Heterogeneity of Distribution of Tuberculosis in Sheka Zone, Ethiopia: Drivers and Temporal Trends
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
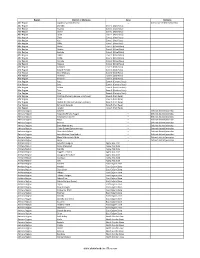
Districts of Ethiopia
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

Impact of Deforestation on Biodiversity, Soil Carbon Stocks, Soil Quality, Runoff and Sediment Yield at Southwest Ethiopia’S Forest Frontier
Impact of deforestation on biodiversity, soil carbon stocks, soil quality, runoff and sediment yield at southwest Ethiopia’s forest frontier Henok Kassa Tegegne Proefschrift voorgedragen tot het behalen van de graad van Doctor in de Wetenschappen Geografie Faculteit Wetenschappen Henok Kassa Tegegne Impact of deforestation on biodiversity, soil carbon stocks, soil quality, runoff and sediment yield at southwest Ethiopia’s forest frontier Proefschrift voorgelegd tot het behalen van de graad van Doctor in de Wetenschappen: Geografie 2016-2017 Copyright: Henok Kassa 2017 Published by: Department of Geography - Ghent University Krijgslaan 281 (S8), 9000 Gent (Belgium) (c) All rights reserved. ix x Promoter: Prof. Dr. Jan Nyssen, Department of Geography, Faculty of Sciences, Ghent University, Belgium Co-promoter: Prof. Dr. Jean Poesen, Department of Earth and Environmental Sciences, Section of Geography and Tourism, KU Leuven, Belgium Members of the Jury: Prof. Dr. Nico Vandeweghe, Department of Geography, Faculty of Sciences, Ghent University, Belgium (Chair) Dr. Denyse Snelder, Senior Advisor Natural Resources Management, VU Amsterdam, The Netherlands Prof. Dr. Stefaan Dondeyne, Department of Earth and Environmental Sciences, Section of Soil and Water Management, KU Leuven, Belgium Prof. Dr. Ann Verdoodt, Department of Soil Management, Faculty of Biosciences Engineering, Ghent University, Belgium Dr. Amaury Frankl, Department of Geography, Faculty of Sciences, Ghent University, Belgium (secretary) Dr. Miro Jacob, Department of Geography, Faculty of Sciences, Ghent University, Belgium Dean: Prof. Dr. Herwig Dejonghe Rector: Prof. Dr. Anne De Paepe xi xii Acknowledgements First and foremost, I thank the Almighty God for granting me the capability and patience to accomplish the study. Firstly, I would like to express my sincere gratitude to my promoters Prof. -

Ethiopia: a Situation Analysis and Trend Assessment
writenet is a network of researchers and writers on human rights, forced migration, ethnic and political conflict WRITENET writenet is the resource base of practical management (uk) e-mail: [email protected] independent analysis ETHIOPIA: A SITUATION ANALYSIS AND TREND ASSESSMENT A Writenet Report by Sarah Vaughan commissioned by United Nations High Commissioner for Refugees, Protection Information Section (DIP) January 2004 Caveat: Writenet papers are prepared mainly on the basis of publicly available information, analysis and comment. The papers are not, and do not purport to be, either exhaustive with regard to conditions in the country surveyed, or conclusive as to the merits of any particular claim to refugee status or asylum. The views expressed in the paper are those of the author and are not necessarily those of UNHCR, Writenet or Practical Management. ETHIOPIA: A SITUATION ANALYSIS AND TREND ASSESSMENT TABLE OF CONTENTS List of Acronyms ..................................................................................... iii Executive Summary ..................................................................................v 1 Introduction........................................................................................1 2 Review of the Contemporary Situation ...........................................4 2.1 State/Government ........................................................................................4 2.1.1 Ethnic Federalism: Constitutional Framework and Issues ................4 2.1.2 Organization of the Executive -

By Seyoum Mesfin Seyoum
Federalism at the Margins of the Ethiopian State: The Lived Experience of the Majang People By Seyoum Mesfin Seyoum A Dissertation Submitted to ADDIS ABABA UNIVERSITY Requirements for the Degree of DOCTOR OF PHILOSOPHY in Federal Studies College of Law and Governance, Center for Federal Studies Addis Ababa University Addis Ababa, Ethiopia June 2015 Contents Abstract ........................................................................................................................................... v Acknowledgement ......................................................................................................................... ix List of Acronyms .......................................................................................................................... xii List of Figures .............................................................................................................................. xiv List of Tables ............................................................................................................................... xvi Chapter 1 ......................................................................................................................................... 1 Introduction ..................................................................................................................................... 1 1.1 The Political Context: From a Unitarian to a Federal State .......................................................... 1 1.2 The Zonal Setting: Description of the Main Study -

The Culture of Power in Contemporary Ethiopian Political Life
Studies 10 omslag_edita 03-12-09 15.47 Sida 1 THE CULTURE OF POWER IN CONTEMPORARY ETHIOPIAN POLITICAL LIFE OF POWER IN CONTEMPORARY THE CULTURE The Culture of Power in Contemporary Ethiopian Political Life SARAH VAUGHAN AND KJETIL TRONVOLL SARAH VAUGHAN AND KJETIL TRONVOLL Sarah Vaughan is a Research Consultant and Honorary Fellow of the School of Social and Political Studies of the University of Edinburgh. Kjetil Tronvoll is a research fellow and Director of the Horn of Africa Programme at the For more than a decade, reforms designed to liberalise Norwegian Centre for Human Rights at the University of Oslo. Ethiopia’s economy, decentralise its state, and democratise its politics have sought to reverse a history of centralised autocracy and violent political conflict. Despite important advances, the capacity and the freedom of action of civil society and political opposition remain limited. The cur- rent period is critical in terms both of political stability and pluralism, and of pro-poor socio-economic development in Ethiopia. The study advocates an analysis of power that takes account of the political culture, knowledge, and be- liefs of Ethiopia’s diverse citizens. The authors argue that Sida involving all Ethiopians in decisions affecting their lives is studies one of the most significant challenges to socio-political transformation. THE SIDA STUDIES-SERIES OFFERS A SELECTION OF THE REPORTS AND STUDIES COMMISSIONED BY DIFFERENT no. DEPARTMENTS AT SIDA. THE SELECTION IS MADE TO REFLECT ISSUES OF RELEVANCE TO SIDA’S POLICIES AND PRACTICES, BUT EACH REPORT EXPRESSES THE VIEWS AND FINDINGS OF ITS WRITER(S). Swedish International Development Cooperation Agency Address: SE–105 25 Stockholm, Sweden. -

The Contribution of GUDO Forest Conservation Culture Is Key to Biodiversity Conservation
Journal of Geography & Natural Disasters Research The contribution of GUDO forest conservation culture is key to biodiversity conservation Getaneh Haile Shoddo Department of Natural Resource Management, Jigjiga University,Ethopia. ABSTRACT Background: The Sheka people have long been sustainably managing and conserving the Sheka forest by utilizing different procedures. Shockingly, these indigenous methods for natural resource management are ordinarily absent from scientific forest management and not archived. This paper aims to document “the GUDO culture” and demonstrate how the Sheka people through their indigenous culture can provide valuable, appropriate, and effective forest conservation strategies. Thus, every culture has a system of beliefs that guides their interactions with nature. One of the traditional forest management practice commonly found in Sheka zone is the GUDO. Results: The GUDO is a designated forest area mostly found in the mountainous and the rocky area of the Sheka zone. It is found mostly in rocky and mountainous parts of the Sheka zone. They are cultural symbols related to indigenous beliefs and signify spiritual connections to the forestland. Conclusions: This paper concludes that the GUDO forest conservation culture is illustrated in the Sheka people forest utilization, protection, and management. Therefore, the GUDO forest conservation culture provides important insights into the protection of various forest types and tree species, contributing to the conservation of biodiversity. Keywords: Gudo Culture; Forest; Indigenous Belief; Natural Resource Management. INTRODUCTION indigenous networks, people groups, and countries (Martinez Recent developments in the field of traditional forest-related Cobo, 1986/7). Numerous specialists have put accentuation on knowledge have led to renewed interest in the conservation, incorporating traditional forest-related knowledge and scientific management, and sustainable use of natural resources. -

Forest Allocation, Bene T Sharing, and Management Practice in the KOBO
Forest Allocation, Benet Sharing, and Management Practice in the KOBO Community Forest Among the Sheka People Getaneh Haile Shoddo ( [email protected] ) Jigjiga University Research Keywords: KOBO forest, forest allocation, forest benet sharing and forest management practice Posted Date: October 22nd, 2020 DOI: https://doi.org/10.21203/rs.3.rs-94567/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/17 Abstract Background: Sheka people have the right to forest allocation, benet sharing, and management practice that they possess due to traditional ownership or other traditional occupation. Locally, these forests are known as KOBO. There is a scarcity of documented information on the KOBO culture of forest allocation, benet sharing, and management practice among Sheka people. A study was conducted in Sheka zone southwestern Ethiopia. Methods: A framework based on ethnographic information is proposed in this paper; accordingly, qualitative indicators are suggested for different variables relating to indigenous forest allocation, benet sharing, and management practice. A representative sample of 20 volunteered research participants were chosen. Observational and interview surveys were done by the rst author through personal visits. Results: The analysis of data shows the KOBO culture is productive and ecient for forest management, and this useful culture has demonstrated its signicance in the protection of various forest types and tree species, contributing to the conservation of biodiversity. These results lend support to the idea that the KOBO forest conservation culture is illustrated in the Sheka people forest utilization, protection, and management provide important insights into the protection of various forest types and tree species, contributing to the conservation of biodiversity. -

Evaluation of the Financial Growth and Performance of Tepi Coffee
Global Journal of Management and Business Research: D Accounting and Auditing Volume 18 Issue 1 Version 1.0 Year 2018 Type: Double Blind Peer Reviewed International Research Journal Publisher: Global Journals Online ISSN: 2249-4588 & Print ISSN: 0975-5853 Evaluation of the Financial Growth and Performance of Tepi Coffee Producer Farmers' Cooperatives Union, Sheka Zone, South West Ethiopia By Abdu Mohammed Assfaw Mizan Tepi University Abstract- Financial performance analysis of a firm is made from its audited financial reports, balance sheets and income statements, to measure its liquidity, solvency, asset management efficiency and profitability position in maximizing the wealth of owners. In line with this, the main purpose of the paper is Evaluation of the Financial Growth and Performances of Tepi Forest Coffee Producer Farmers' Cooperative Union, Sheka Zone, South West Ethiopia. For attaining this objective, secondary data were drawn from audited financial statements of the union for 2010-2016 G.C. and analyzed through ratios and trend analytical techniques. The result of the study revealed current ratio, quick ratio and networking capital were above the standard denoting that the liquidity position of the union is satisfactory. However, the debt and equity ratio (all periods) and the debt to asset ratio (in some study periods) were greater than the standard and the proprietors’ ratio (over all study periods) was below the standards showing that the union’s long term solvency was very poor. Keywords: 1. financial growth and performance 2. cooperative union 3. ratio analysis 4. trend analysis. GJMBR-D Classification: JEL Code: M40 EvaluationoftheFinancialGrowthandPerformanceofTepiCoffeeProducerFarmersCooperativesUnionShekaZoneSouthWestEthiopia Strictly as per the compliance and regulations of: © 2018. -

Characterization of Indigenous Chicken Production Systems in Sheka Zone, South Western Ethiopia Hailu Assefa*1, Aberra Melesse2 , Mestawet Taye2
International Journal For Research In Agricultural And Food Science ISSN: 2208-2719 Characterization of indigenous chicken production systems in Sheka zone, south western Ethiopia Hailu Assefa*1, Aberra Melesse2 , Mestawet Taye2 *1Mizan Agricultural Technical, Vocational, Educational and Training College, P.O. Box 217. Southern Nations Nationalities Regional State, Ethiopia 2 School of Animal and Range Sciences, Hawassa University, P.O. Box 5, Hawassa, Ethiopia *Corresponding author: E-mail: [email protected] Abstract The survey was conducted in Sheka Zone to characterize the production system of indigenous chicken populations. A mixture of purposive and random sampling techniques was used to collect the data. Data on chicken production system were assessed through semi-structured questionnaire survey. Households who rear only indigenous chicken were considered in this study. The findings revealed that the mean flock size in the study area was 13.2 per household. About 38.3 and 61.7% of respondents replaced their flock through buying from market and from hatched, respectively. The primary purpose of egg production in the study zone was for income generation (80.4%). The study indicated that indigenous chicken production system in study area is characterized by scavenging with seasonal feed supplemented system. The most common supplementary feed was Ensete ventricosum (processed enset) (64.9%) in the study zone. About 52.5% of respondents keep their chickens in a separate house while the rest (47.5%) used different types of night sheltering systems. Newcastle disease (40.5%) was the main devastating diseases reported by the households. The mean age at first egg laying for pullets and sexual maturity for cockerels was 6.3 and 5.6 months, respectively. -
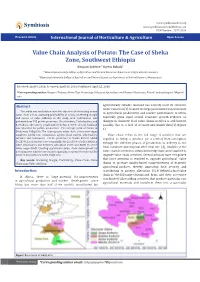
Value Chain Analysis of Potato: the Case of Sheka Zone, Southwest
Symbiosis www.symbiosisonline.org www.symbiosisonlinepublishing.com Research Article International Journal of Horticulture & Agriculture ISSN Number: Open 2572-3154 Access Value Chain Analysis of Potato: The Case of Sheka Zone, Southwest Ethiopia Benyam Tadesse1* Fayera Bakala2 1* Mizan-Tepi university, College of Agriculture and Natural Resources, department of Agricultural economics 2Mizan-Tepi University, College of Agriculture and Natural Resources, department of Natural Resource Management Received: April 9, 2018; Accepted: April 19, 2018; Published: April 25, 2018 *Corresponding author: Benyam Tadesse, Mizan-Tepi University, College of Agriculture and Natural Resources, E-mail: tadessebenyam7@gmail. com Abstract agriculturally suitable land and has scarcely used its extensive The study was undertaken with the objective of identifying potato water resources [1]. Despite the large potential for improvements value chain actors, assessing profitability of actors, marketing margin in agricultural productivity and market performance in Africa, and extent of value addition in the study area. Information was especially given rapid overall economic growth, evidence on wasgathered allocated from 193for potato potato production.producers, 7local The traders,average 7yield wholesalers, of Potato and in changes in domestic food value chains in Africa is still limited, 8 retailers. The survey result indicated that 27.94% of total farmland possibly due to a lack of accurate and reliable data [2].(Figure 1) Sheka was 108qt/ ha. The major potato -

Guide 2000 English.Pub
1 MAY 2008 AWASSA 2 Table of Contents Page N0 • Introduction 1 Part I Location and Administrative Division—- - - - - - - - - - - - - - 2 • Topography —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 2 • Climate —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - • Soil Resource —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 3 • Land use and land cover —- - - - - - - - - - - - - - - - - - - - - - - - - 3 • Water bodies —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - • Forest Resource —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 5 • Wild life resource —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 5 • Tourist Attraction and potential —- - - - - - - - - - - - - - - - - - - 6 • Population —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 7 • Ethnic Composition —- - - - - - - - - - - - - - - - - - - - - - - - - 8 • Urbanization —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 8 • Agriculture —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 8 • Livestock resource —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 9 • Fisher —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 9 • Hides and skins production and market —- - - - - - - - - - - - - - 9 • Apiculture —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 9 • Industry —- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 9 • Education—- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -

Assessment of Beekeeping Practices and Honey
Research Article Agri Res & Tech: Open Access J Volume 16 Issue 1 - May 2018 Copyright © All rights are reserved by Getachew Abraham DOI: 10.19080/ARTOAJ.2018.16.555974 Assessment on the Constraints & Practices of Beekeeping, and Post-Harvest Honey Handling in Gesha District, Keffa Zone, South-West Ethiopia Getachew Abraham* Department of Animal Science, College of Agriculture Science, Ethiopia Submission: April 07,2018; Published: May 11, 2018 *Corresponding author: Getachew Abraham, Department of Animal Science, College of Agriculture Science, Arba-Minch University, Ethiopia, Email: Abstract The study was conducted in Gesha district, Keffa zone, SNNPRS of Ethiopia to assess the current practices & constraints of beekeeping, and post-harvest honey handling. A total of 160 respondents’ were selected randomly from four purposively selected localities based on beekeeping potential & interviewed using semi structured questioner. Data were analyzed using SPSS version 21 software. The study revealed the majority of the respondents (60%) in the district practiced traditional beekeeping only. The average annual honey yield per hive from traditional beekeeping Pestobserved & honey significance bee enemies, difference herbicide (p>0.05) poisoning, for the absconding localities; of however bees, and from lack transitionalof appropriate & movableknowledge frame to manage hive, it bees observed were foundno significance the major difference. The average annual honey yields per hive from traditional, transitional & modern beehive were 8.62kg, 13.13kg