Hemophilia Update 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protein S Deficiency Presenting with Hemorrhage in a Term Neonate
: Curre re nt a R C e Ayari et al., Health Care Current Reviews 2018, 6:1 h v t i l e a w DOI: 10.4172/2375-4273.1000219 e s H Health Care: Current Reviews ISSN: 2375-4273 Review Article Open Access Protein S Deficiency Presenting with Hemorrhage in a Term Neonate Fairouz Ayari*, Takoua Bensmail, Essid Latifa, Wiem Barbaria and Samia Kacem Neonatology Intensive Care Unit of the Maternity and Neonatology Center, Tunis, Tunisia Abstract Unexplained bleeding symptoms in otherwise healthy full-term usually present a diagnostic challenge for treating physicians requiring prompt and accurate laboratory investigations to ensure appropriate treatment and possibly avoid long-term morbidity. We report a case of a term neonate with severe protein S deficiency manifested by systemic hemorrhage and multiple organ failure at 9 days of age. We review how protein S influences the coagulation and the fibrinolytic pathways, discussing therapeutic approaches of neonates with purpura fulminans. Keywords: Protein S deficiency; Blood sample; Thrombophilic dis- resuscitation with 20 ml/kg bodyweight (BW) saline solution and, after order blood sampling, intravenous administration of 10 mg vitamin K, 20 ml/kg BW fresh frozen plasma, 20 ml/kg BW packed red blood cells Introduction (5 transfusion cycles), 20 mg/kg BW Phenobarbital and vasoactive Protein S (PS) is an antithrombotic plasma protein that acts mainly drugs. Cerebral ultrasound revealed intraventricular haemorrhage, as a cofactor of activated protein C (APC) anticoagulant activity in the abdominal ultrasound showed splenic hemorrhage and cardiac degradation of factor Va and activated factor VIII [1]. PS circulates in ultrasound showed a floating intracardiac thrombus. -

Evans Syndrome As Rare Presentation in Systemic Lupus Erythematosus
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Case Report Evans Syndrome as Rare Presentation in Systemic Lupus Erythematosus Dr Sabarish Mahalingam1, Dr P. Z. Wadia2, Dr Priyanka Lad1 1Resident Doctor, Department of Internal Medicine, Government Medical College, Surat 2Additional Professor, Department of Internal Medicine, Government Medical College, Surat Corresponding Author: Dr Sabarish Mahalingam ABSTRACT Evans syndrome is a rare disorder in which the body’s immune system produces antibodies that mistakenly destroy red blood cells, platelets and sometimes certain white blood cell known as neutrophils. It is one of the rare presenting features of autoimmune disorders, especially systemic lupus erythematosus (SLE), and sometimes may even precede the onset of disease. Primary Evans syndrome with no cause is very rare and is seen in children. Here, we describe a case of secondary Evans syndrome with severe autoimmune hemolytic anemia leading to acute kidney injury. This is one of the rare presentations of SLE and there are only few case reports. Key word: Evans syndrome, systemic lupus erythematosus, autoimmune haemolytic anaemia. INTRODUCTION literature; [9-11] therefore, the characteristics Evans syndrome (ES), which was and outcome of adult's ES are poorly first described in 1951, is an autoimmune known. disorder characterized by the simultaneous or sequential development of autoimmune CASE REPORT hemolytic anemia (AIHA) and immune A 28 aged female came to (ITP) and/or immune neutropenia in the emergency department with the complain of absence of any underlying cause. [1,2] ES has breathlessness for past 5 days. On been since its first description considered or examination, patient was pale and defined as an “idiopathic” condition and tachypneic, systemic examination was thus mainly as a diagnosis of exclusion, ES normal. -

