Wu 3, Chun-Nan Lin 1, I-Chuan Chen 1,2, and Cheng-Ting Hsiao 1,2,* 1 Department of Emergency Medicine, Chang Gung Memorial Hospital, No.6, Sec. W., Jiapu Rd., Puzi City, Chiayi County 613, Taiwan; [email protected] (C.-P.C.); [email protected] (W.-C.F.); [email protected] (C.-N.L.); [email protected] (I.-C.C.) 2 Department of Medicine, Chang Gung University, Taoyuan 333, Taiwan 3 Department of Pediatrics, Kaohsiung Veterans General Hospital, Kaohsiung 813, Taiwan; [email protected] * Correspondence: [email protected]; Tel.: +886-975352985, Fax: +886-53622790 Received: 16 October 2018; Accepted: 8 November 2018; Published: 10 November 2018 Abstract: Background: Hypoalbuminemia is known to be associated with adverse outcomes in critical illness. In this study, we attempted to identify whether hypoalbuminemia on emergency department (ED) arrival is a reliable predictor for in-hospital mortality in necrotizing fasciitis (NF). patients. Method: A retrospective cohort study of hospitalized adult patients with NF was conducted in a tertiary teaching hospital in Taiwan between March 2010 and March 2018. Blood samples were collected in the ED upon arrival, and serum albumin levels were determined. We evaluated the predictive value of serum albumin level at ED presentation for in-hospital mortality. All collected data were statistically analyzed. Result: Of the 707 NF patients, 40 (5.66%) died in the hospital. The mean serum albumin level was 3.1 ± 0.9 g/dL and serum albumin levels were significantly lower in the non-survivor group than in the survivor group (2.8 ± 0.7 g/dL vs.