Intraocular Lens Power Calculation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eye Tester's Manual
EYE TESTER’S MANUAL Before using your vision (eye) tester GnomE read this manual carefully to ensure correct use. 1. GENERAL INSTRUCTIONS The home Eye Tester GnomE (or Tester) is a compact, autonomous optical instrument protected by the patent of Russian Federation No. 2202937. The main function of the Tester is to quickly check the parameters of the vision on your own at home or at working place. The Tester can be used in room conditions: - ambient temperature from +10 C to +35 C; average humidity at ambient temperature +25 C from 30% to 80% Absolute measurement accuracy is 0.25 diopter. Dimensions: 14 mm in diameter and 75 mm long Weight (without a case) up to 20g As the Tester is used in proximity to eyes take care of your movements. The Tester is made from safe materials (glass and metals). Please, avoid strong impacts caused by bumping or dropping the tester. The Tester imitates the operation of different kinds of glasses when eye watches remote objects. MEASURING PARAMETERS OF VISION. Checking near- and farsightedness Sit down and make yourself comfortable, take off your glasses or contact lens and hold that part of the Tester where the objective is with your hand (see photo). Look inside the tester through a lens with a checking eye, and read minimal and maximal digits at the scale. The scale looks like a watch, where 12 o’clock corresponds to zero on the scale and normal vision. There are negative values to the left from zero, and positive numbers to the right on the scale too. -

Field Review: FIT Close up Lenses. by Alex Mustard
Field Review: FIT Close Up Lenses. By Alex Mustard Supermacro images are will give me the magnification while commonly defined as pictures shot minimising the drawbacks of any at magnifications of greater than 1:1 single accessory. Typically, I favour (Left) The FIT +5 dioptre: achromatic, dual element and 67mm threaded. (real life versus actual size on your adding a teleconverter behind my SLR (Right) The achromatic, dual element FIT +8 dioptre, is smaller but comes with sensor). Since most of the popular lens and dioptre to the front of it. a step up ring to 67mm. There was not cut off from the filter with my 105mm lens macro lenses will take us down to This article is a review of the when used singly or stacked with the +5. 1:1, we need an accessory to become newly released FIT dual element, super. There are many, many methods achromatic dioptre lenses, sold in for achieving supermacro, indeed (out of the water) strengths of +5 and I have often joked that I want to +8. External dioptres have always write an instructional underwater been popular underwater because photography book called “101 Ways they can be added and removed To Supermacro”, with a century and underwater. While many value this one photos each taken with a different feature – it has never been that kit configurations. important for me because I believe In simple terms there are that the best underwater images tend 5 types of accessories that we to be taken when dives are dedicated regularly use to transform our macro in the pursuit of a particular type of lenses to super-status underwater: images. -
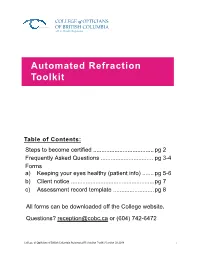
Automated Refraction Toolkit
COLLEGE of OPTICIANS OF BRITISH COLUMBIA a B.C. Health Regulator Automated Refraction Toolkit Table of Contents: Steps to become certified ..................................... pg 2 Frequently Asked Questions ................................ pg 3-4 Forms a) Keeping your eyes healthy (patient info) ....... pg 5-6 b) Client notice ................................................... pg 7 c) Assessment record template ......................... pg 8 All forms can be downloaded off the College website. Questions? [email protected] or (604) 742-6472 College of Opticians of British Columbia Automated Refraction Toolkit Version 02.2018 "1 Steps to become a certified automated refracting optician The College has established high qualifications, professional standards and strict guidelines around independent automated refraction to safeguard public safety. Only certified opticians who are trained to safely and e fectively perform automated refraction are legally permitted to assess visual acuity. Opticians who are not certified in automated refraction cannot perform this service. To become certified to conduct independent automated refractions, opticians must complete the following steps: 1) Approved certification program 2) Jurisprudence examination 3) Certification application form and fees Approved certification program The following programs are approved by the College, under terms and conditions established by the Board and with the terms ending on the dates indicated, as meeting the standards of academic or technical achievement required for -

