Managing the Presbyope
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prescription Companion
PRESCRIPTION COMPANION ©2012Transitions Optical inc. ophthalmic lens technical reference JUBILEE YEAR 2012 E -Edition 7 www.norville.co.uk Introduction and Page Index The Norville Companion is a supporting publication for our Prescription Catalogue, providing further technical details, hints and ideas gleaned from everyday experiences. TOPIC Page(s) TOPIC Page(s) Index 2 - 3 Part II Rx Allsorts Lens Shapes 4 - 6 Lens Forms 49 Effective Diameter Chart 7 Base Curves 50 - 51 Simplify Rx 8 Aspherics 52 - 53 Ophthalmic Resins 9 Free-form Digital Design 54 Indices of Ophthalmic lenses - Resin 10 Compensated Lens Powers 55 - 56 Polycarbonate 11 Intelligent Prism Thinning 57 - 58 Trivex 12 - 13 Superlenti - Glass 59 Resin Photochromic Lenses 14 Superlenti - Resin 60 Transitions Availability Check List 15 V Value / Fresnels 61 Nupolar Polarising Lenses 16 E Style Bifocal / Trifocal 62 Drivewear Lenses 17 - 18 Photochromic / Glazing / Prisms 63 UV Protective Lenses 19 Lens Measures 64 Norville PLS Tints 20 Sports 65 Tinted Resin Lenses 21 3D Technology Overview 66 Mid and High Index Resins Tintability 22 Rx Ordering 67 Norlite Tint Transmission Charts 23 - 25 Order Progress 68 Norlite Speciality Tinted Resins 26 - 31 Rx Order Form 69 Norlite Mirror Coating 32 Queries 70 Reflection Free Coating 33 - 34 Optical Heritage 71 F.A.Q. Reflection Free Coatings 35 - 37 Rx House - Change afoot? 72 - 73 Indices of Ophthalmic Lenses - Glass 38 Remote Edging 74 Glass Photochromic Lenses 38 Remote edging - F.A.Q. 75 Speciality Absorbing Glass 39 Quality Assurance -

The Eye Is a Natural Optical Tool
KEY CONCEPT The eye is a natural optical tool. BEFORE, you learned NOW, you will learn •Mirrors and lenses focus light • How the eye depends on to form images natural lenses •Mirrors and lenses can alter • How artificial lenses can be images in useful ways used to correct vision problems VOCABULARY EXPLORE Focusing Vision cornea p. 607 How does the eye focus an image? pupil p. 607 retina p. 607 PROCEDURE 1 Position yourself so you can see an object about 6 meters (20 feet) away. 2 Close one eye, hold up your index finger, and bring it as close to your open eye as you can while keeping the finger clearly in focus. 3 Keeping your finger in place, look just to the side at the more distant object and focus your eye on it. 4 Without looking away from the more distant object, observe your finger. WHAT DO YOU THINK? • How does the nearby object look when you are focusing on something distant? • What might be happening in your eye to cause this change in the nearby object? The eye gathers and focuses light. The eyes of human beings and many other animals are natural optical tools that process visible light. Eyes transmit light, refract light, and respond to different wavelengths of light. Eyes contain natural lenses that focus images of objects. Eyes convert the energy of light waves into signals that can be sent to the brain. The brain interprets these signals as shape, brightness, and color. Altogether, these processes make vision possible. In this section, you will learn how the eye works. -

Patient Instruction Guide
1‐DAY ACUVUE® MOIST Brand Contact Lenses 1‐DAY ACUVUE® MOIST Brand Contact Lenses for ASTIGMATISM 1‐DAY ACUVUE® MOIST Brand MULTIFOCAL Contact Lenses etafilcon A Soft (hydrophilic) Contact Lenses Visibility Tinted with UV Blocker for Daily Disposable Wear PATIENT INSTRUCTION GUIDE CAUTION: U.S. Federal law restricts this device to sale by or on the order of a licensed practitioner. 1 TABLE OF CONTENTS TABLE OF CONTENTS ............................................................................................................................................... 2 INTRODUCTION ....................................................................................................................................................... 3 SYMBOLS KEY .......................................................................................................................................................... 4 UNDERSTANDING YOUR PRESCRIPTION ................................................................................................................. 5 GLOSSARY OF COMMONLY USED TERMS ............................................................................................................... 5 WEARING RESTRICTIONS & INDICATIONS ............................................................................................................... 6 WHEN LENSES SHOULD NOT BE WORN (CONTRAINDICATIONS) ............................................................................ 6 WARNINGS ............................................................................................................................................................. -
Intraocular Lenses and Spectacle Correction
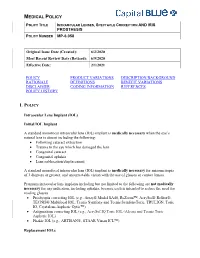
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

