Denver Health Doctoral Psychology Internship Program Brochure and Policies December 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
What Are Reasonable Expectations For
Beyond Evidence-Based Psychotherapy RT21601_C000.indd i 9/5/08 7:29:11 AM COUNSELING AND PSYCHOTHERAPY: INVESTIGATING PRACTICE FROM SCIENTIFIC, HISTORICAL, AND CULTURAL PERSPECTIVES A Routledge book series Editor, Bruce E. Wampold, University of Wisconsin Th is innovative new series is devoted to grasping the vast complexities of the practice of coun- seling and psychotherapy. As a set of healing practices delivered in a context shaped by health delivery systems and the attitudes and values of consumers, practitioners, and researchers, counseling and psychotherapy must be examined critically. By understanding the historical and cultural context of counseling and psychotherapy and by examining the extant research, these critical inquiries seek a deeper, richer understanding of what is a remarkably eff ective endeavor. Published Counseling and Th erapy With Clients Who Abuse Alcohol or Other Drugs Cynthia E. Glidden-Tracy Th e Great Psychotherapy Debate Bruce Wampold Th e Psychology of Working: Implications for Career Development, Counseling, and Public Policy David Blustein Neuropsychotherapy: How the Neurosciences Inform Eff ective Psychotherapy Klaus Grawe Principles of Multicultural Counseling Uwe P. Gielen, Juris G. Draguns, Jeff erson M. Fish Cognitive-Behavioral Th erapy for Deaf and Hearing Persons With Language and Learning Challenges Neil Glickman Forthcoming Th e Pharmacology and Treatment of Substance Abuse: Evidence and Outcomes Based Perspective Lee Cohen, Frank Collins, Alice Young, Dennis McChargue Making Treatment Count: Using Outcomes to Inform and Manage Th erapy Michael Lambert, Jeb Brown, Scott Miller, Bruce Wampold Th e Handbook of Th erapeutic Assessment Stephen E. Finn IDM Supervision: An Integrated Developmental Model for Supervising Counselors and Th era- pists, Th ird Edition Cal Stoltenberg and Brian McNeill Th e Great Psychotherapy Debate, Revised Edition Bruce Wampold Casebook for Multicultural Counseling Miguel E. -

John Steel, Artist of the Underwater World
Historical Diver, Number 19, 1999 Item Type monograph Publisher Historical Diving Society U.S.A. Download date 23/09/2021 12:48:50 Link to Item http://hdl.handle.net/1834/30862 NUMBER 19 SPRING 1999 John Steel, Artist of the Underwater World Salvage Man - The Career of Edward Ellsberg • Sicard's 1853 Scuba Apparatus Underwater Photography 1935 • Lambertsen Gas Saver Unit • Lang Helmet • NOGI Awards ADC Awards • D.E.M.A. Awards • Carol Ann Merker • Beneath the Sea Show HISTORICAL DIVING SOCIETY USA A PUBLIC BENEFIT NON-PROFIT CORPORATION PMB 405 2022 CLIFF DRIVE SANTA BARBARA, CALIFORNIA 93109-1506, U.S.A. PHONE: 805-692-0072 FAX: 805-692-0042 e-mail: [email protected] or HTTP://WWW.hds.org/ ADVISORY BOARD CORPORATE MEMBERS Dr. Sylvia Earle Lotte Hass DIVERS ALERT NETWORK Dr. Peter B. Bennett Dick Long STOLT COMEX SEAWAY Dick Bonin J. Thomas Millington, M.D. OCEAN FUTURES Scott Carpenter Bob & Bill Meistrell OCEANIC DIVING SYSTEMS INTERNATIONAL Jean-Michel Cousteau Bev Morgan D.E.S.C.O. E.R. Cross Phil Nuytten SCUBA TECHNOLOGIES, INC. Andre Galerne Sir John Rawlins DIVE COMMERCIAL INTERNATIONAL, INC. Lad Handelman Andreas B. Rechnitzer, Ph.D. MARES Prof. Hans Hass Sidney J. Smith SEA PEARLS CALDWELL'S DIVING CO. INC. Les Ashton Smith OCEANEERING INTL. INC. WEST COAST SOCIETY BOARD OF DIRECTORS DRS MARINE, INC. Chairman: Lee Selisky, President: Leslie Leaney, Secretary: AQUA-LUNG James Forte, Treasurer: Blair Mott, Directors: Bonnie W.J. CASTLE P.E. & ASSOC.P.C. Cardone, Angela Tripp, Captain Paul Linaweaver, M.D., MARINE SURPLUS SUPPLY BEST PUBLISHING U.S.N. -