LENS EFFICIENCY-A CLINICAL CONCEPT*T the Accommodation
Br J Ophthalmol: first published as 10.1136/bjo.30.5.291 on 1 May 1946. Downloaded from LENS EFFICIENCY 291 LENS EFFICIENCY-A CLINICAL CONCEPT*t BY JOSEPH I. PASCAL NEW YORK THE fact tllat a lens has a different effectivity depending upon its position before the eye is well known. We say a convex lens gains in effectivity when moved away from the eye and loses in effect- ivity when moved closer to the eye. A concave lens behaves in just the opposite way. There is, however, another feature of changes in lens power which is not dependent upon movement farther from or nearer to the eye. This variable lens effect may be -called its "efficiency," which may be of an ascending order, termed positive efficiency or of a- descending order termed negative efficiency. A similar gradation of efficiency may be postulated with r8ference to the accommodation. It is well known that if a natural emmetrope, an uncorrected hypermetrope and an uncorrected myope each accommodate the same amount, they are not all focused for the same distance. But this is also true, though to a less extent, for the corrected hyperme- copyright. trope and the corrected myope. The prevalent idea that the cor- rected hypermetrope and the corrected myope accommodate 10 D. for one metre, 20 D. for 1/2 mm. and so on is not correct. For example, the natural emmetrope accommodating 3 0 D. is focused for 333 mm. from the eye. But the 2 0 D. corrected hyper- metrope and the 2-0 D. corrected myope when accommodating http://bjo.bmj.com/ 3 0- dioptres are focused for 360 mm. -

Asmofilcon a (40% Water) for 2 Week Or 1 Month Replacement Contact Lens
en Instructions for Use: asmofilcon A (40% water) for 2 week or 1 month replacement contact lens Important • Read the following instructions carefully before use and keep this document in a safe place for future reference. • Always follow the instructions in this document and those of your eye care professional or practitioner for appropriate use of contact lenses and lens care products including lens cases. FoR 2 week ReplAcement contAct lens Introduction asmofilcon A (40% water) is a blue tinted soft silicone hydrogel contact lens with 40% water content. The sterile asmofilcon A (40% water) is individually packaged in a foil-sealed plastic container and immersed in buffered saline solution. Indications asmofilcon A (40% water) is intended for daily or up to 7 days extended wear and correction of refractive ametropia (myopia, hyperopia and/or astigmatism) in non-aphakic disease-free eyes. wearing restrictions Clean and disinfect the contact lenses after lens removal using the cleaning and disinfecting regimen recommended by your eye care professional or practitioner. Replace the contact lenses every 2 weeks with fresh lenses. Be sure to consult your eye care professional or practitioner for the lens wearing schedule based on your individual needs. Always dispose of the contact lenses after the instructed wearing period. Wearing the contact lenses beyond the instructed wearing period increases the risk of eye problems. FoR 1 month ReplAcement contAct lens Introduction asmofilcon A (40% water) is a blue or lavender tinted soft silicone hydrogel contact lens with 40% water content. The sterile asmofilcon A (40% water) is individually packaged in a foil-sealed plastic container and immersed in buffered saline solution. -

Essential Contact Lens Practice
Contact Lens Monthly CET Essential contact lens practice Part 8 — Managing the presbyope Practitioners can expect a rise in presbyopic patients attending for contact lens fitting over the next few years. Jane Veys, John Meyler and Ian Davies continue their series by outlining the options and techniques available to correct presbyopia with contact lenses. C7603, three contact lens points suitable for optometrists, DOs and CLOs s the number of patients the same category as the presbyopic KEY POINTS wearing contact lenses emmetrope. The advantage of this around the world grows, technique is that the contact lens correc- ● The number of presbyopic patients so does the number requir- tion requires no modifications which, requiring contact lens correction is ing presbyopic correction. assuming that it is optimum at the time increasing and is predicted to continue AMany patients fitted with lenses are now of fitting, remains the case. to do so over the next five years ● In fitting the presbyope, the beginning to experience presbyopia and The obvious disadvantage is, of course, practitioner should have access to demand satisfactory correction without that the principal reason for contact lens a number of different lens designs recourse to spectacles. wear is being ignored. Contact lens and be aware of alternative fitting There is also the demand from presby- patients do not want to wear spectacles, approaches opic hyperopes who, on reaching presby- because, if they did, they would be doing ● The availability of single use opia, now need full-time correction for so already. Consequently pure contact disposable trial lenses allows distance and near and, with more active lens options should be explained first ease of trial for both patients and lifestyles and increased awareness of to the presbyopic contact lens wearers practitioners contact lenses, are asking for contact followed by spectacle correction option ● Lens power adjustments should lens correction. -