Eye Tester's Manual
EYE TESTER’S MANUAL Before using your vision (eye) tester GnomE read this manual carefully to ensure correct use. 1. GENERAL INSTRUCTIONS The home Eye Tester GnomE (or Tester) is a compact, autonomous optical instrument protected by the patent of Russian Federation No. 2202937. The main function of the Tester is to quickly check the parameters of the vision on your own at home or at working place. The Tester can be used in room conditions: - ambient temperature from +10 C to +35 C; average humidity at ambient temperature +25 C from 30% to 80% Absolute measurement accuracy is 0.25 diopter. Dimensions: 14 mm in diameter and 75 mm long Weight (without a case) up to 20g As the Tester is used in proximity to eyes take care of your movements. The Tester is made from safe materials (glass and metals). Please, avoid strong impacts caused by bumping or dropping the tester. The Tester imitates the operation of different kinds of glasses when eye watches remote objects. MEASURING PARAMETERS OF VISION. Checking near- and farsightedness Sit down and make yourself comfortable, take off your glasses or contact lens and hold that part of the Tester where the objective is with your hand (see photo). Look inside the tester through a lens with a checking eye, and read minimal and maximal digits at the scale. The scale looks like a watch, where 12 o’clock corresponds to zero on the scale and normal vision. There are negative values to the left from zero, and positive numbers to the right on the scale too. -
Contact Lenses
Buying Contact Lenses Some common Questions and Answers to help you buy your lenses safely Wearing contact lenses offers many benefits. Following some simple precautions when buying lenses can help to make sure that you don’t put the health and comfort of your eyes at risk. The British Contact Lens Association and General Optical Council have put together some common questions and answers to help you buy your lenses safely 2 Images courtesy of College of Optometrists, General Optical Council and Optician How do I find out about wearing contact lenses? ● If you want to wear contact lenses to correct your eyesight, you must start by consulting an eye care practitioner for a fitting. Only registered optometrists, dispensing opticians with a specialist qualification (contact lens opticians) and medical practitioners can fit contact lenses. Fitting includes discussing your visual and lifestyle requirements, an eye examination to make sure your eyes are healthy and find out if you’re suitable, and measurements of your eyes to ensure the best lens type, fit and vision, before trying lenses. Once you have worn the lenses, you should have the health of your eyes checked again. You will also need to learn how to handle and care for your lenses. Your practitioner will advise you when you should wear the lenses and how often you should replace them. When is the fitting completed? ● Your prescribing practitioner will tell you when the fitting is completed. How long the fitting takes will depend on your lens type and your eye health. Don’t forget that, once fitted, you will need to have regular check-ups to make sure your eyes are healthy and to get the best from your contact lenses. -