MYH9-Related Platelet Disorders
Reprinted with permission from Thieme Medical Publishers (Semin Thromb Hemost 2009;35:189-203) Homepage at www.thieme.com MYH9-Related Platelet Disorders Karina Althaus, M.D.,1 and Andreas Greinacher, M.D.1 ABSTRACT Myosin heavy chain 9 (MYH9)-related platelet disorders belong to the group of inherited thrombocytopenias. The MYH9 gene encodes the nonmuscle myosin heavy chain IIA (NMMHC-IIA), a cytoskeletal contractile protein. Several mutations in the MYH9 gene lead to premature release of platelets from the bone marrow, macro- thrombocytopenia, and cytoplasmic inclusion bodies within leukocytes. Four overlapping syndromes, known as May-Hegglin anomaly, Epstein syndrome, Fechtner syndrome, and Sebastian platelet syndrome, describe different clinical manifestations of MYH9 gene mutations. Macrothrombocytopenia is present in all affected individuals, whereas only some develop additional clinical manifestations such as renal failure, hearing loss, and presenile cataracts. The bleeding tendency is usually moderate, with menorrhagia and easy bruising being most frequent. The biggest risk for the individual is inappropriate treatment due to misdiagnosis of chronic autoimmune thrombocytopenia. To date, 31 mutations of the MYH9 gene leading to macrothrombocytopenia have been identified, of which the upstream mutations up to amino acid 1400 are more likely associated with syndromic manifestations than the downstream mutations. This review provides a short history of MYH9-related disorders, summarizes the clinical and laboratory character- istics, describes a diagnostic algorithm, presents recent results of animal models, and discusses aspects of therapeutic management. KEYWORDS: MYH9 gene, nonmuscle myosin IIA, May-Hegglin anomaly, Epstein syndrome, Fechtner syndrome, Sebastian platelet syndrome, macrothrombocytopenia The correct diagnosis of hereditary chronic as isolated platelet count reductions or as part of thrombocytopenias is important for planning appropri- more complex clinical syndromes. -

Case Report Treatment of Severe Evans Syndrome with an Allogeneic Cord Blood Transplant
Bone Marrow Transplantation, (1997) 20, 427–429 1997 Stockton Press All rights reserved 0268–3369/97 $12.00 Case report Treatment of severe Evans syndrome with an allogeneic cord blood transplant E Raetz1, PG Beatty2 and RH Adams1 Departments of 1Pediatrics and 2Medicine, University of Utah School of Medicine, Salt Lake City, UT, USA Summary: began experiencing increased difficulty with mucosal bleeding, which prompted frequent platelet transfusions. At Immunosuppressive therapy is commonly used in the 4. years, he had a major gastrointestinal bleed, followed management of autoimmune disorders. As marrow- 1 month later by an intracranial hemorrhage. He required derived lymphocytes appear to play a key role in these transient ventilator support, but eventually regained full diseases, lymphoid ablation followed by replacement neurologic function. Direct (DAT) and indirect (IAT) with autologous or allogeneic stem cells may be a thera- Coombs evaluations were always 3+ positive. Due to the peutic option. We report a 5-year-old boy with severe severe and refractory nature of his disease, the option of Evans syndrome which consists of immune thrombocy- novel therapy with bone marrow transplantation was topenia and Coombs-positive hemolytic anemia. He was pursued. rendered into complete remission with marrow ablation HLA typing of the family, and a search of the unrelated followed by rescue with an HLA-identical sibling cord marrow donor registries, did not identify an appropriate blood transplant. He unexpectedly died 9 months donor, but DNA-based typing for HLA-A, -B, -DRB1 of following transplant from acute hepatic failure of the amniotic fluid of a sibling fetus, of 6 months gestational unknown etiology. -

Case Report Evans Syndrome
Bangladesh Med J. 2018 Sept; 47(3) Case Report Evans Syndrome: A Case Report *Biswas SK1, BiswasT2, Khondoker N3, Alam MR4, Rahim MA5, Paul HK6, Shahin MA7, Hasan MN 8, Bhuiyan AKMM9 Abstract: INTRODUCTION Evans syndrome, a combined clinical condition of autoimmune Evans syndrome is an uncommon clinical condition de!ned haemolytic anaemia (AHA) and idiopathic thrombocytopaenic by the combination of autoimmune hemolytic anemia 1 purpura (ITP) and has non-speci!c pathogenesis. "e clinical (AHA) and idiopathic thrombocytopenic purpura (ITP). It cases are extremely rare, since only 4% of AHA or ITP are is a chronic immune- associated disease which has unknown incorporated with Evans. It is distinguished from di#erentials, pathophysiology. "e true Evans syndrome is diagnosed such as lupus, IgA de!ciency, and acquired immunode!ciency, when possibility of other confounding disorders is excluded. by peripheral blood !lm, bone marrow, Coombs test, and In 1951, Dr. Robert Evan discovered the spectrum like coagulation pro!le. A case of adult female from Pabna, relationship between these two combined diseases after 1 Bangladesh is documented in this report. She complained of studying twenty-four cases. Epidemiologically, the high grade intermittent fever, exertional dyspnea, icteric skin condition is extremely rare that only less than 4% of ITP or 2-5 and sclera. Other features included mild splenomegaly, dark AHA are diagnosed as Evans syndrome. "ere is evidence urine, and profuse sweating after fever. Investigation reports of both cellular and humoral immune-abnormalities in 6 were consistent with AHA and ITP, with normal coagulation Evans syndrome. Di#erent scientists provided di#erent and viral pro!le. -

