External Jugular Venous Sampling for Cushing's Disease in a Patient With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Non-Pathological Opacification of the Cavernous Sinus on Brain CT
healthcare Article Non-Pathological Opacification of the Cavernous Sinus on Brain CT Angiography: Comparison with Flow-Related Signal Intensity on Time-of-Flight MR Angiography Sun Ah Heo 1, Eun Soo Kim 1,* , Yul Lee 1, Sang Min Lee 1, Kwanseop Lee 1 , Dae Young Yoon 2, Young-Su Ju 3 and Mi Jung Kwon 4 1 Department of Radiology, Hallym University Sacred Heart Hospital, College of Medicine, Hallym University, Seoul 14068, Korea; [email protected] (S.A.H.); [email protected] (Y.L.); [email protected] (S.M.L.); [email protected] (K.L.) 2 Department of Radiology, Kangdong Sacred Heart Hospital, College of Medicine, Hallym University, Seoul 14068, Korea; [email protected] 3 National Medical Center, Seoul 04564, Korea; [email protected] 4 Department of Pathology, Hallym University Sacred Heart Hospital, College of Medicine, Hallym University, Seoul 14068, Korea; [email protected] * Correspondence: [email protected] Abstract: Purpose: To investigate the non-pathological opacification of the cavernous sinus (CS) on brain computed tomography angiography (CTA) and compare it with flow-related signal intensity (FRSI) on time-of-flight magnetic resonance angiography (TOF-MRA). Methods: Opacification of the CS was observed in 355 participants who underwent CTA and an additional 77 participants who underwent examination with three diagnostic modalities: CTA, TOF-MRA, and digital subtraction angiography (DSA). Opacification of the CS, superior petrosal sinus (SPS), inferior petrosal sinus Citation: Heo, S.A.; Kim, E.S.; Lee, Y.; Lee, S.M.; Lee, K.; Yoon, D.Y.; Ju, Y.-S.; (IPS), and pterygoid plexus (PP) were also analyzed using a five-point scale. -

Hemodynamic Features in Normal and Cavernous Sinus Dural ORIGINAL RESEARCH Arteriovenous Fistulas
Published September 6, 2012 as 10.3174/ajnr.A3252 Superior Petrosal Sinus: Hemodynamic Features in Normal and Cavernous Sinus Dural ORIGINAL RESEARCH Arteriovenous Fistulas R. Shimada BACKGROUND AND PURPOSE: Normal hemodynamic features of the superior petrosal sinus and their H. Kiyosue relationships to the SPS drainage from cavernous sinus dural arteriovenous fistulas are not well known. We investigated normal hemodynamic features of the SPS on cerebral angiography as well as the S. Tanoue frequency and types of the SPS drainage from CSDAVFs. H. Mori T. Abe MATERIALS AND METHODS: We evaluated 119 patients who underwent cerebral angiography by focusing on visualization and hemodynamic status of the SPS. We also reviewed selective angiography in 25 consecutive patients with CSDAVFs; we were especially interested in the presence of drainage routes through the SPS from CSDAVFs. RESULTS: In 119 patients (238 sides), the SPS was segmentally (anterior segment, 37 sides; posterior segment, 82 sides) or totally (116 sides) demonstrated. It was demonstrated on carotid angiography in 11 sides (4.6%), receiving blood from the basal vein of Rosenthal or sphenopetrosal sinus, and on vertebral angiography in 235 sides (98.7%), receiving blood from the petrosal vein. No SPSs were demonstrated with venous drainage from the cavernous sinus. SPS drainage was found in 7 of 25 patients (28%) with CSDAVFs. CSDAVFs drained through the anterior segment of SPS into the petrosal vein without draining to the posterior segment in 3 of 7 patients (12%). CONCLUSIONS: The SPS normally works as the drainage route receiving blood from the anterior cerebellar and brain stem venous systems. -

