Current and Future Trends in Periodontal Tissue Engineering and Bone Regeneration
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal of Dental Research
Journal of Dental Research http://jdr.sagepub.com/ Cell Differentiation and Matrix Organization in Engineered Teeth A. Nait Lechguer, M.L. Couble, N. Labert, S. Kuchler-Bopp, L. Keller, H. Magloire, F. Bleicher and H. Lesot J DENT RES 2011 90: 583 originally published online 4 February 2011 DOI: 10.1177/0022034510391796 The online version of this article can be found at: http://jdr.sagepub.com/content/90/5/583 Published by: http://www.sagepublications.com On behalf of: International and American Associations for Dental Research Additional services and information for Journal of Dental Research can be found at: Email Alerts: http://jdr.sagepub.com/cgi/alerts Subscriptions: http://jdr.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - Apr 13, 2011 OnlineFirst Version of Record - Feb 4, 2011 What is This? Downloaded from jdr.sagepub.com at Service Commun de la Documentation Université de Strasbourg on September 6, 2013 For personal use only. No other uses without permission. © 2011 International & American Associations for Dental Research RESEARCH REPORTS Biomaterials & Bioengineering A. Nait Lechguer1,2, M.L. Couble3,4, N. Labert3,4, S. Kuchler-Bopp1,2, Cell Differentiation and L. Keller1,2, H. Magloire3,4, F. Bleicher3,4, Matrix Organization in and H. Lesot1,2* Engineered Teeth 1INSERM UMR 977, Faculté de Médecine, 11, rue Humann, F-67085 Strasbourg, France; 2Dental School, University of Strasbourg, Strasbourg, France; 3Université de Lyon, Faculté d’Odontologie, Rue Guillaume Paradin, F-69372 Lyon Cedex 08, France; and 4IGFL, CNRS UMR 5242, Ecole Normale Supérieure, 46 Allée d’Italie, 69364, Lyon Cedex 08, France; *corresponding author, [email protected] J Dent Res 90(5):583-589, 2011 ABSTRACT InTRODuCTIOn Embryonic dental cells were used to check a series of criteria to be achieved for tooth engineering. -

Lecture 2 – Bone
Oral Histology Summary Notes Enoch Ng Lecture 2 – Bone - Protection of brain, lungs, other internal organs - Structural support for heart, lungs, and marrow - Attachment sites for muscles - Mineral reservoir for calcium (99% of body’s) and phosphorous (85% of body’s) - Trap for dangerous minerals (ex:// lead) - Transduction of sound - Endocrine organ (osteocalcin regulates insulin signaling, glucose metabolism, and fat mass) Structure - Compact/Cortical o Diaphysis of long bone, “envelope” of cuboid bones (vertebrae) o 10% porosity, 70-80% calcified (4x mass of trabecular bone) o Protective, subject to bending/torsion/compressive forces o Has Haversian system structure - Trabecular/Cancellous o Metaphysis and epiphysis of long bone, cuboid bone o 3D branching lattice formed along areas of mechanical stress o 50-90% porosity, 15-25% calcified (1/4 mass of compact bone) o High surface area high cellular activity (has marrow) o Metabolic turnover 8x greater than cortical bone o Subject to compressive forces o Trabeculae lined with endosteum (contains osteoprogenitors, osteoblasts, osteoclasts) - Woven Bone o Immature/primitive, rapidly growing . Normally – embryos, newborns, fracture calluses, metaphyseal region of bone . Abnormally – tumors, osteogenesis imperfecta, Pagetic bone o Disorganized, no uniform orientation of collagen fibers, coarse fibers, cells randomly arranged, varying mineral content, isotropic mechanical behavior (behavior the same no matter direction of applied force) - Lamellar Bone o Mature bone, remodeling of woven -

Dental Cementum Reviewed: Development, Structure, Composition, Regeneration and Potential Functions
Braz J Oral Sci. January/March 2005 - Vol.4 - Number 12 Dental cementum reviewed: development, structure, composition, regeneration and potential functions Patricia Furtado Gonçalves 1 Enilson Antonio Sallum 1 Abstract Antonio Wilson Sallum 1 This article reviews developmental and structural characteristics of Márcio Zaffalon Casati 1 cementum, a unique avascular mineralized tissue covering the root Sérgio de Toledo 1 surface that forms the interface between root dentin and periodontal Francisco Humberto Nociti Junior 1 ligament. Besides describing the types of cementum and 1 Dept. of Prosthodontics and Periodontics, cementogenesis, attention is given to recent advances in scientific Division of Periodontics, School of Dentistry understanding of the molecular and cellular aspects of the formation at Piracicaba - UNICAMP, Piracicaba, São and regeneration of cementum. The understanding of the mechanisms Paulo, Brazil. involved in the dynamic of this tissue should allow for the development of new treatment strategies concerning the approach of the root surface affected by periodontal disease and periodontal regeneration techniques. Received for publication: October 01, 2004 Key Words: Accepted: December 17, 2004 dental cementum, review Correspondence to: Francisco H. Nociti Jr. Av. Limeira 901 - Caixa Postal: 052 - CEP: 13414-903 - Piracicaba - S.P. - Brazil Tel: ++ 55 19 34125298 Fax: ++ 55 19 3412 5218 E-mail: [email protected] 651 Braz J Oral Sci. 4(12): 651-658 Dental cementum reviewed: development, structure, composition, regeneration and potential functions Introduction junction (Figure 1). The areas and location of acellular Cementum is an avascular mineralized tissue covering the afibrillar cementum vary from tooth to tooth and along the entire root surface. Due to its intermediary position, forming cementoenamel junction of the same tooth6-9. -

Sclerostin in Oral Tissues: Distribution, Biological Functions and Potential Therapeutic Role
Review Article Open Access Journal of Review Article Biomedical Science ISSN: 2690-487X Sclerostin in Oral Tissues: Distribution, Biological Functions and Potential Therapeutic Role Fangyuan Shuai1, Aileen To2, Yan Jing3 and Xianglong Han1* 1State Key Laboratory of Oral Diseases, West China Hospital of Stomatology, Sichuan University, China 2Texas A&M College of Dentistry, D3 dental student, USA 3Texas A&M College of Dentistry, Department of Orthodontics, USA ABSTRACT Sclerostin is a well-known osteogenic negative regulator whose biological functions have been widely studied in bone homeostasis. Targeting sclerostin via monoclonal antibodies was shown to be a powerful strategy for bone-related diseases. Traditionally, to osteocytes, there are other cell types in oral tissues that can produce sclerostin. Sclerostin regulates the formation of dental andsclerostin periodontal was known structures as an and osteocyte-specific is also involved inglycoprotein. various physiological However, andin recent pathological studies, events it has in been oral showntissues. thatThus, in sclerostin addition modulation has been determined as a possible treatment strategy for periodontium-related diseases. To develop the therapeutic oral tissues. In this review, we highlight the existing awareness of sclerostin’s functions in oral tissues; the roles it plays in dental and periodontalpotential of sclerostindiseases and and treatments; its antibodies and in the the therapeutic field of dentistry, potential researchers of sclerostin must and clearly its antibodies -

A Global Compendium of Oral Health
A Global Compendium of Oral Health A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan This book first published 2019 Cambridge Scholars Publishing Lady Stephenson Library, Newcastle upon Tyne, NE6 2PA, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2019 by Morenike Oluwatoyin Folayan and contributors All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-5275-3691-2 ISBN (13): 978-1-5275-3691-3 TABLE OF CONTENTS Foreword .................................................................................................. viii Introduction ................................................................................................. 1 Dental Development: Anthropological Perspectives ................................. 31 Temitope A. Esan and Lynne A. Schepartz Belarus ....................................................................................................... 48 Natallia Shakavets, Alexander Yatzuk, Klavdia Gorbacheva and Nadezhda Chernyavskaya Bangladesh ............................................................................................... -