Field Review: FIT Close up Lenses. by Alex Mustard
Field Review: FIT Close Up Lenses. By Alex Mustard Supermacro images are will give me the magnification while commonly defined as pictures shot minimising the drawbacks of any at magnifications of greater than 1:1 single accessory. Typically, I favour (Left) The FIT +5 dioptre: achromatic, dual element and 67mm threaded. (real life versus actual size on your adding a teleconverter behind my SLR (Right) The achromatic, dual element FIT +8 dioptre, is smaller but comes with sensor). Since most of the popular lens and dioptre to the front of it. a step up ring to 67mm. There was not cut off from the filter with my 105mm lens macro lenses will take us down to This article is a review of the when used singly or stacked with the +5. 1:1, we need an accessory to become newly released FIT dual element, super. There are many, many methods achromatic dioptre lenses, sold in for achieving supermacro, indeed (out of the water) strengths of +5 and I have often joked that I want to +8. External dioptres have always write an instructional underwater been popular underwater because photography book called “101 Ways they can be added and removed To Supermacro”, with a century and underwater. While many value this one photos each taken with a different feature – it has never been that kit configurations. important for me because I believe In simple terms there are that the best underwater images tend 5 types of accessories that we to be taken when dives are dedicated regularly use to transform our macro in the pursuit of a particular type of lenses to super-status underwater: images. -
Automated Refraction Toolkit
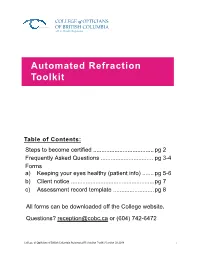
COLLEGE of OPTICIANS OF BRITISH COLUMBIA a B.C. Health Regulator Automated Refraction Toolkit Table of Contents: Steps to become certified ..................................... pg 2 Frequently Asked Questions ................................ pg 3-4 Forms a) Keeping your eyes healthy (patient info) ....... pg 5-6 b) Client notice ................................................... pg 7 c) Assessment record template ......................... pg 8 All forms can be downloaded off the College website. Questions? [email protected] or (604) 742-6472 College of Opticians of British Columbia Automated Refraction Toolkit Version 02.2018 "1 Steps to become a certified automated refracting optician The College has established high qualifications, professional standards and strict guidelines around independent automated refraction to safeguard public safety. Only certified opticians who are trained to safely and e fectively perform automated refraction are legally permitted to assess visual acuity. Opticians who are not certified in automated refraction cannot perform this service. To become certified to conduct independent automated refractions, opticians must complete the following steps: 1) Approved certification program 2) Jurisprudence examination 3) Certification application form and fees Approved certification program The following programs are approved by the College, under terms and conditions established by the Board and with the terms ending on the dates indicated, as meeting the standards of academic or technical achievement required for -

Comparative Analysis of Cosmetic Contact Lens Fitting By
Report of the Staff to the Federal Trade Commission A Comparative ~alysis of Cosmetic Coritact Lens Fitting by Ophtha1ffiologists, Optometrists, and Opticians .,... ... ---. ) by . Gary D. Hailey· Jonathan R. Bromberg Joseph P. Mulholland (Note: This report has been prepared by staff members of the Bureau of Consumer Protection and Bureau of Economics of the Federal Trade Commission. The Commission has reviewed the report and authorized its publication.) Acknowledgements The authors owe an enormous debt of gratitude to the many ophthalmologists, optometrists, and opticians wh~ assisted in the design and performance of this study out of a sense of responsi bility to their professions and to the public. Not all of them can be listed here. &ut the following individuals, who repre-. sen ted their respective professions at all stages of th~ study,' deserve special mention: Oliver H. Dabezies, Jr;, M.D., of the' Contact Lens Association of Ophthalmology and the American Academy of Ophthalmology; Earle L. Hunter, O.D., of the American Optometric Association; and Frank B. Sanning and Joseph W. Soper, of the Contact Lens Society of America and the Opticians Associa tion of America. Of course, none of these individuals or asso ciations necessarily endorses the ultimate conclusions of this report. A number ,of current and former FTC staff members have con tr ibuted to the study in important ways.· "'''Me-iribers of the Bureau of Consumer Protection's Impact Evaluation Unit, including Tom Maronick, Sandy Gleason,' Ron Stiff, Michael Sesnowitz, and Ken Bernhardt, helped answer innumerable technical questions related to the design and administration of the study. Christine Latsey, Elizabeth Hilder, Janis Klurfeld, Scott Klurfeld, Erica Summers, Matthew Daynard, Te~ry Latanich, and Gail Jensen interviewed study subjects, supervised the field examinat~ons, prepared data for analysis, wrote preliminary drafts, and helped with a number 6f 6ther ~asks. -