Original Article Construction of a Three-Dimensional Interactive Digital
Int J Clin Exp Med 2018;11(4):3078-3085 www.ijcem.com /ISSN:1940-5901/IJCEM0063223 Original Article Construction of a three-dimensional interactive digital atlas of the dural sinus and deep veins based on human head magnetic resonance images by a comprehensive modeling protocol Zhirong Yang, Zhilin Guo Department of Neurosurgical, The Ninth People Hospital, Medical School, Shanghai Jiaotong University, Shanghai 200011, China Received August 7, 2017; Accepted January 25, 2018; Epub April 15, 2018; Published April 30, 2018 Abstract: Objectives: To design a three-dimensional (3D) interactive digital atlas of the human dural sinus and deep veins for assisting neurosurgeons in preoperative planning and neurosurgical training. Methods: Sagittal head mag- netic resonance (MR) images were obtained of a 54-year-old female who suffered from left posterior fossa tumor. A comprehensive modeling protocol consisting of five steps including thresholding, crop mask, region growing, 3D calculating and 3D editing was used to develop a 3D digital atlas of the dural sinuses and deep veins based on the MR images. The accuracy of the atlas was also evaluated. Results: The 3D digital atlas of the human dural sinus and deep veins was successfully constructed using 176 sagittal head MR images. The contours of the acquired model matched very well with the corresponding structures of the original images in axial and oblique view of MR cross- sections. The atlas can be arbitrarily rotated and viewed from any direction. It can also be zoomed in and out directly using the zoom function. Conclusion: A 3D digital atlas of human dural sinus and deep veins was successfully cre- ated, it can be used for repeated observations and research purposes without limitations of time and shortage of corpses. -

Dural Venous Sinuses Dr Nawal AL-Shannan Dural Venous Sinuses ( DVS )
Dural venous sinuses Dr Nawal AL-Shannan Dural venous sinuses ( DVS ) - Spaces between the endosteal and meningeal layers of the dura Features: 1. Lined by endothelium 2. No musculare tissue in the walls of the sinuses 3. Valueless 4.Connected to diploic veins and scalp veins by emmissary veins .Function: receive blood from the brain via cerebral veins and CSF through arachnoid villi Classification: 15 venous sinuses Paried venous sinuses Unpaired venous sinuses ( lateral in position) • * superior sagittal sinus • * cavernous sinuses • * inferior sagittal sinus • * superior petrosal sinuses • * occipital sinus • * inferior petrosal sinuses • * anterior intercavernous • * transverse sinuses • sinus * sigmoid sinuses • * posterior intercavernous • * spheno-parietal sinuses • sinus • * middle meningeal veins • * basilar plexuses of vein SUPERIOR SAGITTAL SINUS • Begins in front at the frontal crest • ends behind at the internal occipital protuberance diliated to form confluence of sinuses and venous lacunae • • The superior sagittal sinus receives the following : • 1- Superior cerebral veins • 2- dipolic veins • 3- Emissary veins • 4- arachnoid granulation • 5- meningeal veins Clinical significance • Infection from scalp, nasal cavity & diploic tissue • septic thrombosis • CSF absorption intra cranial thrombosis (ICT) • Inferior sagittal sinus - small channel occupy • lower free magin of falx cerebri ( post 2/3) - runs backward and • joins great cerebral vein at free margin of tentorium cerebelli to form straight sinus. • - receives cerebral -
The LATIN LANGUAGE and Bases of Medical Terminology
The LATIN LANGUAGE and Bases of Medical Terminology The LATIN LANGUAGE and Bases of Medical Terminology ОДЕСЬКИЙ ДЕРЖАВНИЙ МЕДИЧНИЙ УНІВЕРСИТЕТ THE ODESSA STATE MEDICAL UNIVERSITY Áiáëiîòåêà ñòóäåíòà-ìåäèêà Medical Student’s Library Започатковано 1999 р. на честь 100-річчя Одеського державного медичного університету (1900–2000 рр.) Initiated in 1999 to mark the Centenary of the Odessa State Medical University (1900–2000) 2 THE LATIN LANGUAGE AND BASES OF MEDICAL TERMINOLOGY Practical course Recommended by the Central Methodical Committee for Higher Medical Education of the Ministry of Health of Ukraine as a manual for students of higher medical educational establishments of the IV level of accreditation using English Odessa The Odessa State Medical University 2008 3 BBC 81.461я73 UDC 811.124(075.8)61:001.4 Authors: G. G. Yeryomkina, T. F. Skuratova, N. S. Ivashchuk, Yu. O. Kravtsova Reviewers: V. K. Zernova, doctor of philological sciences, professor of the Foreign Languages Department of the Ukrainian Medical Stomatological Academy L. M. Kim, candidate of philological sciences, assistant professor, the head of the Department of Foreign Languages, Latin Language and Bases of Medical Terminology of the Vinnitsa State Medical University named after M. I. Pyrogov The manual is composed according to the curriculum of the Latin lan- guage and bases of medical terminology for medical higher schools. Designed to study the bases of general medical and clinical terminology, it contains train- ing exercises for the class-work, control questions and exercises for indivi- dual student’s work and the Latin-English and English-Latin vocabularies (over 2,600 terms). For the use of English speaking students of the first year of study at higher medical schools of IV accreditation level. -