Developmental Biology of Cementum
Int. J. Dev. Biol. 45: 695-706 (2001) Review Developmental Biology of Cementum THOMAS G.H. DIEKWISCH* Allan G. Brodie Laboratory for Craniofacial Genetics, University of Illinois at Chicago, USA CONTENTS Origins of cementum - a scientific "whodunit" ........................................................................695 Loss of ameloblast continuity and insertion of mesenchymal cells from the dental follicle proper ................................................................................................697 Initial cementum matrix deposition by mesenchymal cells in proximity to non-secretory epithelial cells ...................................................................................699 Cementogenesis at the tooth cervix and at the cemento-enamel junction .............................700 Early removal of HERS from the root surface in humans as seen in the Gottlieb collection ..............................................................................................701 Role of amelogenins in cementogenesis ................................................................................702 Possible mechanism of cementoblast induction .....................................................................704 Summary ................................................................................................................................704 KEY WORDS: Cementum, Hertwig’s epithelial root sheath, Gottlieb, amelogenin, periodontium Tooth cementum is a bone-like mineralized tissue secreted by Origins of cementum - a scientific -

Endodontic Recommended Reading List 2018 A. ความรู้วิทยาศาสตร์พื้นฐาน 1
1 Endodontic Recommended Reading List 2018 A. ความรู้วิทยาศาสตร์พื้นฐาน 1. Gross, microscopic และ ultrastructural anatomy of soft and hard tissue (tooth and surrounding) 2. Embryology, histology, bone biology 3. Microbiology 4. Oral infection & immunology 5. Oral medicine, Oral pathology 6. Inflammation & healing 7. ชีวสถิติ 8. ความรู้กฎหมายวิชาชีพ เจตคติ และจรรยาบรรณแห่งวิชาชีพทันตกรรม B. วิทยาศาสตร์การแพทย์ที่เกี่ยวข้องกับสาขา 1. Embryology, histology, physiology of pulp and periapical tissue 2. Biology of dental pulp 1. Bennett CG, Kelln EE, Biddington WR. Age changes of the vascular pattern of the human dental pulp. Arch Oral Biol. 1965;10(6):995-8. 2. Bernick S. Effect of aging on the nerve supply to human teeth. J Dent Res. 1967;46(4):694- 9. 3. Bernick S. Lymphatic vessels of the human dental pulp. J Dent Res. 1977;56(1):70-7. 4. Brannstrom M. The hydrodynamic theory of dentinal pain: sensation in preparations, caries, and the dentinal crack syndrome. J Endod. 1986;12(10):453-7. 2 5. Brannstrom M, Linden LA, Johnson G. Movement of dentinal and pulpal fluid caused by clinical procedures. J Dent Res. 1968;47(5):679-82. 6. Byers MR, Neuhaus SJ, Gehrig JD. Dental sensory receptor structure in human teeth. Pain. 1982;13(3):221-35. 7. Carrigan PJ, Morse DR, Furst ML, Sinai IH. A scanning electron microscopic evaluation of human dentinal tubules according to age and location. J Endod. 1984;10(8):359-63. 8. DENTISTRY AAOP. Guideline on Pulp Therapy for Primary and Immature Permanent Teeth. Pediatr Dent. 2016;38(6):280-8. 9. Fitzgerald M, Chiego DJ, Jr., Heys DR. Autoradiographic analysis of odontoblast replacement following pulp exposure in primate teeth. -

Straumann® Emdogain® ENAMEL MATRIX DERIVATIVE
Product Information Biomaterials@Straumann® Because one option is not enough. Straumann® Emdogain® ENAMEL MATRIX DERIVATIVE 490.280_Emdogain-flyer-4-pager.indd 1 08/01/2018 16:49 Straumann® Emdogain® Emdogain® is a unique protein mix which influences Prof. Dr. David Cochran, a number of different cells and different processes. It Implantologist, « San Antonio/USA really helps the wound healing and wound closure in the oral cavity. « WHY USE STRAUMANN® EMDOGAIN®? Emdogain® induces true regeneration By modulating the wound healing process, Emdogain® induces the regeneration of a functional attachment in periodontal procedures (as evidenced by human histological data¹,²) Emdogain® improves wound healing By promoting angiogenesis³,⁴, modulating the production of factors in oral surgical procedures related to inflammation⁵ and thanks to its anti-microbial effect toward oral pathogens⁶, Emdogain® accelerates the wound healing process of oral surgical procedures⁷ Emdogain® increased the predictability Emdogain® leads to: of your periodontal procedures - significantly improved clinical parameters in intra-osseous defects compared to open flap debridement procedures alone⁸ - increased root coverage achieved when used in a coronally advanced flap (CAF) compared to CAF alone⁹, and leads to results comparable to CAF + Connective Tissue Graft¹⁰ Emdogain® helps you achieve patient - When used to treat intra-osseous defects, Emdogain® contributes satisfaction to improve your patients’ dental prognosis. - When used in oral surgical procedures in general, Emdogain® accelerates wound closure¹¹, and reduces post surgical pain and swelling¹². - When used in periodontal plastic procedures around teeth and implants, Emdogain® may improve the esthetics of the results thanks to improved wound healing. Emdogain® is easy to apply Because Emdogain® is a gel, it requires no trimming and is easy to apply, even in defects difficult to access. -

