The Effect of Aerobic Exercise on the Number of Migraine Days, Duration
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mothers Grimm Kindle
MOTHERS GRIMM PDF, EPUB, EBOOK Danielle Wood | 224 pages | 01 Oct 2016 | Allen & Unwin | 9781741756746 | English | St Leonards, Australia Mothers Grimm PDF Book Showing An aquatic reptilian-like creature that is an exceptional swimmer. They have a temper that they control and release to become effective killers, particularly when a matter involves a family member or loved one. She took Nick to Weston's car and told Nick that he knew Adalind was upstairs with Renard, and the two guys Weston sent around back knew too. When Wu asks how she got over thinking it was real, she tells him that it didn't matter whether it was real, what mattered was losing her fear of it. Dick Award Nominee I found the characters appealing, and the plot intriguing. This wesen is portrayed as the mythological basis for the Three Little Pigs. The tales are very dark, and while the central theme is motherhood, the stories are truly about womanhood, and society's unrealistic and unfair expectations of all of us. Paperback , pages. The series presents them as the mythological basis for The Story of the Three Bears. In a phone call, his parents called him Monroe, seeming to indicate that it is his first name. The first edition contained 86 stories, and by the seventh edition in , had unique fairy tales. Danielle is currently teaching creative writing at the University of Tasmania. The kiss of a musai secretes a psychotropic substance that causes obsessive infatuation. View all 3 comments. He asks Sean Renard, a police captain, to endorse him so he would be elected for the mayor position. -

The Open Notebook’S Pitch Database Includes Dozens of Successful Pitch Letters for Science Stories
Selected Readings Prepared for the AAAS Mass Media Science & Engineering Fellows, May 2012 All contents are copyrighted and may not be used without permission. Table of Contents INTRODUCTION PART ONE: FINDING IDEAS 1. Lost and found: How great non-fiction writers discover great ideas—In this topical feature, TON guest contributor Brendan Borrell interviews numerous science writers about how they find ideas. (The short answer: In the darndest places.) 2. Ask TON: Saving string—Writers and editors provide advice on gathering ideas for feature stories. 3. Ask TON: From idea to story—Four experienced science writers share the questions they ask themselves when weighing whether a story idea is viable. 4. Ask TON: Finding international stories—Six well-traveled science writers share their methods for sussing out international stories. PART TWO: PITCHING 5. Ask TON: How to pitch—In this interview, writers and editors dispense advice on elements of a good pitch letter. 6. Douglas Fox recounts an Antarctic adventure—Doug Fox pitched his Antarctica story to numerous magazines, unsuccessfully, before finding a taker just before leaving on the expedition he had committed to months before. After returning home, that assignment fell through, and Fox pitched it one more time—to Discover, who bought the story. In this interview, Fox describes the lessons he learned in the pitching process; he also shares his pitch letters, both unsuccessful and successful (see links). 7. Pitching errors: How not to pitch—In this topical feature, Smithsonian editor Laura Helmuth conducts a roundtable conversation with six other editors in which they discuss how NOT to pitch. -

The Complete Stories
The Complete Stories by Franz Kafka a.b.e-book v3.0 / Notes at the end Back Cover : "An important book, valuable in itself and absolutely fascinating. The stories are dreamlike, allegorical, symbolic, parabolic, grotesque, ritualistic, nasty, lucent, extremely personal, ghoulishly detached, exquisitely comic. numinous and prophetic." -- New York Times "The Complete Stories is an encyclopedia of our insecurities and our brave attempts to oppose them." -- Anatole Broyard Franz Kafka wrote continuously and furiously throughout his short and intensely lived life, but only allowed a fraction of his work to be published during his lifetime. Shortly before his death at the age of forty, he instructed Max Brod, his friend and literary executor, to burn all his remaining works of fiction. Fortunately, Brod disobeyed. Page 1 The Complete Stories brings together all of Kafka's stories, from the classic tales such as "The Metamorphosis," "In the Penal Colony" and "The Hunger Artist" to less-known, shorter pieces and fragments Brod released after Kafka's death; with the exception of his three novels, the whole of Kafka's narrative work is included in this volume. The remarkable depth and breadth of his brilliant and probing imagination become even more evident when these stories are seen as a whole. This edition also features a fascinating introduction by John Updike, a chronology of Kafka's life, and a selected bibliography of critical writings about Kafka. Copyright © 1971 by Schocken Books Inc. All rights reserved under International and Pan-American Copyright Conventions. Published in the United States by Schocken Books Inc., New York. Distributed by Pantheon Books, a division of Random House, Inc., New York. -