Neurosurgical Forum Tissue Pressure in the Scalp
Neurosurgical forum tissue pressure in the scalp. In our simulation, therefore, bility of overdrainage from the foramen of Monro was we included this variable factor in different ranges to pro- unavoidable, as shown in the same figure (Fig. 7). duce unique correlation between the closing pressure of We therefore searched for a different implantation site, the valves and the flow performance. namely the mastoid process and clavicle. It has been sug- The authors’ assumption of the Delta chamber’s ability gested by Tokoro and Chiba3 that one implant the ASD to “diffuse” the pressure could in no way ensure the effi- valve 10 cm below the level of the foramen of Monro, but cacy of their valve in maintaining the closing pressure no such suggestion has been made for implantation of the uniformly in different head positions, as the diffuse hydro- Delta valve. Because of our familiarity with the less hos- static pressure on the valve has been established in rela- pitable subcutaneous environment in the mastoid region tion to the closing pressure change of the valves (Fig. 5 of and/or clavicle, we also examined the shunt flow charac- the article). teristics with variable external pressure (5–9 cm H2O) and We can address Dr. Pollay’s question regarding the suggested that the other two sites may be an alternative to application of the pressure transducer by repeating our prevent underdrainage in patients with normal-pressure previous explanation that it was placed by removing the hydrocephalus. At the same time we noted the variable Delta chamber (as shown in Fig. -

The Inferior Petrosal Sinus: a Comprehensive Review with Emphasis on Clinical Implications
Childs Nerv Syst (2014) 30:831–834 DOI 10.1007/s00381-014-2378-7 REVIEW PAPER The inferior petrosal sinus: a comprehensive review with emphasis on clinical implications Martin M. Mortazavi & Christoph J. Griessenauer & Sanjay Krishnamurthy & Ketan Verma & Marios Loukas & R. Shane Tubbs Received: 1 December 2013 /Accepted: 29 January 2014 /Published online: 14 February 2014 # Springer-Verlag Berlin Heidelberg 2014 Abstract and brain stem along its course prior to emptying into the Introduction The inferior petrosal sinus is an important com- junction of the sigmoid sinus and superior jugular bulb. In the ponent of the cerebral venous system with implications in jugular foramen, the relationship of the IPS and the cranial diagnosis and treatment of a variety of diseases such as nerves is of great importance. Embryologically, the IPS de- Cushing’s disease, carotid cavernous, and dural arteriovenous velops as a new structure connecting the anterior head vein, fistulas. precursor of the cavernous sinus, and jugular bulb vesicle Methods This manuscript will review the anatomy, embryol- vein. Endovascular access to the IPS has important diagnostic ogy, and clinical implications of the inferior petrosal sinus. and therapeutic utility for a variety of conditions involving the Conclusions Knowledge of the inferior petrosal sinus is of cavernous sinus and sellar regions. This manuscript will re- great importance for open surgical approaches to the skull view the anatomy, embryology, and important clinical impli- base and endovascular access to the cavernous sinus and sellar cations of the IPS. region. Anatomy Keywords Inferior petrosal sinus . Anatomy . Skull base . Pathology The IPS (Figs. 1, 2, 3,and4) are paired venous structures at the base of the skull that drain venous blood from the cavern- ous sinus to the junction of the sigmoid sinus and the superior Introduction jugular bulb on each side. -