Outcomes of Patients with Thrombocytopenia Evaluated at Hematology Subspecialty Clinics
Henry Ford Health System Henry Ford Health System Scholarly Commons Hematology Oncology Articles Hematology-Oncology 2-11-2021 Outcomes of patients with thrombocytopenia evaluated at hematology subspecialty clinics Zaid H. Abdel Rahman Kevin C. Miller H Jabbour Yaser Alkhatib Vijayalakshmi Donthireddy Follow this and additional works at: https://scholarlycommons.henryford.com/ hematologyoncology_articles Hematol Oncol Stem Cell Ther xxx (xxxx) xxx Available at www.sciencedirect.com ScienceDirect journal homepage: www.elsevier.com/locate/hemonc Outcomes of patients with thrombocytopenia evaluated at hematology subspecialty clinics Zaid H. Abdel Rahman a,*, Kevin C. Miller b, Hiba Jabbour c, Yaser Alkhatib c, Vijaya Donthireddy c a Division of Hematology and Medical Oncology, Mayo Clinic, Jacksonville, FL, USA b Department of Medicine, Massachusetts General Hospital, Boston, MA, USA c Division of Hematology and Medical Oncology, Henry Ford Hospital, Detroit, MI, USA Received 6 October 2020; received in revised form 9 December 2020; accepted 15 January 2021 KEYWORDS Abstract Hematology; Background: Thrombocytopenia is a frequently encountered laboratory abnormality and a Malignancy; common reason for hematology referrals. Workup for thrombocytopenia is not standardized Platelets; and frequently does not follow an evidence-based algorithm. We conducted a systematic anal- Referrals; Thrombocytopenia ysis to evaluate the laboratory testing and outcomes of patients evaluated for thrombocytope- nia at hematology clinics in a tertiary referral center between 2013 and 2016. Patient and methods: We performed a comprehensive chart review for patients evaluated for thrombocytopenia during the study period. Patients were followed for 1 year from the initial hematology evaluation and assessed for the development of a hematologic malignancy, rheumatologic, or infectious diseases among other clinical outcomes. -

Diagnosis of Inherited Platelet Disorders on a Blood Smear
Journal of Clinical Medicine Article Diagnosis of Inherited Platelet Disorders on a Blood Smear Carlo Zaninetti 1,2,3 and Andreas Greinacher 1,* 1 Institut für Immunologie und Transfusionsmedizin, Universitätsmedizin Greifswald, 17489 Greifswald, Germany; [email protected] 2 University of Pavia, and IRCCS Policlinico San Matteo Foundation, 27100 Pavia, Italy 3 PhD Program of Experimental Medicine, University of Pavia, 27100 Pavia, Italy * Correspondence: [email protected]; Tel.: +49-3834-865482; Fax: +49-3834-865489 Received: 19 January 2020; Accepted: 12 February 2020; Published: 17 February 2020 Abstract: Inherited platelet disorders (IPDs) are rare diseases featured by low platelet count and defective platelet function. Patients have variable bleeding diathesis and sometimes additional features that can be congenital or acquired. Identification of an IPD is desirable to avoid misdiagnosis of immune thrombocytopenia and the use of improper treatments. Diagnostic tools include platelet function studies and genetic testing. The latter can be challenging as the correlation of its outcomes with phenotype is not easy. The immune-morphological evaluation of blood smears (by light- and immunofluorescence microscopy) represents a reliable method to phenotype subjects with suspected IPD. It is relatively cheap, not excessively time-consuming and applicable to shipped samples. In some forms, it can provide a diagnosis by itself, as for MYH9-RD, or in addition to other first-line tests as aggregometry or flow cytometry. In regard to genetic testing, it can guide specific sequencing. Since only minimal amounts of blood are needed for the preparation of blood smears, it can be used to characterize thrombocytopenia in pediatric patients and even newborns further. -