General Semantics Bulletin
General Semantics Bulletin Yearbook of the Institute of General Semantics Number 71, Membership Year 2004 Fort Worth, TX Honorary Trustees, 1940 Executive Director APPOINTED BY ALFRED KORZYBSKI Steve Stockdale Gaston Bachelard Maxim Bing Assistant Executive Director Abraham A. Brill Jennifer Carmack W. Burridge Ross McC. Chapman, George E. Coghill Arthur Stone Dewing Board of Trustees Franklin C. Ebaugh Officers P. H. Esser President, Andrea Johnson David Fairchild Vice President, Irene S. Ross Mayper Clarence B. Farrar Treasurer, Lynn Schuldt William Healy Lancelot Hogben Secretary, Susan Presby Kodish Earnest A. Hooten Recording Secretary, Robert R. Potter Smith Ely Jelliffe Edward Kasner Board Members Cassius J. Keyser George J. Barenholtz Nolan D. C. Lewis Sanford I. Berman Ralph S. Lillie Laura Bertone Bronislaw Malinowski Walter W. Davis Raymond W. McNealy Milton Dawes Adolf Meyer Allen Flagg Winfred Overholser James Douglas French Stewart Paton Raymond Pearl Gregg Hoffmann William F. Petersen Bruce Kodish Roscoe Pound Susan Presby Kodish George S. Stevenson Martin Levinson M. Tramer Harry Maynard Walter L. Treadway Jeffrey A. Mordkowitz Richard Weil, Jr. Gerard I. Nierenberg George K. Zipf Frank Scardilli Honorary Trustees APPOINTED 1963 AND SINCE Robert Blake, Joseph Brewer, Douglas G. Campbell, Hadley Cantril, Stuart Carter Dodd, R. Buckminster Fuller, Henri Laborit, Abraham Maslow, Myres S. McDougall, Joost A. M. Meerloo, Russell Meyers, E. DeAlton Partridge, Allen Walker Read, J. Gordon Roberts, F. J. Roethlisberger, Jesse H. Shera, Alvin M. Weinberg © Institute of General Semantics The Scientific Philosophy of General Semantics General Semantics (GS) qualifies as an unusual, tough- to-‘pin down’, interdisciplinary field. “Is it a science or a philosophy?” Perhaps GS may best be seen as neither ‘science’ nor ‘philosophy’ but rather as both/and––a scientific philosophy applicable moreover to the life concerns of ‘the man and woman in the street’. -

Red Ban Egiste Section One
RED BAN EGISTE SECTION ONE VOLUME LXIV, NO. i. RED BANK, N. J., THURSDAY, JUNE 26, 1941. PAGES! TO 16 Supper Tonight At 700 DogsEntered In Reformed Church Big Sailing Regatta $1,600 Cleared For Second Registration The second annual supper served Child Welfare by the ladles of the Red Bank Re- formed church on Shrewsbury ave- Mrs. Lewis S. Thompson, Jr., Annual Rumson Sfiow nue, will take place in the churoh On Fourth Of July of Brookdale farm, Llncroft, For Draft Next Tuesday 1 notified The Register Tuesday dining room tonight. Supper will be that there had been 1,100 paid served from 0:30 o'clock and will admissions at the annual Social consist of ham and all ths fixings. Service pet show, and that the Event Saturday At Rumson To The ohalnnan in charge of the af- Inter-Club Races Feature gross receipts totaled. $1,861.94. Instructions Issued By Re'd Bantc fair is Mrs. Wallace B. Ronkln. She She said that approximately Feature Water Test Exhibition will be assisted by tho following com- Event* On M. B. C. Program $1,600 had been cleared for child Board—Expect 15d to Register Here mlttees: Kitchen committee, Un. welfare work. John Weller chairman, Mrs. Eliza- An -unusual "water test" exhibition beth Estelle, Mrs. Victor Hembllng, Arrow and lightning class boats, She was especially apprecia- Instructions for the second draft will be one of the interesting fea- Mrs. Rusiel Clark, Mrs. H«It3r"£i- knockabouts, comets, sneakboxes, tive of the co-operation received registration for military service neat tures of the 13th annual dog show of Joseph Serpico telle and Mm. -

Dragon Magazine #102
