HAVING a URETERIC STENT What to Expect and How to Manage
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Coding for Angioplasty & Stent Procedures
Coding for Angioplasty & Stent Procedures July 2020 Jennifer Bash, RHIA, CIRCC, RCCIR, CPC, RCC Director of Coding Education Agenda • Introduction • Definitions • General Coding Guidelines • Presenting Problems/Medical Necessity for Angioplasty & Stent • General Angioplasty & Stent Procedures • Cervicocerebral Procedures • Lower Extremity Procedures Disclaimer The information presented is based on the experience and interpretation of the presenters. Though all of the information has been carefully researched and checked for accuracy and completeness, ADVOCATE does not accept any responsibility or liability with regard to errors, omissions, misuse or misinterpretation. CPT codes are trademark and copyright of the American Medical Association. Resources •AMA •CMS • ACR/SIR • ZHealth Publishing Angioplasty & Stent Procedures Angioplasty Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty, is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. Vascular Stent A stent is a tiny tube placed into the artery or vein used to treat vessel narrowing or blockage. Most stents are made of a metal or plastic mesh-like material. General Angioplasty & Stent Coding Guidelines • Angioplasty is not separately billable when done with a stent • Pre-Dilatation • PTA converted to Stent • Prophylaxis • EXCEPTION-Complication extending to a different vessel • Coded per vessel • Codes include RS&I • Territories • Hierarchy General Angioplasty -

Kidney, Renal Tubule – Dilation
Kidney, Renal Tubule – Dilation Figure Legend: Figure 1 Kidney, Renal tubule - Dilation in a male B6C3F1 mouse from a chronic study. Dilated tubules are noted as tracts running through the cortex and outer medulla. Figure 2 Kidney, Renal tubule - Dilation in a male F344/N rat from a chronic study. Tubule dilation is present throughout the outer stripe of the outer medulla, extending into the cortex. Figure 3 Kidney, Renal tubule - Dilation in a male B6C3F1 mouse from a chronic study. Slight tubule dilation is associated with degeneration and necrosis. Figure 4 Kidney, Renal tubule - Dilation in a male F344/N rat from a chronic study. Tubule dilation is associated with chronic progressive nephropathy. Comment: Renal tubule dilation may occur anywhere along the nephron or collecting duct system. It may occur in focal areas or as tracts running along the entire length of kidney sections (Figure 1). 1 Kidney, Renal Tubule – Dilation Renal tubule dilation may occur from xenobiotic administration, secondary mechanisms, or an unknown pathogenesis (see Kidney – Nephropathy, Obstructive (Figure 2). Dilation may result from direct toxic injury to the tubule epithelium interfering with absorption and secretion (Figure 3). It may also occur secondary to renal ischemia or from prolonged diuresis related to drug administration. Secondary mechanisms of tubule dilation may result from lower urinary tract obstruction, the deposition of tubule crystals, interstitial inflammation and/or fibrosis, and chronic progressive nephropathy (Figure 4). A few dilated tubules may be regarded as normal histologic variation. Recommendation: Renal tubule dilation should be diagnosed and given a severity grade. The location of tubule dilation should be included in the diagnosis as a site modifier. -

Testosterone Replacement Therapy Is Associated with an Increased Risk of Urolithiasis
World Journal of Urology (2019) 37:2737–2746 https://doi.org/10.1007/s00345-019-02726-6 ORIGINAL ARTICLE Testosterone replacement therapy is associated with an increased risk of urolithiasis Tyler R. McClintock1 · Marie‑Therese I. Valovska2 · Nicollette K. Kwon3 · Alexander P. Cole1,3 · Wei Jiang3 · Martin N. Kathrins1 · Naeem Bhojani4 · George E. Haleblian1 · Tracey Koehlmoos5 · Adil H. Haider3,6 · Shehzad Basaria7 · Quoc‑Dien Trinh1,3 Received: 16 November 2018 / Accepted: 7 March 2019 / Published online: 23 March 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose To determine whether TRT in men with hypogonadism is associated with an increased risk of urolithiasis. Methods We conducted a population-based matched cohort study utilizing data sourced from the Military Health System Data Repository (a large military-based database that includes benefciaries of the TRICARE program). This included men aged 40–64 years with no prior history of urolithiasis who received continuous TRT for a diagnosis of hypogonadism between 2006 and 2014. Eligible individuals were matched using both demographics and comorbidities to TRICARE enrollees who did not receive TRT. The primary outcome was 2-year absolute risk of a stone-related event, comparing men on TRT to non-TRT controls. Results There were 26,586 pairs in our cohort. Four hundred and eighty-two stone-related events were observed at 2 years in the non-TRT group versus 659 in the TRT group. Log-rank comparisons showed this to be a statistically signifcant dif- ference in events between the two groups (p < 0.0001). This diference was observed for topical (p < 0.0001) and injection (p = 0.004) therapy-type subgroups, though not for pellet (p = 0.27). -

Coronary Angiogram, Angioplasty and Stent Placement
Page 1 of 6 Coronary Angiogram, Angioplasty and Stent Placement A Patient’s Guide Page 2 of 6 What is coronary artery disease? What is angioplasty and a stent? Coronary artery disease means that you have a If your doctor finds a blocked artery during your narrowed or blocked artery. It is caused by the angiogram, you may need an angioplasty (AN-jee- buildup of plaque (fatty material) inside the artery o-plas-tee). This is a procedure that uses a small over many years. This buildup can stop blood from inflated balloon to open a blocked artery. It can be getting to the heart, causing a heart attack (the death done during your angiogram test. of heart muscle cells). The heart can then lose some of its ability to pump blood through the body. Your doctor may also place a stent at this time. A stent is a small mesh tube that is placed into an Coronary artery disease is the most common type of artery to help keep it open. Some stents are coated heart disease. It is also the leading cause of death for with medicine, some are not. Your doctor will both men and women in the United States. For this choose the stent that is right for you. reason, it is important to treat a blocked artery. Angioplasty and stent Anatomy of the Heart 1. Stent with 2. Balloon inflated 3. Balloon balloon inserted to expand stent. removed from into narrowed or expanded stent. What is a coronary angiogram? blocked artery. A coronary angiogram (AN-jee-o-gram) is a test that uses contrast dye and X-rays to look at the blood vessels of the heart. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -

Case Report Long-Term Results of Vascular Stent Placements for Portal Vein Stenosis Following Liver Transplantation
Int J Clin Exp Med 2017;10(3):5514-5520 www.ijcem.com /ISSN:1940-5901/IJCEM0042813 Case Report Long-term results of vascular stent placements for portal vein stenosis following liver transplantation Yue-Lin Zhang1,2, Chun-Hui Nie1,2, Guan-Hui Zhou1,2, Tan-Yang Zhou1,2, Tong-Yin Zhu1,2, Jing Ai3, Bao-Quan Wang1,2, Sheng-Qun Chen1,2, Zi-Niu Yu1,2, Wei-Lin Wang1,2, Shu-Sen Zheng1,2, Jun-Hui Sun1,2 1Department of Hepatobiliary and Pancreatic Interventional Center, The First Affiliated Hospital, School of Medi- cine, Zhejiang University, Hangzhou 310003, Zhejiang Province, China; 2Key Laboratory of Combined Multi-organ Transplantation, Ministry of Public Health, Hangzhou 310003, Zhejiang Province, China; 3Department of Oph- thalmology, The Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou 310009, Zhejiang Province, China Received October 25, 2016; Accepted January 4, 2017; Epub March 15, 2017; Published March 30, 2017 Abstract: Portal vein stenosis (PVS) is a serious complication after liver transplantation (LT) and can cause in- creased morbidity, graft loss, and patient death. The aim of this study was to evaluate the long-term treatment ef- fect of vascular stents in the management of PVS after LT. In the present study, follow-up data on 16 patients who received vascular stents for PVS after LT between July 2011 and May 2015 were analyzed. Of these, five patients had portal hypertension-related signs and symptoms. All procedures were performed with direct puncture of the intrahepatic portal vein and with subsequent stent placement. Embolization was required for significant collateral circulation. -
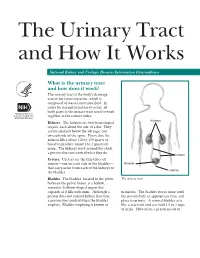
The Urinary Tract and How It Works
The Urinary Tract and How It Works National Kidney and Urologic Diseases Information Clearinghouse What is the urinary tract and how does it work? The urinary tract is the body’s drainage system for removing urine, which is composed of wastes and extra fluid. In order for normal urination to occur, all body parts in the urinary tract need to work together in the correct order. Kidneys Kidneys. The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine. The kidneys work around the clock; a person does not control what they do. Ureters Ureters. Ureters are the thin tubes of muscle—one on each side of the bladder— Bladder that carry urine from each of the kidneys to Urethra the bladder. Bladder. The bladder, located in the pelvis The urinary tract between the pelvic bones, is a hollow, muscular, balloon-shaped organ that expands as it fills with urine. Although a urination. The bladder stores urine until person does not control kidney function, the person finds an appropriate time and a person does control when the bladder place to urinate. A normal bladder acts empties. Bladder emptying is known as like a reservoir and can hold 1.5 to 2 cups of urine. How often a person needs to urinate depends on how quickly the kidneys Why is the urinary tract produce the urine that fills the bladder. -

Complications of Ureteroscopic Approaches, Including Incisions
18 Complications of Ureteroscopic Approaches, Including Incisions Farjaad M. Siddiq, MD and Raymond J. Leveillee, MD CONTENTS INTRODUCTION PREPARATION FOR URETEROSCOPY URETERAL ACCESS DILATION OF THE URETERAL ORIFICE: IS IT NECESSARY? COMPLICATIONS OF URETEROSCOPY URETERAL STENTS: ARE THEY NECESSARY? POSTOPERATIVE IMAGING COMPLICATIONS OF URETEROSCOPIC MANAGEMENT OF UPPER TRACT TCC COMPLICATIONS OF URETEROSCOPIC INCISIONS CONCLUSION REFERENCES SUMMARY Ureteroscopy has progressed from cystoscopic examination of a dilated ureter in a child in 1929 and the initial use of rigid ureteroscopes in the 1980s, to its current state of small caliber semirigid and flexible instruments. In this chapter the authors review complications of ureteroscopy including those associated with incisional techniques where one would anticipate a higher incidence of complications. They review the his- tory and development of modern ureteroscopes, focusing on engineering advances. Clinical points made include proper patient selection and preparation; proper use of dilators, wires, and ureteral access sheaths; and the incidence, identification, and man- agement of complications associated with ureterorenoscopy (both intraopertively and postoperatively). Key Words: Ureteroscopy; calculi; urinary stones; stricture or ureter; urothelial carcinoma; surgical complications. From: Advanced Endourology: The Complete Clinical Guide Edited by: S. Y. Nakada and M. S. Pearle © Humana Press Inc., Totowa, NJ 299 300 Siddiq and Leveillee INTRODUCTION Ureteroscopy has progressed from cystoscopic examination of a dilated ureter in a child with posterior urethral valves by Young and McKay (1) in 1929 and the initial use of a rigid ureteroscope by Perez-Castro Ellendt and Martinez-Pineiro (2,3) in the early 1980s, to its current state of small caliber semirigid and flexible instruments. -

Claudins in the Renal Collecting Duct
International Journal of Molecular Sciences Review Claudins in the Renal Collecting Duct Janna Leiz 1,2 and Kai M. Schmidt-Ott 1,2,3,* 1 Department of Nephrology and Intensive Care Medicine, Charité-Universitätsmedizin Berlin, 12203 Berlin, Germany; [email protected] 2 Molecular and Translational Kidney Research, Max-Delbrück-Center for Molecular Medicine in the Helmholtz Association (MDC), 13125 Berlin, Germany 3 Berlin Institute of Health (BIH), 10178 Berlin, Germany * Correspondence: [email protected]; Tel.: +49-(0)30-450614671 Received: 22 October 2019; Accepted: 20 December 2019; Published: 28 December 2019 Abstract: The renal collecting duct fine-tunes urinary composition, and thereby, coordinates key physiological processes, such as volume/blood pressure regulation, electrolyte-free water reabsorption, and acid-base homeostasis. The collecting duct epithelium is comprised of a tight epithelial barrier resulting in a strict separation of intraluminal urine and the interstitium. Tight junctions are key players in enforcing this barrier and in regulating paracellular transport of solutes across the epithelium. The features of tight junctions across different epithelia are strongly determined by their molecular composition. Claudins are particularly important structural components of tight junctions because they confer barrier and transport properties. In the collecting duct, a specific set of claudins (Cldn-3, Cldn-4, Cldn-7, Cldn-8) is expressed, and each of these claudins has been implicated in mediating aspects of the specific properties of its tight junction. The functional disruption of individual claudins or of the overall barrier function results in defects of blood pressure and water homeostasis. In this concise review, we provide an overview of the current knowledge on the role of the collecting duct epithelial barrier and of claudins in collecting duct function and pathophysiology. -

Discharge Instructions for Ureteroscopy, Laser Lithotripsy and Stent Insertion
Dr. Kevin G. Kwan, BSc (Hons), MD, FRCS(C) Minimally Invasive Surgery and General Urology Assistant Clinical Professor Division of Urology, Department of Surgery McMaster University Chief of Surgery, Milton District Hospital Georgetown Hospital • Milton District Hospital • Oakville Trafalgar Memorial Hospital Suite 205 - 311 Commercial Street • Milton • Ontario • L9T 3Z9 • Tel: (905) 875-3920 • Fax: (905) 875-4340 Email: [email protected] • Web: www.haltonurology.com Discharge Instructions for Ureteroscopy, Laser lithotripsy and Stent insertion Ureteroscopy is a procedure where a scope is passed through the urethra and bladder and into the ureter (the tubes that carry urine from the kidneys to the bladder) to the point where the stone is located. A small laser fiber is then used to break the stone into small pieces that are then extracted or flushed out. In most cases, to ensure that the kidney drains urine well after surgery, a ureteral stent is left in place. Ureteroscopy can also be performed for stones located within the kidney. Similar to ureteral stones, kidney stones can be fragmented and removed with baskets. Occasionally, a kidney stone will fragment with a laser into very small pieces (grains of sand), too small to be basketed. A stent is usually left in place to allow these pieces to clear over time. Ureteral Stenting: Almost always after ureteroscopy, a ureteral stent will be placed. This is a thin, hollow, plastic tube that is used temporarily to keep the ureter open and facilitates drainage of urine down to the bladder until it heals. It also allows the urine to drain and any small stone fragments to pass freely. -

Angiogram, Balloon Angioplasty and Stent Placement for Peripheral Arterial Disease
Form: D-5093 Angiogram, Balloon Angioplasty and Stent Placement for Peripheral Arterial Disease What to expect before, during and after these procedures Check in at: Toronto General Hospital Medical Imaging Reception 1st Floor – Munk Building Date and time of my angiogram: Date: Time: My follow-up appointment: Date: Time: What is an angiogram? An angiogram is a test that lets your doctor see how your blood is flowing (circulating) through your arteries. Using special x-rays, an angiogram shows narrow or blocked arteries, and normal blood vessels. The results are like a “route map” of the blood vessels in your body. Since arteries do not show up on ordinary x-rays, a dye called a contrast is injected into the arteries to make them visible for a short period of time. Two common therapies that can be done during the angiogram are balloon angioplasty and stent placement. What is a balloon angioplasty? Angioplasty is an x-ray guided procedure to open up a blocked or narrowed artery. A plastic tube called a catheter is inserted close to the blocked or narrowed artery, helping a thin wire pass through the blockage or narrowing. A special balloon is then inserted over the wire. The balloon is inflated, flattening the plaque against the artery wall allowing blood to flow again. All balloons, wires and catheters are removed at the end of the procedure. blood vessel plaque inflated balloon balloon catheter 2 What is a stent placement? Sometimes a stent (a small metal mesh tube) is used with the balloon. The doctor places the stent into the artery to hold it open after it has been expanded with the balloon. -

Novel Technique for Performing Retrograde Pyelogram Through A
Case Study DOI: 10.22374/jeleu.v1i1.2 NOVEL TECHNIQUE FOR PERFORMING RETROGRADE PYELOGRAM THROUGH A URETERIC STENT Jonathan Cobley1 MBBCh MRCS and Wasim Mahmalji1 MBBS FRCS 1Hereford County Hospital, Stonebow Road, Hereford, UK. Corresponding author: [email protected] Submitted: March 8, 2017. Accepted: March 9, 2018. Published: June 2, 2018. A female was diagnosed with kidney stones in Nepal two weeks later. Subsequent CT urogram showed an and treated with ureteroscopy and lasertripsy for a left obstructed left kidney secondary to a stricture and ureteric stone. She moved to the UK and was referred the patient complained of left-sided pain once again. for urology opinion with left-sided abdominal pain. POINT OF TECHNIQUE Non-contrast computed tomography of the renal tract (CT KUB) showed a 5–6 mm calculus below the Retrograde pyelogram was attempted but no contrast left pelviureteric junction (PUJ) and multiple lower made it beyond the stricture (see Figure 1). There was pole calculi. At ureteroscopy appearances were of a a pinhole stricture through which a guidewire was long-term ureteric stone which had the middle of it passed with great diffi culty and it was impossible to lasered in Nepal. Subequently, urothelium had started pass 6 French ureteric catheter through the stricture. healing over the remaining portion. Due to the severity of the stricture it was of paramount This was lasered to allow passage of a 6 French, importance to place a stent and to ensure its correct 24-cm ureteric stent to be left in situ prior to re-look placement however there was no retrograde pyelogram ureteroscopy.