Topical Atropine in Retarding Myopia Progression and Axial Length Growth in Children with Myopia
| Original | Article | Topical atropine in retarding myopia progression and axial length growth in children with myopia Abdur Rahman Mohammad Alam, Md. Sanwar Hossain and Md. Shafiqul Islam Article Info Abstract Department of Ophthalmology, Faculty This study was conducted to observe the effect of atropine in retarding myopia progression and of Surgery, Bangabandhu Sheikh Mujib axial length growth in 36 myopic children (atropine group, 24; control, 12). The initial spherical Medical University, Shahbag, Dhaka, equivalent of the atropine group and control group was -3.0 ± 1.6 dioptre and -3.5 ± 1.6 dioptre Bangladesh respectively. At the 12th month in atropine group, it was -2.9 ± 2.6 dioptre and -4.6 ± 1.9 dioptre in For Correspondence: the control group. The power of the atropine group reduced but rose in the control group after 12 Abdur Rahman Mohammad Alam months. There was a statistically significant difference in final refractive errors between the two [email protected] groups (p<0.05). The initial axial length of the atropine group and control group was 24.3± 1.0 mm Received: 18 July 2020 and 24.6 ± 1.1 mm respectively. In 12th month, the changes in axial length in the two groups was Accepted: 28 November 2020 insignificant. However, the mean axial length progression at 12 months of the atropine group was Available Online: 1 December 2020 -0.1 ± 0.1 mm and it was lower than the control group which was -0.2 ± 0.2 mm, and this was statistically significant (p<0.05). In conclusion, topical atropine (0.01%) retarded myopia progre- ISSN: 2224-7750 (Online) ssion and axial length growth in myopic children. -

Analysis of Accommodation Capacity in Presbyopic Patients with Low Body Mass Index
294ARTIGO ORIGINAL Análise da capacidade de acomodação em pacientes présbitas com baixo índice de massa corporal Analysis of accommodation capacity in presbyopic patients with low body mass index Nadyr Antonia Damasceno1, Eduardo de França Damasceno2 RESUMO Objetivo: Correlacionar o índice de massa corporal com condição de baixo peso como possível fator de influência sobre a presbiopia. Métodos: Estudo transversal envolvendo 1030 pacientes com acuidade visual de 20/20 emétropes, com faixa etária entre 36-40 anos, 51-55 anos e 60-65 anos, sendo excluídos pacientes com cover testes positivo, anisometrópicos, com insuficiência de convergência ou alta correlação de convergência / acomodação. Avaliação do índice de massa corpórea de todos os pacientes, como variável pesquisada de presença ou ausência de baixo índice de massa corporal. Resultados: Não houve diferenças estatísticas significativas entre baixo peso e pesos maiores, quando se comparam os dois grupos em relação ao sexo e faixa etária. Houve significância estatística quando se correlacionou indivíduos de baixo peso corporal (IMC < 18,5) e menor expressão de presbiopia em indivíduos com faixa etária entre 51- 55 anos e na faixa etária entre 60-65 anos. Conclusão: Conforme demonstrado pela análise estatística há uma correlação significativa entre baixo peso corporal definido como índice de massa corporal abaixo de 18,5 e menor incidência de presbiopia ou retardo de sua instalação e evolução com a idade. Descritores: Presbiopia; Baixo peso corporal; Índice de massa corporal ABSTRACT Purpuse: To determine the correlation between presbyopia and body mass index. Methods: Cross-sectional study involving 1030 patients with visual acuity of 20/20 emmetropy, aged between 36-40 years, 51-55 years and 60-65 years, excluding patients with positive test cover, anisometropy with convergence insufficiency or high correlation convergence / accommodation. -

Managing the Presbyope
Essential Contact Lens Practice Managing the Presbyope As the number of patients wearing contact KEY POINTS lenses around the world grows, so does the The number of presbyopic patients requiring contact lens number requiring presbyopic correction. Many correction is increasing and is predicted to continue to patients fitted with lenses are now beginning to do so over the next five years KEY POINTS experience presbyopia and demand satisfactory In fitting the presbyope, the practitioner should correction without recourse to spectacles. have access to a number of different lens designs and be aware of alternative There is also the demand from presbyopic fitting approaches hyperopes who, on reaching presbyopia, now The availability of single use need full-time correction for distance and disposable trial lenses allows ease of trial for both patients near and, with more active lifestyles and and practitioners increased awareness of contact lenses, are Lens power adjustments should not be based on asking for contact lens correction. The number objective visual acuity alone of presbyopic patients in Europe is on a steady Subjective visual performance assessment is most effectively incline and is forecast to grow further over the achieved by experiencing lens wear in both the work and next five years. Practitioners can therefore home environment expect to see an increase in the number of There is a significant untapped opportunity for contact lens presbyopes attending for contact lens fittings correction of presbyopes over the next few years. 91 Managing the Presbyope s the size of the presbyopic market increases, so too does the number of options of correcting presbyopia with A contact lenses. -
Focus Group Session on Contact Lens
Focus Group Session on Contact Lens 9 September 2014 Agnes Goh Regulatory Specialist 1 All Rights Reserved Health Sciences Authority. Not to be reproduced without permission. Overview • Contact lens listing guidelines – SMDR Device Name & Model Information • Contact lens – Proposed grouping criteria – For feedback • Contact lens labelling requirements – Label content – Supply of IFU – Supply of fitting guides and brochures • Other Updates 2 All Rights Reserved Health Sciences Authority. Not to be reproduced without permission. CONTACT LENS LISTING GUIDELINES 3 All Rights Reserved Health Sciences Authority. Not to be reproduced without permission. SMDR Device Name Information • <Product owner name><Brand name as per label> 4 All Rights Reserved Health Sciences Authority. Not to be reproduced without permission. SMDR Model Information Scenario 1: Common identifier available for a range of dioptres Brief description Name as per Device Label Identifier of item <Common identifier> <replacement <Name per label>, <dioptre <individual colour, if schedule> range>, <other parameters e.g. applicable> <material> cylinder power, if applicable>, <range of pack size> MAGIC COLOR Xtra (-6.00D to - daily disposable, 0.25D, +0.25D to +6.00D) (pack Z150 (Starry yellow) Nelfilcon A of 6,12) MAGIC COLOR Xtra (-6.00D to - daily disposable, 0.25D, +0.25D to +6.00D) (pack Z250 (Deep purple) Nelfilcon A of 6,12) 5 All Rights Reserved Health Sciences Authority. Not to be reproduced without permission. SMDR Model Information Scenario 2: No unique identifier i.e. only brand name Clear Contact Lens Brief description Name as per Device Label Identifier of item <replacement <Name per label>, <dioptre <Name per label> schedule> range>, <other parameters e.g. -