D RAGON 1 12 20 SPECIAL ATTRACTION 43 Valley of the Earth Mother Designed by Lise Breakey An AD&D® game adventure for 4th-6th level player characters 43 Publisher Mike Cook Editor-in-Chief Kim Mohan OTHER FEATURES Editorial staff 8 Realms of role playing Gary Gygax Patrick Lucien Price In favor of a different style of gaming: less acting and more action Roger Moore Art director and graphics 12 All about the gully dwarf Roger E. Moore Roger Raupp The lowest rung on Krynns demi-human totem pole Subscriptions 20 A collection of canines Stephen Inniss Irene Swan Changes and additions to the AD&D worlds roster of dogdom Advertising Mary Parkinson 30 Nine wands of wonder Ed Greenwood Distinctive new magic items from the Realms Contributing editors Ed Greenwood 38 Now thats firepower! Desmond P. Varady Katharine Kerr Machine guns and missile launchers for TOP SECRET® play This issues contributing artists Dean Morrissey 56 Creating a cast of NPCs Jim Dutton Larry Elmore How to populate your campaign world quickly and coherently Bob Maurus Roger Raupp 58 Passing in the Night Rob Chilson Jim Holloway A story of combat in outer space with an unseen enemy Marvel Bullpen David Trampier Joseph Pillsbury Richard Tomasic Lance Foster Edward Wagner DEPARTMENTS 3 Letters 86 Convention calendar 92 Dragonmirth 4 World Gamers Guide 88 Gamers Guide 94 Snarfquest 6 The forum 90 Wormy COVER The Pillage of Tantlin is another in a long line of paintings weve published that illustrate the imagination and artistic skill of Dean Morrissey, whos being doing art- work for us since these gnomes were knee-high to a kobold. -

Open ., C, •• D David Ferrier Was Another New Orleans District Attorney Orate the Condition Which TNC Ex-S
VOLUME 5, ISSUE 5 University of California, San Diego NOVEMBER 1, 1968 John Muir Reagan Won't Editor's Note: Government The following is the text of a letter sent to all the members of the Board of Regents, as well as the Chancellors of the UC campuses. The indented paragraph was sent to Governor Reagan on Tuesday Underway by telegram. H e responded yesterday, stating that he would be A viable Muir College govern glad to meet with student representatives, but not on state-wide mentwill soon be formed follow television, since this, he felt, would not serve any purpose. ing a year of frustration if plans now under way are successful. The Regents of the University of California have been the target Government at Muir College of criticism by both the students of the University and the Governor began on October 16 of last year of the state. As the elected representatives of the students of the when a group of interested stu University of California, we are deeply concerned about thiS and dents called a meeting of 20 other problems which now threaten the university. We also recog delegates - 2 from each of the nize that conflicting and therefore confusing explanations of the dorms and 4 selected from among causes of these problems have led to minunderstanding among both the commuters. the students and the general public. With the hope of improving The gu iding philosophy ofthose communications and clearing up some of the m!sunderstandingsbetween students was that the traditional the university students and the people of California, we make the form of student government was following proposal: irrelevant because it could only The elected representatives of the students of the Unive rsity do student activities - it could A HALLOW.EEN SURPRISE from the GREAT PUMP.KIN !! of California invite Governor Reagan to discuss, on state-wide not direct the total college life. -

The Future of Music Production Is Here, Now... 2 Contents