Biodental Engineering V
BIODENTAL ENGINEERING V PROCEEDINGS OF THE 5TH INTERNATIONAL CONFERENCE ON BIODENTAL ENGINEERING, PORTO, PORTUGAL, 22–23 JUNE 2018 Biodental Engineering V Editors J. Belinha Instituto Politécnico do Porto, Porto, Portugal R.M. Natal Jorge, J.C. Reis Campos, Mário A.P. Vaz & João Manuel R.S. Tavares Universidade do Porto, Porto, Portugal CRC Press/Balkema is an imprint of the Taylor & Francis Group, an informa business © 2019 Taylor & Francis Group, London, UK Typeset by V Publishing Solutions Pvt Ltd., Chennai, India All rights reserved. No part of this publication or the information contained herein may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, by photocopying, recording or otherwise, without written prior permission from the publisher. Although all care is taken to ensure integrity and the quality of this publication and the information herein, no responsibility is assumed by the publishers nor the author for any damage to the property or persons as a result of operation or use of this publication and/or the information contained herein. Library of Congress Cataloging-in-Publication Data Names: International Conference on Biodental Engineering (5th: 2018: Porto, Portugal), author. | Belinha, Jorge, editor. | Jorge, Renato M. Natal editor. | Campos, J.C. Reis, editor. | Vaz, Mario A.P., editor. | Tavares, Joao Manuel R.S., editor. Title: Biodental engineering V: proceedings of the 5th International Conference on Biodental Engineering, Porto, Portugal, 22–23 June 2018 / editors, J. Belinha, R.M. Natal Jorge, J.C. Reis Campos, Mario A.P. Vaz & Joao Manuel R.S. Tavares. Description: London, UK; Boca Raton, FL: Taylor & Francis Group, [2019] | Includes bibliographical references and index. -