Severe Fever with Thrombocytopenia Syndrome: a Newly Discovered Emerging Infectious Disease
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector REVIEW Severe fever with thrombocytopenia syndrome: a newly discovered emerging infectious disease D. X. Li Key Laboratory for Medical Virology, National Institute for Viral Disease Control and Prevention, China CDC, Beijing, China Abstract Severe fever with thrombocytopenia syndrome (SFTS) is a newly discovered emerging infectious disease that has recently become epidemic in Asia. The causative agent of SFTS is a novel phlebovirus in the family Bunyaviridae, designated SFTS virus (SFTSV). SFTS clinically presents with high fever, thrombocytopenia, leukocytopenia, gastrointestinal disorders, and multi-organ dysfunction, with a high viral load and a high case- fatality rate. In human infection, SFTSV targets microphages, replicates in the spleen of infected mice, and causes thrombocytopenia and a cytokine storm. The tick disseminates virus to humans and animals, forming a special transmission model in nature. Person-to-person transmission though direct contact with patient blood has been frequently reported. Measurements of viral RNA and antibodies have been established for diagnosis, but vaccines and specific therapeutics are not available so far. Clinical Microbiology and Infection © 2015 European Society of Clinical Microbiology and Infectious Diseases. Published by Elsevier Ltd. All rights reserved. Keywords: Clinical, epidemiology, SFTS virus, SFTS, virology Article published online: 11 March 2015 Virology D.X. Li, Key Laboratory for Medical Virology, NCHFP, RRC, National Institute for Viral Disease Control and Prevention, China CDC, Bei- jing 102206, China E-mail: [email protected] The causative agent of SFTS is SFTSV, which is a tick-borne virus in the family Bunyaviridae, genus Phlebovirus. -

Gri Trombosit Sendromu
Cukurova Medical Journal Cukurova Med J 2017;42(2):360-362 ÇUKUROVA ÜNİVERSİTESİ TIP FAKÜLTESİ DERGİSİ DOI: 10.17826/cutf.322967 OLGU SUNUMU / CASE REPORT Gray platelet syndrome Gri trombosit sendromu Fatima Ayaz1, Saeed Bin Ayaz2, Sunila Tashfeen2, Muhammad Furrukh1 1Benazir Bhutto Hospital, Rawalpindi, Punjab, Pakistan 2Combined Military Hospital, Okara, Punjab, Pakistan Cukurova Medical Journal 2017;42(2):360-362 Abstract Öz Gray platelet syndrome (GPS) is an autosomal recessive Gri trombosit (platelet) sendromu (GPS), trombositopeni disorder characterized by thrombocytopenia and defective ve ışık mikroskopunda soluk görünen kusurlu platelets that appear pale on light microscope. Patients trombositlerle karakterize, otozomal resesif geçişli bir present with easy bruisability, nose bleeds, menorrhagia hastalıktır. Hastalarda kolay morarma, burun kanaması, and prolonged bleeding. There is no specific treatment for menoraji ve uzun kanamalar görülmektedir. GPS için GPS and the management includes anticipating risks and spesifik bir tedavi bulunmamaktadır dolayısı ile hastalığa preventing bleeding by avoiding drugs that impair platelet karşı, riskleri öngörmek ve kanamanın önlenmesi function. We present here report of a case who presented için trombosit fonksiyonunu bozan ilaçlardan kaçınmak with repeated episodes of abnormal bleeding and was gerekmektedir. Bu olgu sunumunda, tekrarlayan anormal found to have GPS. kanama atakları olan ve GPS bulgusu bulunan bir vaka sunulmaktadır. Key words: Bleeding disorder, gray platelet syndrome, Anahtar -