The Future of Music Production Is Here, Now... 2 Contents Foreword ...................................................................................... 4 The Leadership Team ................................................................ 6 Spotlight On: The Leadership Team (Production) ....................... 8 Interview With Marwan PKA King Tut ......................................... 10 Meet The Production School Team .............................................. 12 Production Tutors ....................................................................... 13 Spotlight On: The Role Of The Modern Producer ......................... 16 Spotlight On: What Will You Learn? ............................................. 19 Spotlight On: Electives For Producers ...................................... 20 Deconstruction Of A Final Production ......................................... 22 Anatomy Of A Successful Producer ............................................ 23 Spotlight On: Cross-Pathway Business Education ..................... 24 Spotlight On: Brands .................................................................. 26 Spotlight On: Podcasts ............................................................... 27 Spotlight On: Musical Directors ................................................. 29 Spotlight On: Arrangement ....................................................... 31 Spotlight On: Production Career Opportunities ........................ 41 Spotlight On: Metropolis ............................................................ 34 Message -
1997 Fall.Pdf
BOARD OF TRUSTEES PRINCETON DAY SCHOOL JOURNAL Daniel J. Graziano, Jr., Chairman Volume 34, Number 2 Fall 1997 Peter G. Gerry, Vice Chairman Randall A. Hack, Treasurer Christine Grant Halpern, Secretary/Parliamentarian Stephanie J. Briody Features Shawn W. Ellsworth '75 Thomas R. Gates '78 John L. Griffith, Jr. Imagine the Possibilities Marilyn W. Grounds Brooke R. Gunn Students from junior kindergarten through Aaron Lemonick twelfth grade learn from visiting writers and Lila B. Lohr illustrators. Deborah Sze Modzelewski John A. Pinto Jack Z. Rabinowitz Deepak D. Raj Robert A. Revelle Llewellyn G. Ross 2 Alison M. Shehadi Jane Aresty Silverman '63 Live - From Lincoln Center! Robert B. Stockman The performing arts come to life as students Penny Thomas participate in workshops with artists from John D. Wallace '48 James W . Wickenden Lincoln Center Institute. Elizabeth C. Dilworth, Trustee Emerita Betty Wold Johnson, Trustee Emerita Samuel W . Lambert III, Trustee Emeritus ALUMNI COUNCIL Thomas R. Gates '78, President 5 Laura Farina '79, Vice President Markell Meyers Shriver '46, Secretary/Treasurer Christina Bachelder Dufresne '77, Ex Officio Pretty Brook Farm Garden Blooms Again Amy Venable Ciuffreda '88 Lower schoolers revive garden first planted by Dean Thomas Foster '85 Caroline Erdman Hare '75 Mathey 70 years ago. Jamie Phares Jacobson '80 Michael Mantell '76 Harry Rulon-Miller '51 Robert H. Olsson '78 Imaginative Programs Bring Leslie Pell Linneman '82 Summer Students to Campus Karen Turner '72 Find out what PDS does on its On the cover: Pumpkin Pride: Showing o ff summer "vacation.” vegetables they grew in the Pretty Brook Farm garden are (standing) Am elia Baxter- Stoltzfus 06, Giovanna Torchio ’98, Casey Unterman ’99, David Blitzer ’06, (sitting) Rachel Bergenfield ’06, Chris Baker ’06, Departments Phoebe Stockman 06, Becky Stanko 06, Bright Lim m ’98, Andrew Davidson ’06. -

WHO's WHO in POP LP ENGINEERING the Following Is a List of ENGINEERS Credited on at Least One Album in the Top Pop 100 Charts from January 1998 to the Present