Headache and Comorbidities in Childhood and Adolescence Headache
Headache Series Editor: Paolo Martelletti Vincenzo Guidetti Marco A. Arruda Aynur Ozge Editors Headache and Comorbidities in Childhood and Adolescence Headache Series Editor Paolo Martelletti Roma, Italy [email protected] The purpose of this Series, endorsed by the European Headache Federation (EHF), is to describe in detail all aspects of headache disorders that are of importance in primary care and the hospital setting, including pathophysiology, diagnosis, management, comorbidities, and issues in particular patient groups. A key feature of the Series is its multidisciplinary approach, and it will have wide appeal to internists, rheumatologists, neurologists, pain doctors, general practitioners, primary care givers, and pediatricians. Readers will find that the Series assists not only in understanding, recognizing, and treating the primary headache disorders, but also in identifying the potentially dangerous underlying causes of secondary headache disorders and avoiding mismanagement and overuse of medications for acute headache, which are major risk factors for disease aggravation. Each volume is designed to meet the needs of both more experienced professionals and medical students, residents, and trainees. More information about this series at http://www.springer.com/series/11801 [email protected] Vincenzo Guidetti • Marco A. Arruda Aynur Ozge Editors Headache and Comorbidities in Childhood and Adolescence [email protected] Editors Vincenzo Guidetti Marco A. Arruda Child and Adolescent Neuropsychiatry University of São Paulo Sapienza University Neuropsychiatry, Glia Institute Rome Ribeirão Preto Italy Brazil Aynur Ozge Neurology, Algology and Clinical Neurophysiology Mersin University School of Medicine Mersin, Adana Turkey ISSN 2197-652X ISSN 2197-6538 (electronic) Headache ISBN 978-3-319-54725-1 ISBN 978-3-319-54726-8 (eBook) DOI 10.1007/978-3-319-54726-8 Library of Congress Control Number: 2017947346 © Springer International Publishing AG 2017 This work is subject to copyright. -