Neonatal Leukopenia and Thrombocytopenia
Neonatal Leukopenia and Thrombocytopenia Vandy Black, M.D., M.Sc., FAAP March 3, 2016 April 14, 2011 Objecves • Summarize the differenHal diagnosis of leukopenia and/or thrombocytopenia in a neonate • Describe the iniHal steps in the evaluaon of a neonate with leukopenia and/or thrombocytopenia • Review treatment opHons for leukopenia and/ or thrombocytopenia in the NICU Clinical Case 1 • One day old male infant admiUed to the NICU for hypoglycemia and a sepsis rule out • Born at 38 weeks EGA by SVD • Birth weight 4 lbs 13 oz • Exam shows a small cephalohematoma; no dysmorphic features • PLT count 42K with an otherwise normal CBC Definions • Normal WBC count 9-30K at birth – Mean 18K • What is the ANC and ALC – <1000/mm3 is abnormal – 6-8% of infants in the NICU • Normal platelet count: 150-450,000/mm3 – Not age dependent – 22-35% of infants in the NICU have plts<150K Neutropenia Absolute neutrophil count <1500/mm3 Category ANC* InfecHon risk • Mild 1000-1500 None • Moderate 500-1000 Minimal • Severe <500 Moderate to Severe (Highest if <200) • Recurrent bacterial or fungal infecHons are the hallmark of symptomac neutropenia! • *ANC = WBC X % (PMNs + Bands) / 100 DefiniHon of Neutropenia Black and Maheshwari, Neoreviews 2009 How to Approach Cytopenias • Normal vs. abnormal (consider severity) • Malignant vs. non-malignant • Congenital vs. acquired • Is the paent symptomac • Transient, recurrent, cyclic, or persistent How to Approach Cytopenias • Adequate vs. decreased marrow reserve • Decreased producHon vs. increased destrucHon/sequestraon Decreased neutrophil/platelet producon • Primary – Malignancy/leukemia/marrow infiltraon – AplasHc anemia – Genec disorders • Secondary – InfecHous – Drug-induced – NutriHonal • B12, folate, copper Increased destrucHon/sequestraon • Immune-mediated • Drug-induced • Consumpon à Hypersplenism vs. -

Platelet Function Disorders
TREATMENT OF HEMOPHILIA APRIL 2008 • NO 19 PLATELET FUNCTION DISORDERS Second Edition Anjali A. Sharathkumar Amy Shapiro Indiana Hemophilia and Thrombosis Center Indianapolis, U.S.A. Published by the World Federation of Hemophilia (WFH), 1999; revised 2008. © World Federation of Hemophilia, 2008 The WFH encourages redistribution of its publications for educational purposes by not-for-profit hemophilia organizations. In order to obtain permission to reprint, redistribute, or translate this publication, please contact the Communications Department at the address below. This publication is accessible from the World Federation of Hemophilia’s website at www.wfh.org. Additional copies are also available from the WFH at: World Federation of Hemophilia 1425 René Lévesque Boulevard West, Suite 1010 Montréal, Québec H3G 1T7 CANADA Tel. : (514) 875-7944 Fax : (514) 875-8916 E-mail: [email protected] Internet: www.wfh.org The Treatment of Hemophilia series is intended to provide general information on the treatment and management of hemophilia. The World Federation of Hemophilia does not engage in the practice of medicine and under no circumstances recommends particular treatment for specific individuals. Dose schedules and other treatment regimes are continually revised and new side effects recognized. WFH makes no representation, express or implied, that drug doses or other treatment recommendations in this publication are correct. For these reasons it is strongly recommended that individuals seek the advice of a medical adviser and/or consult printed instructions provided by the pharmaceutical company before administering any of the drugs referred to in this monograph. Statements and opinions expressed here do not necessarily represent the opinions, policies, or recommendations of the World Federation of Hemophilia, its Executive Committee, or its staff. -
Thrombocytopenia.Pdf
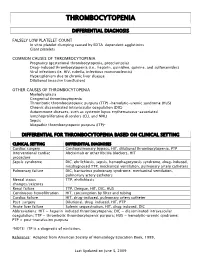
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery