COVID-19: Emerging Trials and Treatments
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(MGH) COVID-19 Treatment Guidance
Version 8.0 4/28/2021 10:00AM © Copyright 2020 The General Hospital Corporation. All Rights Reserved. Massachusetts General Hospital (MGH) COVID-19 Treatment Guidance This document was prepared (in March, 2020-April, 2021) by and for MGH medical professionals (a.k.a. clinicians, care givers) and is being made available publicly for informational purposes only, in the context of a public health emergency related to COVID-19 (a.k.a. the coronavirus) and in connection with the state of emergency declared by the Governor of the Commonwealth of Massachusetts and the President of the United States. It is neither an attempt to substitute for the practice of medicine nor as a substitute for the provision of any medical professional services. Furthermore, the content is not meant to be complete, exhaustive, or a substitute for medical professional advice, diagnosis, or treatment. The information herein should be adapted to each specific patient based on the treating medical professional’s independent professional judgment and consideration of the patient’s needs, the resources available at the location from where the medical professional services are being provided (e.g., healthcare institution, ambulatory clinic, physician’s office, etc.), and any other unique circumstances. This information should not be used to replace, substitute for, or overrule a qualified medical professional’s judgment. This website may contain third party materials and/or links to third party materials and third party websites for your information and convenience. Partners is not responsible for the availability, accuracy, or content of any of those third party materials or websites nor does it endorse them. -

A Qualitative Review of Cruise Service Quality: Case Studies from Asia
sustainability Article A Qualitative Review of Cruise Service Quality: Case Studies from Asia Yeohyun Yoon 1 and Kyoung Cheon Cha 2,* 1 School of Hotel and Tourism Management, Youngsan University, Busan 48015, Korea; [email protected] 2 Department of Business Administration, Dong-A University, Busan 49236, Korea * Correspondence: [email protected] Received: 2 September 2020; Accepted: 29 September 2020; Published: 30 September 2020 Abstract: Although the cruise sector is considered an ‘unreplaceable’ form of tourism, with the cruise industry recording steady growth over the years, there is a lack of research and analysis on cruise ships themselves. Accordingly, this study sought to determine whether service quality differences among ships operating in the Asian market could suggest broader implications for the sustainability of the cruise industry. We chose the SERVQUAL framework for the analysis; we also employed the multiple case study method and topic synthesis to compare the service quality of three ships. Of the ships investigated—the Costa Victoria, Diamond Princess, and Superstar Virgo—the Diamond Princess had the highest service quality. Based on the results, we outlined suggestions for improving the quality of cruise services, including introducing the latest large ships and high-tech facilities, complying with the departure and arrival times of sailing schedules, improving the ratio of crew members per passenger, establishing a cruise personnel training system, and expanding membership program operations. Keywords: cruise; service quality; SERVQUAL; onboard attributes 1. Introduction Cruise tourism is one of the fastest growing tourism segments, and it has undergone significant transformation, especially in the last few decades [1,2]. -

Progress in the Development of Potential Therapeutics and Vaccines Against COVID-19 Pandemic
Acta Scientific Pharmaceutical Sciences (ISSN: 2581-5423) Volume 5 Issue 7 July 2021 Review Article Progress in the Development of Potential Therapeutics and Vaccines against COVID-19 Pandemic Abhishek Kumar Yadav, Shubham Kumar and Vikramdeep Monga* Received: May 02, 2021 Department of Pharmaceutical Chemistry, ISF College of Pharmacy, Moga, Punjab, Published: June 09, 2021 India © All rights are reserved by Vikramdeep *Corresponding Author: Vikramdeep Monga, Department of Pharmaceutical Monga., et al. Chemistry, ISF College of Pharmacy, Moga, Punjab, India. Abstract Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes COVID-19 or coronavirus disease 2019 and the same has been declared as a global pandemic by WHO which marked the third introduction of a virulent coronavirus into human society. This a threat to human life worldwide. Considerable efforts have been made for developing effective and safe drugs and vaccines against is a highly pathogenic human coronavirus in which pneumonia of unknown origin was identified in China in December 2019 and is SARS-CoV-2. The current situation and progress in the development of various therapeutic candidates including vaccines in preclini- cal and clinical studies have been described in the manuscript. Until now, many people have been infected with this lethal virus, and a lot of people have died from this COVID-19. This viral disease spreads by coming in contact with an infected person. Understand- ing of SARS-CoV-2 is growing in relation to its epidemiology, virology, and clinical management strategies. Till date, very few drugs or vaccines have been developed or approved for the treatment of this deadly disease of COVID-19 and many candidates are under the clinical development pipeline. -

Impact of SARS-Cov-2 Variant on the Severity of Maternal Infection and Perinatal Outcomes: Data from the UK Obstetric Surveillan
medRxiv preprint doi: https://doi.org/10.1101/2021.07.22.21261000; this version posted July 25, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY 4.0 International license . Impact of SARS-CoV-2 variant on the severity of maternal infection and perinatal outcomes: Data from the UK Obstetric Surveillance System national cohort. Nicola Vousden PhD1, Rema Ramakrishnan PhD1, Kathryn Bunch MA1, Edward Morris MD2, Nigel Simpson MBBS3, Christopher Gale PhD4, Patrick O’Brien MBBCh,2,5, Maria Quigley MSc1, Peter Brocklehurst MSc6, Jennifer J Kurinczuk MD1, Marian Knight DPhil1 1National Perinatal Epidemiology Unit, Nuffield Department of Population Health, University of Oxford, UK 2Royal College of Obstetricians and Gynaecologists, London, UK 3Department of Women's and Children's Health, School of Medicine, University of Leeds, UK 4Neonatal Medicine, School of Public Health, Faculty of Medicine, Imperial College London, London, UK 5Institute for Women’s Health, University College London, London, UK 6Birmingham Clinical Trials Unit, Institute of Applied Health Research, University of Birmingham, UK *Corresponding author: Marian Knight National Perinatal Epidemiology Unit, Nuffield Department of Population Health, University of Oxford, UK 01865 289700 [email protected] NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. 1 medRxiv preprint doi: https://doi.org/10.1101/2021.07.22.21261000; this version posted July 25, 2021. -

An Examination of COVID-19 Medications' Effectiveness
healthcare Review An Examination of COVID-19 Medications’ Effectiveness in Managing and Treating COVID-19 Patients: A Comparative Review Mahmoud Al-Masaeed 1,* , Mohammad Alghawanmeh 2, Ashraf Al-Singlawi 3 , Rawan Alsababha 4 and Muhammad Alqudah 1 1 Faculty of Health and Medicine, University of Newcastle, Callaghan 2308, Australia; [email protected] 2 Faculty of Pharmacy, Philadelphia University, Amman 19392, Jordan; [email protected] 3 Independent Scholar, Amman 11731, Jordan; [email protected] 4 School of nursing and Midwifery, Western Sydney University, Sydney 2560, Australia; [email protected] * Correspondence: [email protected] Abstract: Background: The review seeks to shed light on the administered and recommended COVID- 19 treatment medications through an evaluation of their efficacy. Methods: Data were collected from key databases, including Scopus, Medline, Google Scholar, and CINAHL. Other platforms included WHO and FDA publications. The review’s literature search was guided by the WHO Citation: Al-Masaeed, M.; solidarity clinical trials for COVID-19 scope and trial-assessment parameters. Results: The findings Alghawanmeh, M.; Al-Singlawi, A.; indicate that the use of antiretroviral drugs as an early treatment for COVID-19 patients has been Alsababha, R.; Alqudah, M. An useful. It has reduced hospital time, hastened the clinical cure period, delayed and reduced the Examination of COVID-19 need for mechanical and invasive ventilation, and reduced mortality rates. The use of vitamins, Medications’ Effectiveness in minerals, and supplements has been linked to increased immunity and thus offering the body a Managing and Treating COVID-19 fighting chance. Nevertheless, antibiotics do not correlate with improving patients’ wellbeing and Patients: A Comparative Review. -
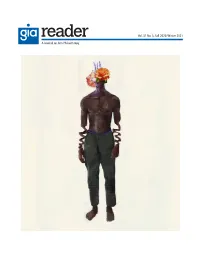
GIA Reader, Volume 31, Number 3 (Winter 2021)
Vol. 31 No. 3, Fall 2020/Winter 2021 A Journal on Arts Philanthropy 2 Grantmakers in the Arts Reader: Volume 31, No. 3, Fall 2020/Winter 2021 RESEARCH Foundation Grants to Arts and Culture, 2018: A One-Year Snapshot ...................................................5 Reina Mukai Public Funding for the Arts 2020 ............................................................................................................12 Ryan Stubbs and Patricia Mullaney-Loss READINGS Centered. Elevated. Celebrated. Well Resourced. Welcome to Nonprofit Wakanda. .........................16 David McGoy DEI Work is Governance Work ................................................................................................................18 Jim Canales and Barbara Hostetter The Equity Builder Loan Program: Looking Toward Autonomy and Freedom from the Crisis Cycle ................................................................................................................................20 Quinton Skinner Equity. Equity. Equity. ..............................................................................................................................25 Shaunda McDill Arts Funders Should Build Stability and Resilience for Black Artists and Cultural Communities .......................................................................................................................26 Tracey Knuckles A Question of (dis)Trust: Lessons When Your Institution Gets Taken Down ....................................27 Anida Yoeu Ali and Shin Yu Pai San Diego/Tijuana: -

Vaccines from Bahrain, Which Are Under Probe, Are Chinese, Officials
WITHOUT F EAR OR FAVOUR Nepal’s largest selling English daily Vol XXIX No. 29 | 12 pages | Rs.5 O O Printed simultaneously in Kathmandu, Biratnagar, Bharatpur and Nepalgunj 34.4 C 2.5 C Friday, March 19, 2021 | 06-12-2077 Nepalgunj Jumla Vaccines from Bahrain, which are under probe, are Chinese, officials say Nepal’s drug regulator says it is consulting with foreign and health ministries, as the issue is not just technical but also concerns bilateral ties and diplomacy. ARJUN POUDEL Sinopharm’s BBIBP-CorV but not to KATHMANDU, MARCH 18 Sinovac’s CoronaVac. Nepal, however, has not rolled out A report on an investigation into Sinopharm vaccines yet. The Oxford- how 2,000 doses of Covid-19 vaccine AstraZeneca vaccine was the first to were brought to Nepal by a Bahraini get emergency use authorisation in prince was to be submitted on Nepal. The vaccine, manufactured by Thursday evening. the Serum Institute of India under the But officials on Thursday afternoon brand name of Covishield, is current- said that the vaccines were Chinese, ly being used in Nepal. not AstraZeneca as claimed before. Sheikh Mohamed Hamad Mohamed At least two officials at the Health al-Khalifa, the Bahraini prince, and Ministry, who did not wish to be his team landed in Kathmandu on named, said that the vaccines from Monday on an Everest mission. Bahrain are Chinese and developed The Nepali embassy in Bahrain on by Sinovac Biotech, for which Nepal Monday said in a statement that the has not granted emergency use prince’s team would be carrying 2,000 authorisation. -

Official Report of This Meeting
COVID-19 Committee Thursday 18 February 2021 Session 5 © Parliamentary copyright. Scottish Parliamentary Corporate Body Information on the Scottish Parliament’s copyright policy can be found on the website - www.parliament.scot or by contacting Public Information on 0131 348 5000 Thursday 18 February 2021 CONTENTS Col. CITIZENS PANEL ................................................................................................................................................ 5 SUBORDINATE LEGISLATION............................................................................................................................. 26 Personal Protective Equipment (Temporary Arrangements) (Coronavirus) (Scotland) Regulations 2021 (SSI 2021/50) ............................................................................................................. 26 Health Protection (Coronavirus) (Restrictions and Requirements) (Local Levels) (Scotland) Amendment (No 16) Regulations 2021 [Draft] ........................................................................................ 26 COVID-19 COMMITTEE 6th Meeting 2021, Session 5 CONVENER *Donald Cameron (Highlands and Islands) (Con) DEPUTY CONVENER Monica Lennon (Central Scotland) (Lab) COMMITTEE MEMBERS *Willie Coffey (Kilmarnock and Irvine Valley) (SNP) *Maurice Corry (West Scotland) (Con) *Annabelle Ewing (Cowdenbeath) (SNP) *John Mason (Glasgow Shettleston) (SNP) *Stuart McMillan (Greenock and Inverclyde) (SNP) *Mark Ruskell (Mid Scotland and Fife) (Green) *Beatrice Wishart (Shetland Islands) (LD) -

COVID-Clinical-Update.Pdf
COVID-19 Update Jorge Mera, MD Whitney Essex, APRN Questions • I have heard that the only thing that will end this pandemic is acquisition of immunity. That means either natural or by vaccination, therefore, in the absence of vaccination, we should be encouraging natural immunity (infection with recovery) rather than advocating avoidance. Any chosen path will result in casualties. however, our current path of avoidance is drawing out the process and hurting our nation. Please comment. • Prescriptions for zithromax and hydroxychloroquine have skyrocketed across the nation. Is there any role for these medications for outpatients, either prophylactically or for treatment? Please also discuss other treatments being advocated such as zinc. Dynamic interventions to control COVID-19 pandemic: a multivariate prediction modelling study comparing 16 worldwide countries • Non-pharmacological interventions (NPI) have been the mainstay for controlling the COVID-19 pandemic. • While NPIs are effective in preventing health systems overload, these long-term measures are likely to have significant adverse economic consequences • Many countries are currently considering to lift the NPIs • Dynamic NPIs, with intervals of relaxed social distancing, may provide a more suitable alternative, • But the ideal frequency and duration of intermittent NPIs, and the ideal “break” when interventions can be temporarily relaxed, remain uncertain • Multivariate prediction model, based on up-to-date transmission and clinical parameters, to simulate outbreak traJectories in 16 countries, from diverse regions and economic categories. • In each country, we then modelled the impacts on intensive care unit (ICU) admissions and deaths over an 18-month period for following scenarios: 1. No intervention 2. Consecutive cycles of mitigation measures followed by a relaxation period 3. -

Ongoing Living Update of Potential COVID-19 Therapeutics: Summary of Rapid Systematic Reviews
Ongoing Living Update of Potential COVID-19 Therapeutics: Summary of Rapid Systematic Reviews RAPID REVIEW – July 13th 2020. (The information included in this review reflects the evidence as of the date posted in the document. Updates will be developed according to new available evidence) Disclaimer This document includes the results of a rapid systematic review of current available literature. The information included in this review reflects the evidence as of the date posted in the document. Yet, recognizing that there are numerous ongoing clinical studies, PAHO will periodically update these reviews and corresponding recommendations as new evidence becomes available. 1 Ongoing Living Update of Potential COVID-19 Therapeutics: Summary of Rapid Systematic Reviews Take-home messages thus far: • More than 200 therapeutic options or their combinations are being investigated in more than 1,700 clinical trials. In this review we examined 26 therapeutic options. • Preliminary findings from the RECOVERY Trial showed that low doses of dexamethasone (6 mg of oral or intravenous preparation once daily for 10 days) significantly reduced mortality by one- third in ventilated patients and by one fifth in patients receiving oxygen only. The anticipated RECOVERY Trial findings and WHO’s SOLIDARITY Trial findings both show no benefit via use of hydroxychloroquine and lopinavir/ritonavir in terms of reducing 28-day mortality or reduced time to clinical improvement or reduced adverse events. • Currently, there is no evidence of benefit in critical outcomes (i.e. reduction in mortality) from any therapeutic option (though remdesivir is revealing promise as one option based on 2 randomized controlled trials) and that conclusively allows for safe and effective use to mitigate or eliminate the causative agent of COVID-19. -

RECOVERY Protocol V12 (2020-12-16)
RANDOMISED EVALUATION OF COVID-19 THERAPY (RECOVERY) Background: In early 2020, as this protocol was being developed, there were no approved treatments for COVID-19, a disease induced by the novel coronavirus SARS-CoV-2 that emerged in China in late 2019. The UK New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) advised that several possible treatments should be evaluated, including Lopinavir-Ritonavir, low-dose corticosteroids, and Hydroxychloroquine (which has now been done). A World Health Organization (WHO) expert group issued broadly similar advice. These groups also advised that other treatments will soon emerge that require evaluation. Eligibility and randomisation: This protocol describes a randomised trial among patients hospitalised for COVID-19. All eligible patients are randomly allocated between several treatment arms, each to be given in addition to the usual standard of care in the participating hospital: No additional treatment vs colchicine vs corticosteroids (children only) vs intravenous immunoglobulin (children only). In a factorial design (in the UK alone), eligible patients are allocated simultaneously to no additional treatment vs convalescent plasma vs synthetic neutralising antibodies (REGN-COV2). Separately, all participants aged 18 years or older will be allocated to either aspirin vs control. The study allows a subsequent randomisation for patients with progressive COVID-19 (evidence of hyper-inflammatory state): No additional treatment vs tocilizumab. For patients for whom not all the trial arms are appropriate or at locations where not all are available, randomisation will be between fewer arms. Adaptive design: The interim trial results will be monitored by an independent Data Monitoring Committee (DMC). The most important task for the DMC will be to assess whether the randomised comparisons in the study have provided evidence on mortality that is strong enough (with a range of uncertainty around the results that is narrow enough) to affect national and global treatment strategies. -

COVID and COVID Vaccine Update
Friday General Session COVID and COVID Vaccine Update Jason Bowling, MD Associate Professor of Infectious Disease, Medical Director of Infection Control and Hospital Epidemiologist Company UT Health San Antonio San Antonio, Texas Educational Objectives By completing this educational activity, the participant should be better able to: 1. Evaluate the diagnostic challenges surrounding COVID. 2. Assess the risk factors for mild versus severe disease in patients infected with COVID. 3. Assess the rapidly changing treatment landscape for COVID patients with mild to moderate disease. Discuss the mechanism of action, side effects, and adverse events of COVID vaccines and review recommendations regarding COVID vaccination. Speaker Disclosure Dr. Bowling has disclosed that neither he nor members of his immediate family have a relevant financial relationship with an ineligible company. 6 COVID-19 and COVID-19 Vaccine Update Disclosures Jason Bowling, MD, FIDSA Associate Professor of Medicine Medical Director Infection Prevention UH & UTHSA Hospital Epidemiologist, University Hospital • I have no financial disclosures or conflicts of interest to report. • I will discuss medications being used in the context of a clinical trial. 12 Objectives • Analyze the clinical impact of the virology and epidemiology of COVID-19. • Evaluate the diagnostic challenges surrounding COVID-19. • Assess the rapidly changing treatment landscape for COVID-19 patients: outpatients and inpatients. • Discuss the mechanism of action, side effects, and adverse effects of COVID-19 vaccines and review recommendations regarding COVID-19 vaccination. https://coronavirus.jhu.edu/map.html - Accessed 5-19-21 34 San Antonio Metro Health: 5-19-21 56 1 Hospitalized COVID-19 Patients IHME COVID-19 PROJECTIONS: TEXAS University Hospital 5-19-21 COVID-19 (healthdata.org) – Updated 5/19/21 78 Brief SARS-CoV-2 Virology SARS-CoV-2 Pathogenesis • Spike protein binds ACE-2 receptor in human host • ACE-2 receptors .