WHO'S WHO IN POP LP ENGINEERING The following is a list of ENGINEERS credited on at least one album in the Top Pop 100 Charts from January 1998 to the present.. (Please note that, due to computer restraints, ENGINEERS are NOT credited on an album that has more than 4 ENGINEERS listed)) This listing includes the ENGINEER'S Name (# of records credited) "Album Title" - Artist/ Other ENGINEERS credited on the record. 4th Disciple(1) - 'Heavy Mental'- Killah Priest-/Troy Hightower Bob Power 4th Disciple Alan Douglaa(1) - "Pilgrim"-Eric Clapton-/ Dave Aaron(i) - "40 Dayz & 40 Nightz"- XzibitVRichard 'Segal' Huredia Greg Droman(l) - "I Don't Want To Miss A Thing'-Mark Chesnutt-/ Josh Abrams(1) - "Something For Everybody"-Baz Luhrmann-/ Michael Dumas(1) - "A Long Way Home'-Dwight Yoakam-/ Dusty Wakeman David Leonard Conley Abrams 111(1) - "Let's Ride'-Montell Jordan-/Annie Mae Catalino Claude Achille Kevin Davis Charles Dye(2) - "Growing Pains'-Billie Myers-/ Michael Brauer Greg Calbi + "Red Voodoo" -Sammy Claude Achille(1) - "Let's Ride'-Montell JordanVAnnie Mae Catalino Kevin Davis Hagar-/Toby Wright Tom McWilliams Brian Ackley(l) - "The Christmas Angel"- Mannheim Steamroller-/ Dave Cwirko Dan Charette Jim Ebert(1) - "Blurring The Edges'-Meredith BrooksVGeza X John Agnello(1) - "Wide Swing Tremolo"- Son VolWDavid Barbe Jack Joseph Puig Brett EliasonM) - "Live On Two Legs'- Pearl Jam-/ John Aguto(1) - "Still In The Game'-Keith SweatVKarl Heilbron Kevin 'KD' Davis Geoff Emerick(1) - "Vertical Man'-Ringo Starr-/Scott Gordon Chuck Ainlay(3) - "One Step At ATime'-George Strait-/ + "If You See Him"-Reba McEntire-/ + "Always Chad Evan«(1) - "Kennedy Center Homecoming: A Celebration Of Our Faith & Heritage"-Bill & Gloria Never The Same'-George Strait-/ Scotch Ralston Gaither-/ John Alagia(i) - "Live At Luther College'-Dave Matthews Band & Tim Reynolds-/Jeff Thomas Stephen Fitzmaurice(l) - "Human Being"- Seal-/ Tim Weidner Richard Lowe Stevo Albini(1) - 'Walking Into Clarksdale"-Jimmy Page & Robert Plant-/ Paul Hicks FloodM) - "Is This Desire?"-P.J. -
Tough Financial Times for Pickering
The Pickering 48 PAGES ✦ Metroland Durham Region Media Group ✦ WEDNESDAY, MARCH 15, 2006 ✦ Optional delivery $6 / Newsstand $1 It fits to a ‘T’ Off to Juniors Toyota Yaris Pickering Swim Club quite a ride members advance Wheels pullout Page B2 [ Briefly ] Pickering helps T ough financial times for Pickering mark 50 years PICKERING — There was a By Danielle Milley find a balance between the needs of the receptive to the idea. factored in. No changes were made to its distinctly Durham flavour as the Staff Writer City and the external restrictions that “Surveys show library materials are allocation in the budget, but CAO Tom Toronto and Region Conservation PICKERING — Imagine a Pickering have been placed upon us,” said Mayor the lifeblood of what we do,” she said, Quinn said it could be something talked authority celebrated a significant with no Dunbarton pool, a significantly Dave Ryan after a day and a adding it would cut a substan- about at a one-day session he is plan- milestone recently. reduced library collection, and a scaled half of budget committee dis- tial amount of materials and ning with council to discuss a number Uxbridge Mayor Gerri Lynn back Canada Day celebration. cussions. have a significant impact. of issues. O’Connor was re-elected vice- At the 2006 budget committee meet- Looking to the future, he Coun. Dickerson asked if Ward 1 City Councillor Kevin Ashe chairwoman as the conservation group, which serves west Dur- ing councillors rejected that Pickering, said a 15 per cent increase $100,000 could be cut from the questioned the expense of Dunbarton ham, held its 50th annual meeting but, faced with tough financial times, wouldn’t be acceptable to total budget of $4,311,000. -
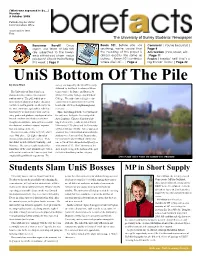