LENS EFFICIENCY-A CLINICAL CONCEPT*T the Accommodation
Br J Ophthalmol: first published as 10.1136/bjo.30.5.291 on 1 May 1946. Downloaded from LENS EFFICIENCY 291 LENS EFFICIENCY-A CLINICAL CONCEPT*t BY JOSEPH I. PASCAL NEW YORK THE fact tllat a lens has a different effectivity depending upon its position before the eye is well known. We say a convex lens gains in effectivity when moved away from the eye and loses in effect- ivity when moved closer to the eye. A concave lens behaves in just the opposite way. There is, however, another feature of changes in lens power which is not dependent upon movement farther from or nearer to the eye. This variable lens effect may be -called its "efficiency," which may be of an ascending order, termed positive efficiency or of a- descending order termed negative efficiency. A similar gradation of efficiency may be postulated with r8ference to the accommodation. It is well known that if a natural emmetrope, an uncorrected hypermetrope and an uncorrected myope each accommodate the same amount, they are not all focused for the same distance. But this is also true, though to a less extent, for the corrected hyperme- copyright. trope and the corrected myope. The prevalent idea that the cor- rected hypermetrope and the corrected myope accommodate 10 D. for one metre, 20 D. for 1/2 mm. and so on is not correct. For example, the natural emmetrope accommodating 3 0 D. is focused for 333 mm. from the eye. But the 2 0 D. corrected hyper- metrope and the 2-0 D. corrected myope when accommodating http://bjo.bmj.com/ 3 0- dioptres are focused for 360 mm. -

Asmofilcon a (40% Water) for 2 Week Or 1 Month Replacement Contact Lens
en Instructions for Use: asmofilcon A (40% water) for 2 week or 1 month replacement contact lens Important • Read the following instructions carefully before use and keep this document in a safe place for future reference. • Always follow the instructions in this document and those of your eye care professional or practitioner for appropriate use of contact lenses and lens care products including lens cases. FoR 2 week ReplAcement contAct lens Introduction asmofilcon A (40% water) is a blue tinted soft silicone hydrogel contact lens with 40% water content. The sterile asmofilcon A (40% water) is individually packaged in a foil-sealed plastic container and immersed in buffered saline solution. Indications asmofilcon A (40% water) is intended for daily or up to 7 days extended wear and correction of refractive ametropia (myopia, hyperopia and/or astigmatism) in non-aphakic disease-free eyes. wearing restrictions Clean and disinfect the contact lenses after lens removal using the cleaning and disinfecting regimen recommended by your eye care professional or practitioner. Replace the contact lenses every 2 weeks with fresh lenses. Be sure to consult your eye care professional or practitioner for the lens wearing schedule based on your individual needs. Always dispose of the contact lenses after the instructed wearing period. Wearing the contact lenses beyond the instructed wearing period increases the risk of eye problems. FoR 1 month ReplAcement contAct lens Introduction asmofilcon A (40% water) is a blue or lavender tinted soft silicone hydrogel contact lens with 40% water content. The sterile asmofilcon A (40% water) is individually packaged in a foil-sealed plastic container and immersed in buffered saline solution. -

Essential Contact Lens Practice
Contact Lens Monthly CET Essential contact lens practice Part 8 — Managing the presbyope Practitioners can expect a rise in presbyopic patients attending for contact lens fitting over the next few years. Jane Veys, John Meyler and Ian Davies continue their series by outlining the options and techniques available to correct presbyopia with contact lenses. C7603, three contact lens points suitable for optometrists, DOs and CLOs s the number of patients the same category as the presbyopic KEY POINTS wearing contact lenses emmetrope. The advantage of this around the world grows, technique is that the contact lens correc- ● The number of presbyopic patients so does the number requir- tion requires no modifications which, requiring contact lens correction is ing presbyopic correction. assuming that it is optimum at the time increasing and is predicted to continue AMany patients fitted with lenses are now of fitting, remains the case. to do so over the next five years ● In fitting the presbyope, the beginning to experience presbyopia and The obvious disadvantage is, of course, practitioner should have access to demand satisfactory correction without that the principal reason for contact lens a number of different lens designs recourse to spectacles. wear is being ignored. Contact lens and be aware of alternative fitting There is also the demand from presby- patients do not want to wear spectacles, approaches opic hyperopes who, on reaching presby- because, if they did, they would be doing ● The availability of single use opia, now need full-time correction for so already. Consequently pure contact disposable trial lenses allows distance and near and, with more active lens options should be explained first ease of trial for both patients and lifestyles and increased awareness of to the presbyopic contact lens wearers practitioners contact lenses, are asking for contact followed by spectacle correction option ● Lens power adjustments should lens correction.