Sympathy for the Devil: Volatile Masculinities in Recent German and American Literatures
Sympathy for the Devil: Volatile Masculinities in Recent German and American Literatures by Mary L. Knight Department of German Duke University Date:_____March 1, 2011______ Approved: ___________________________ William Collins Donahue, Supervisor ___________________________ Matthew Cohen ___________________________ Jochen Vogt ___________________________ Jakob Norberg Dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of German in the Graduate School of Duke University 2011 ABSTRACT Sympathy for the Devil: Volatile Masculinities in Recent German and American Literatures by Mary L. Knight Department of German Duke University Date:_____March 1, 2011_______ Approved: ___________________________ William Collins Donahue, Supervisor ___________________________ Matthew Cohen ___________________________ Jochen Vogt ___________________________ Jakob Norberg An abstract of a dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of German in the Graduate School of Duke University 2011 Copyright by Mary L. Knight 2011 Abstract This study investigates how an ambivalence surrounding men and masculinity has been expressed and exploited in Pop literature since the late 1980s, focusing on works by German-speaking authors Christian Kracht and Benjamin Lebert and American author Bret Easton Ellis. I compare works from the United States with German and Swiss novels in an attempt to reveal the scope – as well as the national particularities – of these troubled gender identities and what it means in the context of recent debates about a “crisis” in masculinity in Western societies. My comparative work will also highlight the ways in which these particular literatures and cultures intersect, invade, and influence each other. In this examination, I demonstrate the complexity and success of the critical projects subsumed in the works of three authors too often underestimated by intellectual communities. -
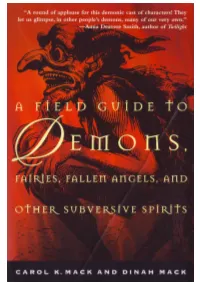
A-Field-Guide-To-Demons-By-Carol-K
A FIELD GUIDE TO DEMONS, FAIRIES, FALLEN ANGELS, AND OTHER SUBVERSIVE SPIRITS A FIELD GUIDE TO DEMONS, FAIRIES, FALLEN ANGELS, AND OTHER SUBVERSIVE SPIRITS CAROL K. MACK AND DINAH MACK AN OWL BOOK HENRY HOLT AND COMPANY NEW YORK Owl Books Henry Holt and Company, LLC Publishers since 1866 175 Fifth Avenue New York, New York 10010 www.henryholt.com An Owl Book® and ® are registered trademarks of Henry Holt and Company, LLC. Copyright © 1998 by Carol K. Mack and Dinah Mack All rights reserved. Distributed in Canada by H. B. Fenn and Company Ltd. Library of Congress-in-Publication Data Mack, Carol K. A field guide to demons, fairies, fallen angels, and other subversive spirits / Carol K. Mack and Dinah Mack—1st Owl books ed. p. cm. "An Owl book." Includes bibliographical references and index. ISBN-13: 978-0-8050-6270-0 ISBN-10: 0-8050-6270-X 1. Demonology. 2. Fairies. I. Mack, Dinah. II. Title. BF1531.M26 1998 99-20481 133.4'2—dc21 CIP Henry Holt books are available for special promotions and premiums. For details contact: Director, Special Markets. First published in hardcover in 1998 by Arcade Publishing, Inc., New York First Owl Books Edition 1999 Designed by Sean McDonald Printed in the United States of America 13 15 17 18 16 14 This book is dedicated to Eliza, may she always be surrounded by love, joy and compassion, the demon vanquishers. Willingly I too say, Hail! to the unknown awful powers which transcend the ken of the understanding. And the attraction which this topic has had for me and which induces me to unfold its parts before you is precisely because I think the numberless forms in which this superstition has reappeared in every time and in every people indicates the inextinguish- ableness of wonder in man; betrays his conviction that behind all your explanations is a vast and potent and living Nature, inexhaustible and sublime, which you cannot explain. -

Kinsella Feb 13
MORPHEUS: A BILDUNGSROMAN A PARTIALLY BACK-ENGINEERED AND RECONSTRUCTED NOVEL MORPHEUS: A BILDUNGSROMAN A PARTIALLY BACK-ENGINEERED AND RECONSTRUCTED NOVEL JOHN KINSELLA B L A Z E V O X [ B O O K S ] Buffalo, New York Morpheus: a Bildungsroman by John Kinsella Copyright © 2013 Published by BlazeVOX [books] All rights reserved. No part of this book may be reproduced without the publisher’s written permission, except for brief quotations in reviews. Printed in the United States of America Interior design and typesetting by Geoffrey Gatza First Edition ISBN: 978-1-60964-125-2 Library of Congress Control Number: 2012950114 BlazeVOX [books] 131 Euclid Ave Kenmore, NY 14217 [email protected] publisher of weird little books BlazeVOX [ books ] blazevox.org 21 20 19 18 17 16 15 14 13 12 01 02 03 04 05 06 07 08 09 10 B l a z e V O X trip, trip to a dream dragon hide your wings in a ghost tower sails crackling at ev’ry plate we break cracked by scattered needles from Syd Barrett’s “Octopus” Table of Contents Introduction: Forging the Unimaginable: The Paradoxes of Morpheus by Nicholas Birns ........................................................ 11 Author’s Preface to Morpheus: a Bildungsroman ...................................................... 19 Pre-Paradigm .................................................................................................. 27 from Metamorphosis Book XI (lines 592-676); Ovid ......................................... 31 Building, Night ...................................................................................................... -