Students Slam Unis Bosses MP in Short Supply University Bosses Came to Union Council on Across the Entire University for Students Being Assessed
(What was supossed to be...) Monday 3 October 2005 Published by the USSU Communications Office. Issue number 1091 Free The University of Surrey Students’ Newspaper Konsumer Revolt! Once Room 101: Before you say Comment | You’re beautiful! | again, our team of lab-rats anything, we’re aware that Page 4 are subjected to the lower- the heading of this paper is Arts Section |Film, Music, etc. ends of the food-chain - value almost exactly the same as |Page 11 products! Check their offering before. Room 101 continues Puzzles| Freakin’ hell! That’s a this week | Page 9 where it left off... | Page 6 big freakin’ maze! | Page 22 UniS Bottom Of The Pile By Chris Ward survey was topped by the Open University, followed by the Royal Academy of Music, The University of Surrey has been Conservatoire for Dance and Drama, St slammed in the results of the national Mary’s University College, and Birkbeck student survey. The poll, which ques- College. The only chartered higher edu- tions students about their higher education cation institutes appearing in the top ten institute is said to provide an alternative to besides the OU were Loughborough and the more common league tables, which are Leicester. based purely on quantitative data, such as Those that slumped to the very bottom of entry grades and graduate employment rates. the poll were led by the University of the Instead, students are asked to scale their Arts (London). Chartered institutes hit- thoughts on qualitative data such as personal ting the low of the results included Brunel development, academic support, organisa- University (117th place) and the University tion and management, etc. -

Northumbria University News Issue 7
Top 50 in the UK for Research Power Autumn 2015 • northumbria.ac.uk • #iwantNU Issue 7 Forecast: A Bright Future NORTHUMBRIAUNIVERSITY NEWS PAGE “This is where I want to be” 9 Exclusive interview with our new Chancellor, Baroness Grey-Thompson (DBE) This positive result is the consequence of an ‘‘ ‘‘overall strategy that is grounded in quality Vice-Chancellor of Northumbria University, Professor Andrew Wathey Northumbria on the rise Northumbria University climbs to 28th in the UK for teaching quality in new league tables. orthumbria has taken Survey and Research Excellence the wider student experience.” consequence of an overall strategy study at Northumbria, the University another step forward in Framework, alongside significant Behind the headline improvement, that is grounded in quality – achieving is now the top post-1992 institution for its ambition to become improvements in entry standards and Northumbria was also ranked 28th significant progress in both teaching entry standards, moving up from 48th a new kind of excellent graduate employability. in the UK for teaching quality and and research, with Northumbria to 46th (and 34th in England). Nuniversity, rising two places in The In the 2016 Guide, The Sunday Times 42nd for overall student experience. recognised as the sector’s biggest riser The Sunday Times result follows Times and Sunday Times University said: “Northumbria University has set The Sunday Times also praised in research power.” recent successes for the University in League Table 2016. The University also out its stall with a public declaration Northumbria’s success in the 2014 There was also success at subject student satisfaction, research quality, saw significant gains in overall student that it wants to win a place among the Research Excellence Framework, level in The Sunday Times, with 10 of and graduate employability.