The Latin Language Латинский Язык
A. Z. TSISYK THE LATIN LANGUAGE ЛАТИНСКИЙ ЯЗЫК Scientia Knowledge est is potentia power Минск 2018 107 МИНИСТЕРСТВО ЗДРАВООХРАНЕНИЯ РЕСПУБЛИКИ БЕЛАРУСЬ БЕЛОРУССКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ КАФЕДРА ЛАТИНСКОГО ЯЗЫКА А.З. ЦИСЫК THE LATIN LANGUAGE ЛАТИНСКИЙ ЯЗЫК Минск 2018 108 УДК 807 (811.124) (075.8) ББК 81.2. Лат. – 923 Ре ц е н з е н т ы : кафедра иностранных языков Гродненского государственного медицинского университета (заведующий кафедрой Разводовская Я.В.); Лин С.А., доцент кафедры иностранных языков Гомельского государственного медицинского университета. Цисык А.З. Ц 73 The Latin Language / Латинский язык: учеб.-метод. пособие / А. З. Цисык. – Мн.: БГМУ, 2018. – 340 с. ISBN 985-496-063-3 Учебное пособие предназначено для иностранных студентов лечебного, педиатрического и других факультетов медицинских вузов, изучающих дисциплину «Латинский язык» на английском языке. This manual is meant for the foreign students studying in English the subject «The Latin Language» at Medical or other Faculties of Medical Universities УДК 807(811.124) (075.8) ББК 81.2.Лат. – 923 ISBN 985-496-063-3 © Цисык А.З., 2018 109 © Белорусский государственный медицинский университет, 2018 PREFACE This manual is meant for English-speaking students of medical universities of the Republic of Belarus. Its structure corresponds to the syllabus presented in the State Educational Standard Plan for the subject “The Latin Language” taught in the medical universities. The manual has been composed in accordance with generally accepted patterns expressed in well-known manuals and textbooks of Latin and Fundamentals of Medical Terminology. The manual is divided into four parts – phonetics, the anatomical part with the main grammar rules, the pharmaceutical part and the clinical one. -
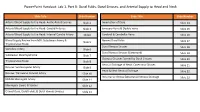
Powerpoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck
PowerPoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck Slide Title Slide Number Slide Title Slide Number Arterial Blood Supply to the Head: Aortic Arch Branches Slide 2 Innervation of Dura Slide 14 Arterial Blood Supply to the Head: Carotid Arteries Slide 3 Emissary Veins & Diploic Veins Slide 15 Arterial Blood Supply to the Head: Internal Carotid Artery Slide4 Cerebral & Cerebellar Veins Slide 16 Blood Supply Review from MSI: Subclavian Artery & Named Dural Folds Slide 5 Slide 17 Thyrocervical Trunk Dural Venous Sinuses Slide 18 Vertebral Artery Slide 6 Dural Venous Sinuses (Continued) Slide 19 Subclavian Steal Syndrome Slide 7 Osseous Grooves formed by Dural Sinuses Slide 20 Thyrocervical Trunk Slide 8 Venous Drainage of Head: Cavernous Sinuses Slide 21 Review: Suprascapular Artery Slide 9 Head & Neck Venous Drainage Slide 22 Review: Transverse Cervical Artery Slide 10 Intracranial Versus EXtracranial Venous Drainage Slide 23 Middle Meningeal Artery Slide 11 Meningeal Layers & Spaces Slide 12 Cranial Dura, Dural Folds, & Dural Venous Sinuses Slide 13 Arterial Blood Supply to the Head: Aortic Arch Branches The head and neck receive their blood supply from https://3d4medic.al/PXGmbxEt branches of the right and left common carotid and right and left subclavian arteries. • On the right side, the subclavian and common carotid arteries arise from the brachiocephalic trunk. • On the left side, these two arteries originate from the arch of the aorta. Arterial Blood Supply to the Head: Carotid Arteries On each side of the neck, the common carotid arteries ascend in the neck to the upper border of the thyroid cartilage (vertebral level C3/C4) where they divide into eXternal and internal carotid arteries at the carotid bifurcation. -

A Systematic Ultrasound Analysis of Cerebral Venous Drainage Patterns
Neuroradiology (2004) 46: 565–570 DOI 10.1007/s00234-004-1213-3 DIAGNOSTIC NEURORADIOLOGY Florian Doepp How does the blood leave the brain? Stephan J. Schreiber Thomas von Mu¨nster A systematic ultrasound analysis Jo¨rg Rademacher Randolf Klingebiel of cerebral venous drainage patterns Jose´M. Valdueza Abstract The internal jugular veins patterns were defined: a total jugular Received: 6 November 2003 Accepted: 29 March 2004 are considered to be the main path- volume flow of more than 2/3 (type Published online: 15 May 2004 ways of cerebral blood drainage. 1), between 1/3 and 2/3 (type 2) and Ó Springer-Verlag 2004 However, angiographic and less than 1/3 (type 3) of the global anatomical studies show a wide arterial blood flow. 2D TOF MR- anatomical variability and varying venography was performed exempl- This study was presented in part as an oral degrees of jugular and non-jugular arily in one subject with type-1 and presentation at the 8th Meeting of Neur- venous drainage. The study system- in two subjects with type-3 drainage. osonology and Hemodynamics, Alicante, Spain, 18–21 May 2003. atically analyses the types and prev- Type-1 drainage was present in 36 alence of human cerebral venous subjects (72%), type 2 in 11 subjects outflow patterns by ultrasound and (22%) and type 3 in 3 subjects (6%). F. Doepp (&) Æ S. J. Schreiber MRI. Fifty healthy volunteers (21 In the majority of subjects in our T. von Mu¨ nster Æ J. Rademacher J. M. Valdueza females; 29 males; mean age study population, the internal Department of Neurology, 27±7 years) were studied by color- jugular veins were indeed the main University Hospital Charite´, coded duplex sonography. -