2009 Princeton Summer Journal
HARRY POTTER RETURNS | 4 NO BREAK FOR SUMMER THEATER | 7 DUCKS QUACK UNDER PRESSURE | 12 The Princeton ummer J ournal sA Publication of The Princeton University Summer Journalism Program Monday, August 10, 2009 Founded in 2002 princeton.edu/sjp Sotomayor sworn in as justice Princetonian is first Hispanic and By Melissa Sanchez only third woman onMORE Supreme COVERAGE Court queens,Sealing n.y. a contentious con- Latino heritage shaped firmation that nonetheless college years | 2 had been viewed by most as Alumna’s life parallels a fait accompli, the Senate voted Thursday to make So- senior thesis subject, nia Sotomayor ’76 the next Puerto Rican hero Luis associate justice of the U.S. Muñoz Marín | 2 BRIAN ROKUS :: THE PRINCETON SUMMER JOURNAL Supreme Court. Jane De La Cruz, who works at Witherspoon Bread Company, does not have health insurance because it would cost much of her paycheck, she said. On Saturday, in the first swearing in of a new justice with her, because she is so ever to be televised, Sotomay- gracious and so open to every- or became the first Hispanic one,” Rivera said. justice and only the third In May, President Obama woman to serve on the High nominated Sotomayor to suc- Court. She is also the first ceed Justice David Souter. justice to be nominated by a The choice set off a series of Democratic president in 15 heated debates over Sotomay- years. or’s experience, qualifications “We are proud and de- and judicial philosophy. lighted,” University Presi- In particular, Republicans dent Shirley Tilghman said cited comments Sotomayor As debate rages nationwide,By Jay Kim :: local businesses grapple with in a statement. -

The Hermit in German Literature COLLEGE of ARTS and SCIENCES Imunci Germanic and Slavic Languages and Literatures
The Hermit in German Literature COLLEGE OF ARTS AND SCIENCES ImUNCI Germanic and Slavic Languages and Literatures From 1949 to 2004, UNC Press and the UNC Department of Germanic & Slavic Languages and Literatures published the UNC Studies in the Germanic Languages and Literatures series. Monographs, anthologies, and critical editions in the series covered an array of topics including medieval and modern literature, theater, linguistics, philology, onomastics, and the history of ideas. Through the generous support of the National Endowment for the Humanities and the Andrew W. Mellon Foundation, books in the series have been reissued in new paperback and open access digital editions. For a complete list of books visit www.uncpress.org. The Hermit in German Literature From Lessing to Eichendorff henry john fitzell UNC Studies in the Germanic Languages and Literatures Number 30 Copyright © 1961 This work is licensed under a Creative Commons cc by-nc-nd license. To view a copy of the license, visit http://creativecommons. org/licenses. Suggested citation: Fitzell, Henry John. The Hermit in German Litera- ture: From Lessing to Eichendorff. Chapel Hill: University of North Car- olina Press, 1961. doi: https://doi.org/10.5149/9781469657493_Fitzell Library of Congress Cataloging-in-Publication Data Names: Fitzell, Henry John. Title: The hermit in German literature : From Lessing to Eichendorff / by Henry John Fitzell. Other titles: University of North Carolina Studies in the Germanic Languages and Literatures ; no. 30. Description: Chapel Hill : University of North Carolina Press, [1961] Series: University of North Carolina Studies in the Germanic Languages and Literatures. | Includes bibliographical references. Identifiers: lccn 61064190 | isbn 978-0-8078-8830-8 (pbk: alk. -
Legislature Seeking TVA Negotiation
FRIDAY 160th yEar • no. 299 aPriL 17, 2015 cLEVELand, Tn 22 PaGES • 50¢ Bulletin Legislature seeking TVA negotiation Special Olympics postponed due to wet conditions Ocoee River’s whitewater rafting future is targeted According to the document, the U.S. tination.” From Staff Reports By BRIAN GRAVES Banner Staff Writer Congress passed legislation in 1983 to provide “By passing SJR166 unanimously, the Due to wet field conditions “recreational water releases” from the Ocoee Tennessee General Assembly recognizes the in Benny Monroe Stadium, The Tennessee General Assembly has unan- No. 2 power project and enabled a contract vital impact the Ocoee River and the rafting the 33rd annual Special imously passed a joint resolution asking action between the state and TVA to provide reliable industry has on the economy of Polk County Olympics has been post- by TVA, the state and the U.S. Congress to be releases for 116 days per year. and Southeast Tennessee,” Bell told the poned to Saturday, April 25. taken to maintain “reliable water releases” That contract will expire in March 2019 with Cleveland Daily Banner. “I hope the TVA board Starting time will remain 9 along the Ocoee River. the last recreational release for rafting occur- of directors and our congressional delegation a.m. State Sen. Mike Bell, R-Riceville, introduced ring in October 2018. realize how important settling the water The popular annual event the measure and state Rep. Dan Howell, R- The resolution says the Legislature supports release issue is to our rafting businesses and Georgetown, is expressing concern the agency actions that will maintain the Ocoee’s status was supposed to have been Howell held Saturday (tomorrow). -