Emdogain) and Subepithelial Connective Tissue Graft for Root Coverage in Patients with Multiple Gingival Recession Defects: a Randomized Controlled Clinical Study
QUINTESSENCE INTERNATIONAL PERIODONTOLOGY Angeliki Alexiou Comparison of enamel matrix derivative (Emdogain) and subepithelial connective tissue graft for root coverage in patients with multiple gingival recession defects: A randomized controlled clinical study Angeliki Alexiou, DDS, MSc1/Ioannis Vouros, Dr med dent2/Georgios Menexes, BMath, MA, PhD3/Antonis Konstantinidis, Prof DMD, MSc, PhD4 Objective: The purpose of the present study was to compare list. Data were analyzed within the frame of Mixed Linear the clinical efficiency of enamel matrix derivative (EMD) placed Models with the ANOVA method. Results: There were no sta- under a coronally advanced flap (CAF; test group), to a connec- tistically significantly differences observed between test and tive tissue graft (CTG) placed under a CAF (control group), in control groups in regards with the depth of buccal recession patients with multiple recession defects. Method and with a mean REC of 1.82 mm (CTG) and 1.72 mm (EMD) re- Materials: Twelve patients with multiple Miller’s Class I or II spectively. Similarly the mean PPD value was 1.3 mm for both gingival recessions in contralateral quadrants of the maxilla groups at T6, while the respective value for CAL was 1.7 mm were selected. The primary outcome variable was the change (EMD) and 1.8 mm (CTG). Statistically significant differences in depth of the buccal recession (REC), at 6 months (T6) after were observed only for the WKT, which were 3.0 mm and surgery. The secondary outcome parameters included the clin- 3.6 mm for the test and control groups respectively (P < .001) ical attachment level (CAL), the probing pocket depth (PPD), at T6. -
AIPET Syllabus for Periodontology – Paper – II
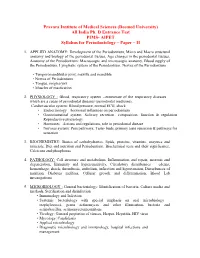
Pravara Institute of Medical Sciences (Deemed University) All India Ph. D Entrance Test PIMS- AIPET Syllabus for Periodontology – Paper – II 1. APPLIED ANATOMY: Development of the Periodontium, Micro and Macro structural anatomy and biology of the periodontal tissues, Age changes in the periodontal tissues, Anatomy of the Periodontium: Macroscopic and microscopic anatomy, Blood supply of the Periodontium, Lymphatic system of the Periodontium, Nerves of the Periodontium • Temporomandibular joint, maxilla and mandible • Nerves of Periodontium. • Tongue, oropharynx • Muscles of mastication 2. PHYSIOLOGY : Blood, respiratory system --enumerate of the respiratory diseases which are a cause of periodontal diseases (periodontal medicine), Cardiovascular system: Blood pressure, normal ECG, shock • Endocrinology—hormonal influences on periodontium • Gastrointestinal system: Salivary secretion—composition, function & regulation Reproductive physiology • Hormones –Actions and regulations, role in periodontal disease • Nervous system: Pain pathways, Taste- buds, primary taste sensation & pathways for sensation 3. BIOCHEMISTRY: Basics of carbohydrartes, lipids, proteins, vitamins, enzymes and minerals, Diet and nutrition and Periodontium, Biochemical tests and their significance, Calcicum and phosphorus 4. PATHOLOGY: Cell structure and metabolism, Inflammation and repair, necrosis and degeneration, Immunity and hypersensitivity, Circulatory disturbances – edema, hemorrhage, shock, thrombosis, embolism, infarction and hypertension, Disturbances of -

The Multiple Functions of Gingival and Mucoperiosteal Fibroblasts in Oral Wound Healing and Repair
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Bern Open Repository and Information System (BORIS) Chiquet et al. Review Periodontology 2000 11.10.2011 MCh, revised 27.01.2014 The multiple functions of gingival and mucoperiosteal fibroblasts in oral wound healing and repair Matthias Chiquet1, Christos Katsaros1, and Dimitris Kletsas2 Periodontol 2000. 2015 Jun;68(1):21-40. doi: 10.1111/prd.12076. Accepted Manuscript; Contributor's version The final version is available from http://onlinelibrary.wiley.com/ | downloaded: 13.3.2017 https://doi.org/10.7892/boris.76776 source: 1 Chiquet et al. Review Periodontology 2000 11.10.2011 MCh, revised 27.01.2014 The multiple functions of gingival and mucoperiosteal fibroblasts in oral wound healing and repair Matthias Chiquet1, Christos Katsaros1, and Dimitris Kletsas2 1Department of Orthodontics and Dentofacial Orthopedics, Dental School, University of Bern, Bern, Switzerland 2Laboratory of Cell Proliferation and Ageing, Institute of Biology, NCSR "Demokritos", Athens, Greece Correspondence: Professor Matthias Chiquet, Ph.D. Department of Orthodontics and Dentofacial Orthopedics School of Dental Medicine / Medical Faculty, University of Bern Freiburgstrasse 7 CH-3010 Bern, Switzerland Phone: +41-31-632-9882 Fax: +41-31-632-9869 e-Mail: [email protected] Running title: Fibroblasts in oral wound healing Monograph title: Wound healing in Periodontology and Implantology Guest Editors: Anton Sculean, Iain Chapple 2 Chiquet et al. Review Periodontology 2000 11.10.2011 MCh, revised 27.01.2014 Abstract Fibroblasts are cells of mesenchymal origin responsible for the production of most extracellular matrix in connective tissues, and are essential for wound healing and repair.