Endovascular Approaches to the Cavernous Sinus in the Setting of Dural Arteriovenous Fistula
brain sciences Review Endovascular Approaches to the Cavernous Sinus in the Setting of Dural Arteriovenous Fistula Justin Dye 1,*, Gary Duckwiler 2, Nestor Gonzalez 3, Naoki Kaneko 2, Robert Goldberg 4, Daniel Rootman 4, Reza Jahan 2, Satoshi Tateshima 2 and Viktor Szeder 2 1 Department of Neurosurgery, Loma Linda University, Loma Linda, CA 92354, USA 2 Division of Interventional Neuroradiology, Department of Radiological Sciences, David Geffen School of Medicine, University of California, Los Angeles, CA 90095, USA; [email protected] (G.D.); [email protected] (N.K.); [email protected] (R.J.); [email protected] (S.T.); [email protected] (V.S.) 3 Department of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, CA 90048, USA; [email protected] 4 Department of Ophthalmology, David Geffen School of Medicine, University of California, Los Angeles, CA 90095, USA; [email protected] (R.G.); [email protected] (D.R.) * Correspondence: [email protected]; Tel.: +1-909-558-6338 Received: 16 July 2020; Accepted: 12 August 2020; Published: 14 August 2020 Abstract: Dural arteriovenous fistulas involving the cavernous sinus can lead to orbital pain, vision loss and, in the setting of associated cortical venous reflux, intracranial hemorrhage. The treatment of dural arteriovenous fistulas has primarily become the role of the endovascular surgeon. The venous anatomy surrounding the cavernous sinus and venous sinus thrombosis that is often associated with these fistulas contributes to the complexity of these interventions. The current report gives a detailed description of the alternate endovascular routes to the cavernous sinus based on a single center’s experience as well as a literature review supporting each approach. -

A05/2 A11 A05/2 A13
A11 A13 A05/2 A11 A05/2 A13 A05/2, A11, A13 Latin English OSSA / BONES / KNOCHEN / HUESOS / OSSOS / OS / OSSA Cranium /Skull / Schädel / Cráneo / Crânio / Crâne / Cranio A05/2, A11, A13: A05/2, A11, A13: 1 Diploe 1 Diploe 2 Clivus 2 Clivus 3 Fossa temporalis 3 Temporal fossa 4 Arcus zygomaticus 4 Zygomatic arch 5 Fossa infratemporalis 5 Infratemporal fossa 6 Fossa pterygopalatina 6 Pterygopalatine fossa 7 Foramen jugulare 7 Jugular foramen 8 Foramen Iacerum 8 Foramen lacerum 9 Foramen palatinum majus 9 Greater palatine foramen 10 Fossa incisiva 10 Incisive fossa 11 Canalis incisivi 11 Incisive canals 12 Septum nasi osseum 12 Bony nasal septum 13 Apertura piriformis 13 Piriform aperture 14 Concha nasalis media 14 Middle nasal concha 15 Foramen ethmoidale anterius 15 Anterior ethmoidal foramen 16 Foramen ethmoidale posterius 16 Posterior ethmoidal foramen 17 Fossa sacci Iacrimalis 17 Fossa for lacrimal sac 18 Fissura orbitalis superior 18 Superior orbital® fissure 19 Fissura orbitalis inferior 19 Inferior orbital fissure 20 Os occipitale 20 Occipital bone 21 Foramen magnum 21 Foramen magnum 22 Sulcus sinus petrosi inferioris 22 Groove for inferior petrosal sinus 23 Tuberculum pharyngeum 23 Pharyngeal tubercle 24 Squama occipitalis 24 Squamous part of occipital bone 25 Condylus occipitalis 25 Occipital condyle 26 Canalis condylaris 26 Condylar canal 27 Canalis nervi hypoglossi 27 Hypoglossal canal 28 Incisura jugularis 28 Jugular notch 29 Protuberantia occipitalis externa 29 External occipital protuberance 30 Linea nuchalis suprema 30 Highest