Truly Accommodating Iols Set the Trend for Presbyopia Correction Refractive Refractive
Lens Truly accommodating IOLs set the trend for presbyopia correction Refractive Refractive Samuel Masket Courtesy of Samuel Masket MD 2006 ASCRS survey reveals that greater than 200,000 presbyopic USFDA data for ReSTOR IOL indicates very high levels of patient satisfaction Postoperative changes in the lens capsule bag, specifically fibrometaplasia may influence IOL’s were implanted in the US results with accommodating IOLs. Currently, sealed capsule irrigation, from Maloof, is the only available strategy; however it is used infrequently Stefanie Petrou Binder MD ensues and patients with increasing cylinder through the hard ring, leading to bulging and by multifocality or increased focus depth, in Nürnberg become much more susceptible to blurred a simulation of accommodation. rather than lens movement or shape change, vision, he said. A recent study on 10 eyes with advanced he said. In fact, the use of presbyopic IOLs TRULY accommodating, physiologic IOLs The Synchrony IOL is comprised of two macular degeneration revealed improved according to an ASCRS learning survey with fewer optical side effects are the hope lenses: an anterior +32D optic and a variable UCVA with the NuLens. Nonetheless, showed that US ASCRS members implanted for the future in presbyopia correction, as posterior minus optic. It has spring-like patient satisfaction remains to be seen, due 216,000 IOLs, of which 62 per cent were compared with pseudo-accommodating haptics to store energy for forward and to an ‘opposite accommodation’ effect noted ReSTOR lenses, 28 per cent ReZOOM, and IOLs, said Samuel Masket MD during his backward motion.The principle behind the with these lenses.This manifests as silicone 10 per cent Crystalens. -

Our Eyes in a Digital Era
Our eyes in a digital era Challenges and opportunities for practitioners Dr. Willis C Maples Geraint Griffiths Prof. Gunta Krumina USA United Kingdom Latvia Doctor Willis Clem Maples is currently in practice Geraint Griffiths is an independent optometrist Professor Gunta Krumina is the head of the Department Content at Bellevue Specialty Eye Clinic in Hattiesburg, and owner of Optical3 Opticians. He is the of Optometry and Vision Science at University of Latvia Mississippi (USA) in a practice limited to vision managing director of Sportsvision UK, chair in Riga, director of the optometry bachelor’s programme development and visual rehabilitation issues. of The Association of Sport and Schoolvision and a senior researcher-project leader. She was awarded a In addition to his Doctor of Optometry (OD) Willis Practitioners and author of the Diplomas PhD in medical physics for her research on the correlation Clem Maples has a Master’s in Community Health. in Sport and Schoolvision Practice. He is an between stereothreshold and quality of monocular stimuli. He is a Fellow of the American Academy of Optometry examiner for the College of Optometrists Her main research topics are related to stereovision, visual and he practised privately for 12 years before being and a sportvision expert for the British electrophysiology and clinical optometry. recruited to begin the vision therapy programme at Standards Institute (BSI). He believes that Her latest scientific work has focused on the visual screening the Oklahoma College of Optometry at Northeastern the understanding and management of the of schoolchildren and the visual fatigue of computer users. Introduction 4 State University.