A Critical Ethnography of the Myrtles Plantation in St. Francisville, Louisiana with Ruminations on Hauntology
Louisiana State University LSU Digital Commons LSU Doctoral Dissertations Graduate School 2012 A critical ethnography of The yM rtles Plantation in St. Francisville, Louisiana with ruminations on hauntology Holley Ann Vaughn Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_dissertations Part of the Communication Commons Recommended Citation Vaughn, Holley Ann, "A critical ethnography of The yM rtles Plantation in St. Francisville, Louisiana with ruminations on hauntology" (2012). LSU Doctoral Dissertations. 3317. https://digitalcommons.lsu.edu/gradschool_dissertations/3317 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Doctoral Dissertations by an authorized graduate school editor of LSU Digital Commons. For more information, please [email protected]. A CRITICAL ETHNOGRAPHY OF THE MYRTLES PLANTATION IN ST. FRANCISVILLE, LOUISIANA WITH RUMINATIONS ON HAUNTOLOGY A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College In partial fulfillment of the Requirements of the degree of Doctor of Philosophy in The Department of Communication Studies by Holley Ann Vaughn B.A., University of North Texas, 2001 M.A., University of North Texas, 2005 December 2012 ACKNOWLEDGMENTS This project could not have come to fruition without the time, love, commitment and dedication of so many of my friends, family, mentors and colleagues. To my huge, loving family, particularly my parents Devora Vaughn, Greg Vaughn, and Carolyn Vaughn, thank you for your support, patience and constant encouragement. To my aunt and uncle Rhonda and Ed King, thank you for taking me in, opening your home, and providing a space to cocoon and grow. -

The Malleus Maleficarum
broedel.cov 12/8/03 9:23 am Page 1 ‘Broedel has provided an excellent study, not only of the Malleus and its authors, and the construction of witchcraft The Malleus Maleficarum but just as importantly, of the intellectual context in which the Malleus must be set and the theological and folk traditions to which it is, in many ways, an heir.’ and the construction of witchcraft PETER MAXWELL-STUART, ST ANDREWS UNIVERSITY Theology and popular belief HAT WAS WITCHCRAFT? Were witches real? How should witches The HANS PETER BROEDEL be identified? How should they be judged? Towards the end of the middle ages these were serious and important questions – and completely W Malleus Maleficarum new ones. Between 1430 and 1500, a number of learned ‘witch-theorists’ attempted to answer such questions, and of these perhaps the most famous are the Dominican inquisitors Heinrich Institoris and Jacob Sprenger, the authors of the Malleus Maleficarum, or The Hammer of Witches. The Malleus is an important text and is frequently quoted by authors across a wide range of scholarly disciplines.Yet it also presents serious difficulties: it is difficult to understand out of context, and is not generally representative of late medieval learned thinking. This, the first book-length study of the original text in English, provides students and scholars with an introduction to this controversial work and to the conceptual world of its authors. Like all witch-theorists, Institoris and Sprenger constructed their witch out of a constellation of pre-existing popular beliefs and learned traditions. BROEDEL Therefore, to understand the Malleus, one must also understand the contemporary and subsequent debates over the reality and nature of witches.